How Much Cost Saving Can Be Achieved by Introducing a Scoring System to Triage Women with Heavy Menstrual Bleeding?
Al-Inizi Shamma*
Consultant obstetrician and gynaecologist, South Tyneside & Sunderland NHS Foundation Trust, UK
Received Date: 21/02/2023; Published Date: 14/04/2023
*Corresponding author: Dr. Shamma Al-Inizi, MBChB, MSC, CABOG, DFFP, CCT, PG CERT MED ED, FRCOG, Consultant obstetrician and gynecologist, South Tyneside & Sunderland NHS Foundation Trust, Kayll Road, Sunderland, SR4 7TP, United Kingdom
Abstract
Heavy Menstrual Bleeding (HMB) can affect women`s physical, emotional, social wellbeing and their quality of life. Prolongation of the treatment journey by undergoing different medical and surgical uterine sparing modalities such as the Intrauterine System (IUS) & Endometrial Ablation (EA) prior to definitive treatment for this condition, can increase women`s suffering and add more cost. Certain gynaecological pathologies can predispose to hysterectomy in women with HMB such as fibroids, adenomyosis and endometriosis.
We propose introducing a scoring system (score 1-6) based on different parameters retrieved from the patient`s history, examination, and investigations, which aims to triage women with HMB into hysterectomy & uterine sparing modalities. We anticipate that this scoring system would ultimately reduce the cost spent on the overall treatment, by avoiding uterine sparing modalities when the score =>3 and would reduce the treatment journey by offering definitive surgery (hysterectomy) early where these modalities would usually fail.
We have reviewed 300 women who underwent hysterectomy for HMB over 5 years at South Tyneside & Sunderland Hospitals. We looked at different parameters and introduced the scoring system. We then calculated the cost spent on the uterine sparing modalities prior to hysterectomy which was found to be significant. Realising the amount of money spent on the medical and surgical interventions prior to hysterectomy in women with HMB would encourage the clinician to consider utilization of this scoring system in order to avoid unnecessary interventions, cost and prolongation of suffering prior to definitive treatment when the score is >=3.
Keywords: Heavy menstrual bleeding; Scoring system; Cost
Introduction
Several women are referred to secondary care hospitals in the UK annually with HMB and are offered different medical and surgical uterine sparing modalities before definitive treatment (hysterectomy) is offered. These modalities add not only a significant cost which the service provider would pay on top of the cost of definitive surgery, but also add prolongation of suffering which would further affect women`s quality of life and wellbeing.
The two most widely used uterine sparing medical and surgical interventions in modern gynecological practice for HMB are the Levonorgestrel IUS (Mirena IUS Bayer Healthcare pharmaceutical) and EA. They both proved to be very effective in managing these symptoms and controlling women`s suffering [1-4].
These procedures represent a lower cost with a shorter recovery time compared to hysterectomy. However, on a longer term follow up as highlighted by the ECLIPSE Trial; 1:5 women needed hysterectomy after 5 years of having the Levonorgestrel IUS [2]. The same applies to EA, where longer term follow up showed reduced treatment efficacy and women`s satisfaction with a post ablation hysterectomy rate reaching 21% in some series [5].
In the UK, ‘cost pressures on the National Health Service (NHS) will only grow and it needs a proper sustainable funding solution which will most probably result in a substantial tax increase’ [6]. Trends and plans to reduce NHS cost spent by the health system is usually welcomed [7].
In this study we calculated the spent cost on uterine sparing modalities prior to hysterectomy in women with HMB. In order to consider reducing the cost spent together with improved quality of care via shortening the treatment journey prior to hysterectomy, a scoring system was introduced. Certain pathologies can predispose to hysterectomy in HMB which we tried to incorporate into the scoring system we introduced. This scoring system aimed to triage women into hysterectomy and uterine sparing medical and surgical modalities based on the woman`s history, examination findings, results of investigations such as ultrasound scan and haemoglobin level correlating that to the histology of the removed uterus at hysterectomy.
This can support the counselling process in the future towards hysterectomy or uterine sparing modalities in women with heavy menstrual bleeding.
