Profile of Patients with a Combination of Sleep Apnea Syndrome and Heart Failure
Kadiri S and Salama A*
Department of Cardiology, Dreux Hospital, France
Received Date: 16/02/2023; Published Date: 26/04/2023
*Corresponding author: Kadiri Sara, Department of Cardiology, Dreux Hospital, 28 100 Dreux, France
Summary
Background: the sleep apnea syndrome is a factor contributing to the impairment of ventricular function and thus worsening of heart failure, which justifies its screening in this disease.
Aims: The aim of our study was to determine the profile of patients with syndrome association of sleep apnea - heart failure.
Methods: This is a descriptive retrospective study over a period of 2 years (November 2019- December 2021), performed in 42 patients with sleep apnea syndrome with at least one relapse of heart failure.
Results: There’s a majority of men (61.9 %) with a mean age of 66 years. A statistically significant prevalence of obstructive SAS (66.67%), followed by mixed SAS (14.29%) and central SAS (11.9%). Factors such as, hypertension (71.43%), dyslipidemia (73.81%) and obesity (40.48%), were associated with sleep apnea syndrome in a statistically significant way.
We also noted a correlation between the association of sleep apnea syndrome - heart failure and dilated left atrium (42.86%), atrial fibrillation (47.62%) and mitral profile type III (38.10%). Heart failure with preserved ejection fraction predominates in our patients (88.10%). Pulmonary hypertension is a poor prognostic factor. Hypertensive heart disease is the major cause. The sleep apnea syndrome central type seems to be linked to the development of systolic heart failure and mitral profile type III. In contrast, the mixed type apnea syndrome is associated with heart failure with preserved ejection and mitral profile type II.
Conclusions: Factors such as obesity, hypertension, dyslipidemia, atrial fibrillation, dilatation of the left atrium and the restrictive mitral flow are closely correlated with the syndrome association of sleep apnea - heart failure.
Keywords: Heart failure; Sleep apnea syndrome; Profile of patients
Introduction
Sleep apnea syndrome (SAS) in heart failure is attracting increasing interest due to its high prevalence in the range of 50-60 % [1,2,4- 6].
It is defined by symptoms related to the occurrence during sleep of apneas and / or hypopneas that correspond to the interruption (apnea) or decrease of more than 30% (hypopnea) of the inspiratory flow, during more than 10 seconds or more and occurring in more than 5 per hour during sleep [2,4,9,11].
In patients with heart failure, SAS may be obstructive by collapse of the upper airway with persistence of inspiratory effort, i.e., central characterized by use Cheyne-Stokes breathing, or still mixed (coexistence of both types) [1,2,12].
The presence of SAS in people with heart failure appears to be a contributing factor to the impairment of ventricular function and thus to the worsening of heart failure [2,13,14], this which justifies its systematic screening in this pathology [2,13].
The clinical signs suggestive of SAS are not very specific, even if the notions of obesity, nocturnal breathing pauses noted by relatives, nocturnal snoring, daytime sleepiness, non-restorative sleep sensation with fatigue are suggestive. it should be stressed that the IC patients are less drowsy than others with equivalent SAS severity, the symptomatology is poorer with regard to central SAS, because besides the patients are not drowsy, they do not snore and is sometimes noticed also at wakefulness or during a stress test [12].
Polygraphy is the examination that comes second after polysomnography, it is a simple examination to perform, allows to record the cardiorespiratory parameters and to determine the type of apnea (obstructive, central or mixed) as well as the severity of the SAS, by calculating the index of apneas and hypopneas (AHI).
In this work, we evaluate the profile of patients with the association of sleep apnea syndrome and heart failure as well as their characteristics according to the type of SAS.
Methodology
This is a monocentric descriptive retrospective study spread over a 2-year period from November 2019 to December 2021.
We included patients with SAS, confirmed by polygraphy, with at least one hospitalization in the cardiology department of the Deux hospital for cardiac decompensation. Patients with minor SAS were excluded from the study.
We selected 42 patients, The studied parameters reported in our series are: cardiovascular risk factors and history, number and mode of hospitalizations for decompensation cardiac ultrasound data, including the ejection fraction of the left ventricle (LVEF), left ventricular hypertrophy (LVH), mitral profile, left atrium surface (OG), pulmonary pressures (PAPS) as well as the type of heart failure and its etiology.
We defined heart failure with reduced ejection fraction (LVEF) ≤40% (CI-FER) and heart failure with preserved ejection fraction ≥ 50% (CI-FEP) [3].
Data were analyzed with SPSS version 12 software and results expressed as percentages and averages ± standard deviations
Finally, multiple correspondence analysis was used to project qualitative variables on a factorial basis.
Results
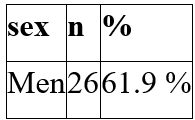
We included 42 patients including 26 men (61.9%) and 16 women (38.1%). The sex ratio is 1.62. The age of patients is 68 years (31-85 years). The average age of men was 67, younger than women whose average age was 70.
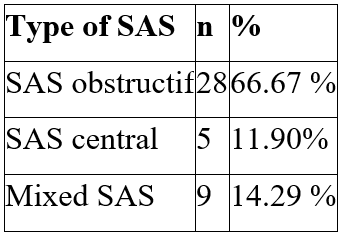
SAS is severe in the majority of patients. The average apnea hypopnea index (AHI) of our population is 42 ± 14. A predominance of obstructive SAS was noted with 66.67% (n = 28), compared to 14.29% (n = 9) for mixed SAS and 11.90% (n = 5) for central SAS.
High blood pressure was found in 71.43% of patients (n = 30), dyslipidemia in 73.81% (n = 31), obesity in 40.48% of patients (n = 17), atrial fibrillation in 47.62% of patients (n = 20), diabetes in 33.33 % of patients (n = 14).
Table 1: Distribution of patients by sex.
Clinically, acute lung oedema (OAP) is the most common mode of decompensation with 52.6% of our patients (n = 25).
Global cardiac decompensation is found in 17 patients, or 47.4%.
Table 2: Distribution of patients by type of SAS.
Regarding echocardiographic parameters, dilation of the left atrium (OG) is found in 42.86 % of patients.
The average LV ejection fraction is 56 ± 13 with medium extremes ranging from 20 to 76%. The type III mitral profile is significantly found in (38.10%, n = 16) of patients, against the type II profile (23.81%, n = 11) and the type profile (35.71%, n = 15) PAH was found in 6 patients (14.29 %).
Indeed, in our patients, heart failure with preserved ejection fraction (HF-FEP) predominates with 88.10% of cases against systolic heart failure (HF-IRON) with 11.90%.
The ischemic etiology of heart failure is found in 15 cases (35.71%), non-ischemic dilated cardiomyopathy (DCM) is found in 9 cases (21.43%), hypertensive heart disease predominates in our series with 18 cases (42.86%)
Table 3: Key patient histories.

Table 4: Clinical features, echocardiography, type and etiology of heart failure.

The number of hospitalizations per patient during the study period ranged from 1 to 6, The mean was 1.74 ± 0.94, with no significant difference by type of SAS.
Multifactorial analysis of our data shows that central SAS is associated with systolic heart failure, non-ischemic DCM, restrictive mitral type profile and permanent fibrillation. On the other hand, mixed SAS is associated withIC-FEP, hypertensive heart disease, LVH, mitral profile type 2 and paroxysmal atrial fibrillation.
Therapeutically, more than half of our patients are treated with continuous positive airway pressure (CPAP) (n: 27 or 64.29%). 15 patients (35.71%) benefit from a mandibular advancement orthosis. 9 patients (11.8%) have a pacemaker for sinus dysfunction; 1 patient has a defibrillator for primary prevention.
Loop diuretics, ACE inhibitors/sacubitril-valsartan and beta-blockers are prescribed in 84.8%, 86%, and 75.4% of patients, respectively.
Table 5: Main treatments of patients.

Discussion
The three forms of SAS (central, obstructive and mixed SAS) described in people with heart failure [1,2,8,9,12] are found in our patient population. Screening studies for SAS in people with heart failure clearly show the high prevalence of central SAS in the presence of heart failure [1,2,4,8,11,12], in contrast to what is seen in the general population where SAS is 95 % of obstructive type [2,6,8,11,12,13,14].
The high prevalence of obstructive SAS in our patients seems to be related to the obesity factor, whose impact on the occurrence of obstructive SAS is known and whose prevalence increases with age [2,8,10, 14,15,16].
Central SAS predominates in young subjects with systolic dysfunction [1,2,12,17].
The predominance of male patients found in our patient population affirms the data from the literature [17,18,19,20,21,]. It is indeed described a higher prevalence in men 4% against 2% in women, in the same age group [2,8,16,18].
However, we did not find a statistically significant difference by patient sex.
Highly significant factors appear in our patients: obesity, hypertension, dyslipidemia, this observation is recurrent in the literature [2- 6,12].
There is arguably a linear relationship between IAH, high blood pressure and BMI [2,4,5,11].