Materials & Methods
A retrospective review of electronic records of all women referred to South Tyneside and Sunderland hospitals between January 2016 and December 2020 with HMB who ended having hysterectomy, was conducted. 1246 hysterectomies during the period of the study were reviewed and only 300 women had hysterectomy for HMB were included in the study. Hysterectomy for other reasons such as uterovaginal prolapse, premalignant or malignant conditions, large ovarian masses, and chronic pelvic pain without HMB and post-menopausal bleeding were excluded. A detailed data collection proforma was used where women`s clinical details were documented. This included associated symptoms such as chronic pelvic pain, dysmenorrhoea, dyspareunia or known endometriosis, examination findings of uterine cavity length, symptomatic anaemia necessitating blood or iron transfusion and ultrasound scan suggesting leiomyoma >3 cm or adenomyosis and woman`s desire for definitive surgery. Information on previous medical & surgical interventions performed prior to hysterectomy was obtained. Histology of the removed uterus was reviewed and was linked to the pre-hysterectomy symptoms and scan findings. Cost for each uterine sparing medical and surgical intervention was calculated according to the local hospital NHS coding system. The electronic proforma was completed on Excel spread sheets. A simple statistical tool was used to analyse the data. Ethical approval, and patients` consent were not required as the study is a retrospective electronic record review study.
Results
300 women had hysterectomy for HMB during the period of the study & were included. Age ranged between 31-56 with a mean age of 45. Parity ranged between 0-4 with a mean of 2. Duration of HMB ranged between 1-15 years with a mean of 3 years. 110 women (36.6%) had history of CPP, dysmenorrhoea, dyspareunia or were known to have endometriosis. 142 women (47%) expressed their desire for definitive treatment (hysterectomy) during their consultation aiming for complete amenorrhoea, however; most of them were offered uterine sparing modalities first (Tables 1,2). 140 women (44.7%) had an ultrasound scan (USS) indicating a fibroid(s)>3 cm whereas, 25 women (8%) had an USS finding of adenomyosis. 88 women (29.3%) had a large endometrial cavity>10 cm on examination measured by the pipelle endometrial biopsy aspirator (Table 1). 64 women (21.6%) were found to be anaemic but only 32 women (10.6%) their symptomatic anaemia needed blood/ iron transfusions with the lowest recorded Hb to be 5.7 gm/dl (Table 1). 118 women (39%) had the Levonorgestrel IUS (Mirena IUS, Bayer Healthcare pharmaceuticals) whereas, 116 women (38.6%) had EA. 41 women had both EA & IUS (13.5%), Table 2.
The commonest EA performed was found to be the NovaSure EA (NovSure, Hologic INC, Bedford MA) which was performed in 90 women (30%), where 5 of them had the Novasure ablation procedure repeated (1.6%). The rest had transcervical resection of endometrium (TCRE) (Richard Wolf UK Ltd Monopolar resectoscope system, Waterside Way, London), the Minitouch endometrial ablation (MINITOUCH Ltd, Durham, UK) & Hydrothermal Ablation (HTA) (Genesys HTA system, Boston Scientific, Portsmouth, UK) (Table 3). 63 women had laparoscopic sterilisation/bilateral salpingectomy for family planning with the EA (21%) especially women are usually advised not to fall pregnant post endometrial ablation and sterilisation is often suggested to be performed at the same time, being a good option to prevent pregnancy after ablation [8].
41 women (13.5%) had both EA & the IUS (Table 2). Different varieties of medical treatment such as Tranexmic acid, Mefenamic acid, the contraceptive pill, Depo provera injections, the progesterone implant, Esmya (Ulipristal Acetate) and Gonadotrophin releasing hormone analogue (GNRHA) were also offered (Table 2). 183 (61%) had laparoscopic hysterectomy, 75 women (25%) had abdominal hysterectomy and 42 women (14%) had vaginal hysterectomy. Upon reviewing histology of the removed uterus, 254 women (85%) had a pathology at histology (Table 4). The commonest identified pathology was benign fibroid followed by adenomyosis or both. Associated fibroid>3 cm and women`s desire for complete amenorrhoea were identified to be the commonest associated factors leading to hysterectomy (Table 1). A scoring system of 1-6 was introduced based on these identified parameters (Table 1). Histological examination identified a much higher number of fibroids and adenomyosis to what was identified by US scan (65% had benign fibroids and 42% had adenomyosis on histology VS 44.7% had fibroids on USS & 8% had adenomyosis), (Tables 1,4). Improvement in gynaecological scanning is suggested in women with HMB.
75% of women who had hysterectomy for HMB in this study had scored >=3 (Table 1).
Cost of the medical and surgical uterine sparing interventions was calculated by adding all the costs needed for these interventions according to an NHS-hospital coding system & the British National Formulary (BNF). This total cost was found to be £ 413,699 (Table no. 5). This spent cost has been paid by the health provider in the UK (The NHS) and it is on top of the cost paid for hysterectomy in all the women included in this study.
Table 1: Associated factors leading to hysterectomy with their suggested score.
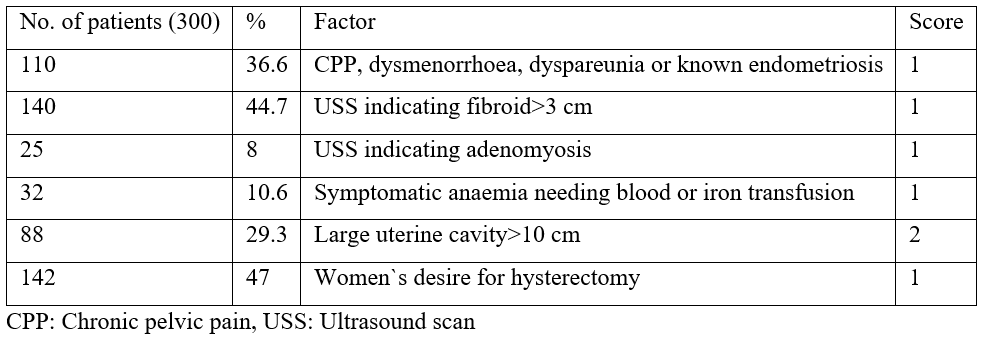
Table 2: Medical and surgical uterine sparing interventions prior to hysterectomy.
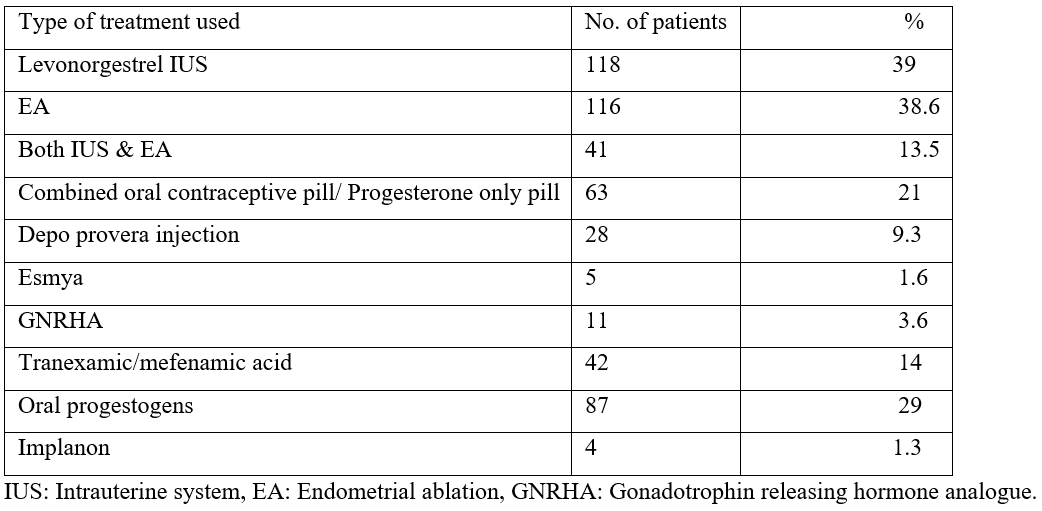
Table 3: Types of endometrial ablation used in the study.