Similarly, atrial fibrillation has a significant relationship with the combination of heart failure-SAS. SAS has been shown to significantly increase the prevalence of atrial fibrillation in people with heart failure [2,8,17,21]. SAS can be considered as an experimental model of atrial fibrillation by pressure overload and dysautonomia [3,4,17,19].
GGO dilation is cited as a specific factor in the SAS-heart failure association [1,2,8]. Similar to diastolic LV dysfunction, LV filling pressures are significantly higher in patients with SAS [1,7,19,21].
In our study, the restrictive mitral pattern is a factor significantly related to the SAS-heart failure association.
However, the results on the type and etiology of heart failure are divergent [1,2,8,17,18].
In our series, analysis of the results reveals a significant predominance of HF-FEP and hypertensive heart disease.
This result could be explained, on the one hand, by the fact that our study concerning the association SAS - heart failure is carried out in stable heart failure with systolic dysfunction of the LV (LVEF mean 30%). On the other hand, the advanced age of our patients predisposes them more to the development of a CI-FEP, but we also know that the CI-FEP is more a complication of hypertension [14,18,21-24].
There is a close relationship between central SAS, systolic heart failure, non-ischemic heart disease, mitral profile type 3 and permanent atrial fibrillation.
Similarly, for mixed SAS, LVH, IC-FEP, mitral profile type 2, hypertensive heart disease and paroxysmal atrial fibrillation. Similar results have been reported in the literature [1, 7, 16, 19, 20].
GHRAIDI A. et al. demonstrated [21] the link between the mitral profile type 1 and obstructive SAS and that the mitral profile type 3 would favor central SAS.
Regarding PAH, it appears in our study as a factor of poor prognosis, Diastolic dysfunction of the LV and hypoxic arteriolar vasoconstriction have been implicated as a mechanism of development PAH in SAS-heart failure patients [25,27].
The management of OSA in our series is based on continuous positive airway pressure nocturnal ventilation, its effectiveness on cardiovascular morbidity and mortality was described in 2005 by Marin et al. which showed that OSA mortality with apnea-hypopnea index (AHI))> 30/h was corrected in patients choosing CPAP therapy [28].
The SAVE study on more than 2700 patients with moderate to severe SAS in prevention
Secondary, randomized standard treatment alone versus standard treatment plus CPAP found no beneficial effect of CPAP treatment on cardiovascular risk.
The treatment of central SAS proposed in our patients with an IC-FER is based on the optimization of medical treatment, the introduction of new molecules of heart failure and cardiac resynchronization electrophysiology, no other treatment recommendations are established, as the various studies are based on a low level of evidence. Oxygen therapy induces a decrease in AHI of 15/h and an improvement in LVEF of + 5%, but this in monocentric studies with significant variability, suggesting a great heterogeneity of patients, some of whom do not are not responders. [3,7,28].
As far as VET CI is concerned, few studies are available. There is only one randomised trial in a small size, where self-controlled ventilation (ASV) treatment improved dyspnoea and survival, without significant excess adverse events, Currently, these patients are fitted if the optimization of cardiovascular treatment is insufficient. Data from the FACE cohort study and the FACIL-VAA registry, two ongoing French studies, will certainly be of interest. [7,28,29].
Conclusion
Sleep apnea syndrome is common in people with heart failure warranting broad screening.
Dilation of the left atrium, mitral profile type 3 and atrial fibrillation are statistically related factors to the association SAS-heart failure. Emphasis must be placed on knowledge of the factors allowing the screening of patients, the implantation of new stimulators cardiac with analysis of apneas and ear rhythm disorders. this is in order to adapt ventilation and antiarrhythmic treatment on the one hand, and the realization of systematic echocardiography to patients with SAS, on the other hand.
It is established that CPAP treatment improves the prognosis of patients with heart failure and provides a benefit on morbidity, clear in obstructive SAS, probable in central SAS, but still to be confirmed by large-scale studies.
Declaration of Interests: The authors declare that they have no conflict of interest in relation to this article.
References
- Tsemo Watchueng G, Mouly-Bertin C, Depagne C, Lantelme P, Guerin J-C. Factors associated with sleep apnea syndrome in heart failure. Annal cardiol angiol, 2011; 0; 1-2
- P Balagny, E Wiernik, J Matta, J Frija-Masson, Prevalence of sleep apnea syndrome and its association with cardiovascular events in the general French population- Revue des Maladies, 2020; 5 : 407-416.
- McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J, 2021: ehab368. doi:10.1093/eurheartj/ehab368.
- Javaheri S, Parker TJ, Liming JD, et al. Sleep apnée in 81 ambulatory male patients with stable heart failure. Types and their prevalence, consequences, and presentation. Circulation, 1998; 21: 2154-2159.