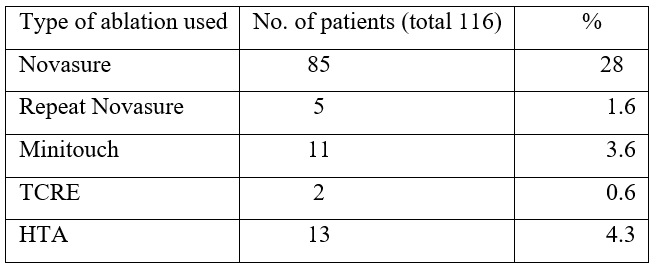
Table 4: Histological examination of the removed uterus at hysterectomy.
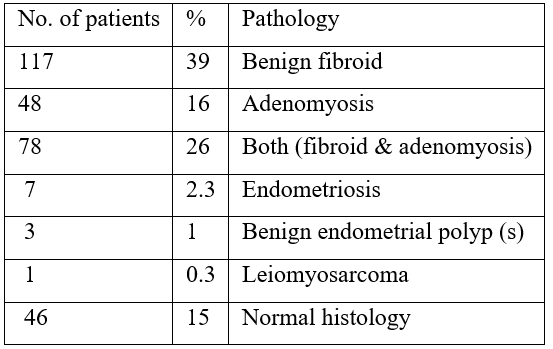
Table 5: Spent cost on each uterine sparing medical and surgical intervention.

Discussion
In the UK, The National Health Service (The NHS) is a unique system of its kind where taxpayers’ money is utilised to provide a free health system to the public with consideration of reduced waste of that money and setting targets to provide a better service for the patients [9]. The NHS constitution considers six major values to ensure the best possible care for the patients which are: working together for patients, respect and dignity, commitment to quality of care, compassion, improving lives and everyone counts [10].
Over the years, the NHS Bill is growing, and this growth mostly results from the older population growth, together with the increased patients suffering from chronic health illnesses in addition to the high drug bills [6]. The NHS has always planned to improve quality of care together with reducing spent cost on the services provided [7]. A recent report indicated that reviewing past trends in the NHS productivity could provide few lessons for current financial challenged health system, one of which is by providing support to clinical teams to make improvements to the way they deliver services in collaboration with their patients [7]. It has been published before that improving quality reduces costs of treatment and improves value-for-money across the whole health care system [11].
This retrospective study aimed to calculate the cost spent on women referred to hospital with HMB who needed multiple interventions prior to having definitive surgery (hysterectomy). It also aimed to improve the quality of care provided to this group of women especially when suffering was prolonged and definitive surgery was not offered early. Cost saving is proposed to be achieved by avoiding uterine sparing modalities offered to those women if they score >=3 according to a suggested scoring system introduced in this study.
Heavy menstrual bleeding is a common condition affecting 1:4 women during their reproductive life [12]. Around 50000 women are referred annually to the National Health Service (NHS) at secondary care hospitals with HMB in England and Wales [13]. Around 28000 of those women undergo surgical management of HMB, the commonest of which is EA [13]. HMB has several implications on quality of life by affecting the physical and mental health of women as well as their emotional and social wellbeing [13]. It can also be associated with severe pain symptoms, anaemia and fatigue [14,15].
Different pathologies can be associated with HMB including uterine fibroids, adenomyosis and endometriosis which can predispose to additional symptoms including pelvic pain, dysmenorrhoea, dyspareunia and pressure symptoms. Identifying these symptoms during the gynaecological consultation for HMB is important which can highlight the possible association of these pathologies with HMB.
Stevens et al in 2019 published a retrospective review predicting the likelihood of failed EA used to treat HMB. This was based on woman`s age, parity, duration of HMB, associated dysmenorrhoea and previous caesarean section [1]. It suggested that this prediction could aid clinicians in the counselling process for EA in women with HMB by predicting the likelihood of a failed procedure needing further intervention in the following two years post EA [1]. In our study, we identified different factors associated with HMB leading to hysterectomy. These factors were retrieved from symptoms at presentation, uterine cavity length at examination, investigations including USS & haemoglobin level, women`s desire for definitive treatment and histology of the removed uterus.
Associated chronic pelvic pain, dysmenorrhoea, dyspareunia or known endometriosis & adenomyosis were identified as risk factors for failed medical & surgical uterine sparing modalities for HMB in this study, especially these modalities might not improve the pain symptoms completely. EA was reported to be associated with post ablation pelvic pain in 20.8% of women in one series especially in women with pre ablation dysmenorrhoea and endometriosis [16]. It was recommended to properly counsel women regarding the expected surgical outcome post EA in this group [16]. Late-Onset Endometrial Ablation Failure (LOEAF) was lately identified to be associated with hysterectomy in 25% of women undergoing EA regardless of the type of EA used and an unknown number of women who had EA had less than satisfactory results in that series [17]. It has been suggested that understanding factors which lead to LOEAF with good patient selection for the procedure would reduce LOEAF and improve patient`s satisfaction [17]. The commonest cause of post ablation hysterectomy in some series was found to be recurrence of HMB due to inadequate destruction of the endometrium or its regrowth following ablation, chronic pelvic pain, leiomyomas and adenomyosis [17-19]. On the other hand, the Levonorgestrel IUS was found to be associated with failure to control HMB in women with a uterine fibroid>=2.5 cm or a uterine size of>12 cm [20].
In this study, we found that 36.6% of the identified patients had chronic pelvic pain, dysmenorrhoea, dyspareunia or known endometriosis, in addition to 8% had an USS finding of preoperative adenomyosis and 44.6% of uterine fibroid of >=3 cm size. The failure rate of EA in this study was 38.6%, failed Levonorgestrel IUS rate was 39%, whereas both failed in 13.5%. Considering histology, we recognised that several women had fibroids and adenomyosis which were not picked up on USS and were confirmed by histology (Tables 1,4). We appreciate that adenomyosis is more difficult to be picked up on USS compared to uterine fibroids. We recommend further training in gynaecological USS to improve diagnosis. It has been suggested that further training in 3D USS can further pick up adenomyosis [21]. Hanafi M suggested that USS is a valuable non-invasive method to diagnose leiomyoma with or without adenomyosis which can be sensitive but not specific in the diagnosis of adenomyosis [22].
Large uterine cavity >10.5 cm was identified as a risk factor for failed EA and LOEAF and it can also be associated with a failed Levonorgestrel IUS [18,23]. In this study 29.3% of women had a large endometrial cavity >10 cm length which has resulted in failed uterine sparing medical and surgical procedures namely EA and IUS.
We identified that 21.6% of the women in this study were anaemic on oral iron therapy but 10.6% had iron infusions with blood transfusion due to their life-threatening anaemia. We considered this group of women as a potential group benefiting from hysterectomy if other scoring factors existed, giving anaemia needing blood/iron transfusion one score (Table 1). Iron deficiency anaemia can result from chronic and excessive heavy menstrual blood loss and can be life-threatening which should be addressed proactively [24]. A consensus guidance covering screening and diagnosis of iron deficiency anaemia in women with HMB has been suggested to improve health outcomes in those women [25].
Hysterectomy is the most performed major surgical procedure in gynecology [26]. Despite its invasive nature, it represents the most definitive treatment option for HMB in women where future fertility is not a requirement [26].
Due to its invasive nature with longer recovery time and complications, it was suggested that hysterectomy should only be considered when other treatment options have failed or are contraindicated [26].
Women`s desire for definitive treatment was identified as a risk factor leading to hysterectomy in this study. This was especially identified in women aiming for complete amenorrhoea where other uterine sparing modalities such as the Levonorgestrel IUS and EA might not guarantee. Nearly half of the women who had hysterectomy for HMB in this study had a desire for complete amenorrhoea. We recommend that having some additional risk factors to woman`s desire for hysterectomy would aid the clinician to offer definitive treatment for HMB.