- Michael Arzt, Terry Young, et al. Sleepiness and Sleep in Patients with Both Systolic Heart Failure and Obstructive Sleep Apnea, Arch Intern Med, 2006; 166.
- Durieux P, Neukirich F. Epidemiology of adult sleep apnea syndrome. Rev badly resp, 1990; 7: 441-449.
- Bocquillon V, Destors M, Guzun R, Doutreleau S, Pépin JL. Tamisier dysfunction and the obstructive sleep apnoea syndrome, revue des maladies respiratoires, 2020; 161-170.
- Sin DD, Fitzgerald F, Parker JD, et al. Risk factors of central and obstructive sleep apnea in 450 men and women with congestive heart failure. AM J Respir ait Care Med, 1999; 1101: -6.
- Lering RS, Bradley TD. Sleep apnéa and cardiovascular disease. Am J Respir ait Care Med. 42001; 16: 2174-2167.
- Sin DD, Fitzgerald F, Parker JD, et al. Relationship of systolic BP to obstructive sleep apnéa in patients with heart failure. Chest, 2003; 1: 1536-543.
- Tracova R, Rankin F, Fitzgerald F, et al. Effects of continuous positive airway pressure on obstructive sleep apnéa and left ventricular afterload in patient heart failure. Circulation, 1998; 98: 2269-2275.
- From Ortho Marie-Pia. Sleep apnea syndromes in people with heart failure. Cardio consensus, 2009; n° 49.
- Oldenburg O, Lamp B, Faber L, et al. Sleep disordered breathing in patients with symptomatic heart failure a contemporany study of prevalence and characteristics of 700 patients. Eur J Heart fail.) 2006; 9(3): 251-257.
- Yaggi HK, Concato J, Kerman WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med, 2005; 353: 2034-2041.
- Lavie P, Herer P, Hoffstein V. Obstructive Sleep apnea syndrome as a risk factor for hypertension: population study. BMJ.32000; 479-482.
- Laaban JP. Cross-epidemiology of obese and sleep-disordered breathing. Sleep medicine, 2004; 1: 13-16.
- De Roguefeuil F. Sleep apnea syndrome. What should a cardiologist know in 2013? Cardiology- cardinal, 2013; 54 (7); 13-23
- Kohnlein T, Welte T, Tan LB, Eliott MW. Central sleep apnea syndrome in patients with chronic heart disease: a critical review of the current literature. Thorax, 2002; 57: 547-554.
- Javaheri S. A mechanism of central sleep apnea in patients with heart failure, N eng J Med, 3149199; 949-954.
- Javaheri S. Sleep disorders in systolic heart failure: a prospective study of 100 male patients. The final report .int J Cardiol 1200606; 21-28.
- Chrairi A, Trimeche B, Bouraoui H, et al. Diastolic dysfunction and sleep apnea syndrome in stable heart failure.
- Juillier Y, Trochu JN, Decroote P, et al. Heart failure with preserved systolic function: a diagnostic algorithm for a pragmatic definition. Arch Evil Heart, 2006; 9; 279-286.
- Banno K, Shiomi T, Sasanab R, et al. Sleep- disordered breathing in patients with idiopathic cardiomyopathy. Circu J, 2004; 68: 338-342.
- Alexandor N, Ugontzas A, Edward O, et al. Sleep apnea is a manifestation of the metabolic syndrome. Sleep Med Rev, 2005; 9; 211-224.
- Bradley TD, Floras JS. Obstructive sleep apnea and its cardiovascular consequences. Lancet, 2009; 373: 82-103.
- Tracova R, Miroumand M, Lorenzi M, Lorenzi- Lilho G, BradleY TD. Overnight shift from obstructive to central apnéas in patients with heart failure: role of PCO2 and circulatory delay. Circul ation0, 2011; 1: 238-243.
- Pepin JL, Levy P. Pathophysiology of cardiovascular risk during sleep apnea syndrome. Journal Neurology, 2002; 9: 158–189.
- Marin JM, Carrizo SJ, Vicente E, et Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with conti- nuous positive airway pressure: an observational study. Lancet, 2005; 365: 1046-1053.
- Akiomi Yoshihisa,Satoshi Suzuki,Takayoshi Yamaki,Koichi Sugimoto,Hiroyuki Kunii,Kazuhiko Nakazato,Hitoshi Suzuki,Shu-ichi Saitoh,Yasuchika Takeishi . empact of adaptive servo-ventilation on cardiovascular function and prognosis in heart failure patients with preserved left ventricular ejection fraction and sleep- disordered breathing.