A massive financial cost of £ 413,699 was identified by calculating all the medical and surgical cost spent on managing women referred with HMB during the period of the study prior to hysterectomy. This included all medical interventions such as the IUS and surgical management using EA (Table 5). The cost becomes higher when women were offered permanent contraception as recommended by the American College of Obstetricians and gynaecologists offering a long-term reliable contraception for women undergoing endometrial ablation [8]. Due to the fact that hysteroscopic approach for sterilisation is not available anymore, women are offered laparoscopic approach for sterilisation during EA [27]. There is a steady trend towards laparoscopic salpingectomy versus laparoscopic clip sterilisation as shown in our study (Table 5), due to the international recommendation of its large benefits including sterility & decreased lifetime risk of epithelial-cell ovarian cancer [27-30]. It has been suggested that laparoscopic bilateral salpingectomy combined with endometrial ablation could become the most-common surgery performed by gynecologic surgeons [27]. This would include an additional cost (Table 5).
Cost reduction programs in health systems have always been suggested, but most hospitals lack effective cost reduction programs, a recent survey found [31]. This survey recommended that hospitals must identify areas of savings, establish a governance structure and foster collaboration to achieve effective cost reduction programs [31].
A way of introducing a cost reduction process in gynecology clinics, we recommend introducing a scoring system (Table 1), where women who score >=3 would be counselled towards having hysterectomy rather than uterine sparing medical and surgical modalities especially 75% of the women in the study were found to score >=3. This would result in massive cost saving considering the huge cost we calculated on all these modalities utilised prior to hysterectomy in the study group. This study is limited by not including women who were referred with HMB and did not end up having hysterectomy.
Conclusion
A significant cost saving can be achieved by introducing a scoring system which aims to triage women referred with HMB into hysterectomy and uterine sparing modalities. This would also improve patient`s satisfaction and suffering by shortening the treatment journey towards definitive surgery. We suggest conducting a randomised controlled trial using this scoring system for women referred with HMB in the future to aid in patient`s selection for different treatment options.
Competing interest and grant information: I confirm that there is no competing interest to declare and I did not receive any grant to conduct this study.
Acknowledgements: We would like to thank Miss Claire Challoner, Dr. Nazoorah Malek, Dr. Ala Abdullah, Dr. Neelam Agrawal and Dr Sheena Johns in helping us to collect the data.
References
- Stevens KYR, Meulenbroeks D, Houteran S, et al. Gynecol Surg. Weyers S. Prediction of unsuccessful endometrial ablation: a retrospective study, 2019; 19(7). org/10.1186/s10397-019-1060-1.
- Gupta J, Daniels J, Middleton L. A randomised controlled trial of the clinical effectiveness and cost-effectiveness of the levonorgestrel-releasing intrauterine system in primary care against standard treatment for menorrhagia: the ECLIPSE trial. Health Technol Assess, 2015; 19(88): i-xxv, 1-118. DOI: 10.3310/hta19880.
- Kumar v, Chodankar R, Gupta J. Endometrial ablation for heavy menstrual bleeding. Women’s Health (London), 2016; 12(1): 45-52. doi: 2217/whe.15.86.
- Matteson KA, Abed H, Wheeler TL, et al. A systematic review comparing hysterectomy with less-invasive treatments for abnormal uterine bleeding. J Minim Invasive Gynecol, 2012; 19(1): 13-28. https://doi.org/10.1016/j.jmig.2011.08.005
- Kiran A, Geary RS, Urganci IG, et al. Sociodemographic differences in symptom severity and duration among women referred to secondary care for menorrhagia in England and Wales: a cohort study from the National Heavy Menstrual Bleeding Audit. BMJ, 2018; 8(2): e018444. doi:10.1136/bmjopen-2017-018444.
- Charlesworth A, Watt T, Kelly E. The health foundation. Securing the future: funding health and social care to the 2030s: Cost pressures on the NHS are set to grow; a long-term funding solution is needed, likely through tax increases. Institute for Fiscal Studies. NHS Confederation, 2018.
- Better value in the NHS: The role of changes in clinical practice: report summary. The Kings Fund-Ideas that change health care. 2015.
- Dalmo S. ACOG Guideline on Endometrial Ablation. Am Fam Physician, 2008; 77(4): 545-546.
- Smith T. The NHS Bill. BMJ, 1989; 299(6712): 1354. Doi:10:1136/bmj.299.6712.1354.
- The NHS Constitution for England, Health Education England, updated Jan 2021. The NHS belongs to us all.
- MacArthur H, Philips C, Simpson H, et al. Improving quality reduces costs- Quality as the business strategy. 1000 Lives Plus, Improving Healthcare White Paper Series-No.8, 2012.
- Kiran A, Geary RS, Urganci IG, et al. Sociodemographic differences in symptom severity and duration among women referred to secondary care for menorrhagia in England and Wales: a cohort study from the National Heavy Menstrual Bleeding Audit. BMJ, 2018; 8(2): e018444. doi:10.1136/bmjopen-2017-018444.
- Royal College of Obstetricians and Gynaecologists, London School of Hygiene & Tropical Medicine, Iposos MORI, National Heavy Menstrual Bleeding Audit: Third Annual Report. London, UK: RCOG Press, 2013.
- Wang W, Bourgeois T, Klima J, et al. Iron deficiency, and fatigue in adolescent females with heavy menstrual bleeding. Haemophilia, 2013; 19: 225-30. DOI: 1111/hae.12046
- Cohen BJ, Gibor Y. Anemia and menstrual blood loss. Obstet Gynecol Surv 1980; 35:597-618. PMID: 6997784.
- Thomassee M, Curlin H, Yunker A, et al. Predicting pelvic pain after endometrial ablation: which preoperative patient characteristics are associated? J Minim Invasive Gynecol. 2013;20(5):642-647. Doi: 10.1016/j.jmig.2013.04.006
- Wortman M. Late-Onset endometrial ablation failure. Case Reports in Women s Health. 2017;15. Doi: 10.1016/j.crwh.2017.07.001
- McCausland AM, McCausland VM. Depth of endometrial penetration in adenomyosis helps determine outcome of rollerball ablation. Am J Obstet Gynecol, 1996; 174: 1793-1794. DOI: 1016/s0002-9378(96)70211-9
- Seidman JD, Kjerulff KH. Pathologic findings from Maryland Women`s Health Study: practice patterns in the diagnosis of adenomyosis. Int J Gynecol Pathol, 1996; 15: 217-221. DOI: 1097/00004347-199607000-00005
- Singh K, Bharati G, Prasad D, et al. Role of levonorgestrel releasing intrauterine device in management of heavy menstrual bleeding: a conservative approach. Int J Reprod Contracep Obstet Gynecol, 2017; 6(2): 01-31. DOI:10.18203/2320-1770.ijrcog20170396.
- Struble J, Reid S, Bedaiwy M. Adenomyosis: A clinical review of a challenging gynecologic condition, J Minim invasive Gynecol, 2016; 1(2): 164-185. DOI:10: 1016/j.jmig.2015.09.018.
- Hanafi M. Ultrasound diagnosis of adenomyosis, leimyoma, or combined with histopathological correlation. J Hum Reprod Sci, 2013; 6(3): 189-193. DOI: 4103/0974-1208.121421
- Shazly SA, Famuyide AO, El-Nashar SA, et al. Intraoperative predictors of long-term outcomes after radiofrequency endometrial ablation. J Minim Invasive Gynecol, 2016; 23: 582-589. DOI: 1016/j.jmig.2016.02.002
- Nelson A, Ritchie J. Severe anemia from heavy menstrual bleeding requires heightened attention. Am J Obstet Gynecol, 2015; 213(1): 97.e1- 97.e6. DOI: 10.1016/j.ajog.2015.04.023
- Mansour D, Hofmann A, Gemzell-Danielsson K. A review of clinical guidelines on the management of iron deficiency and iron-deficiency anaemia in women with heavy menstrual bleeding. Advances in Therapy, 2021; 38(1): 201-225. https://doi.org/10.1007/s12325-020-01564-y.
- Van der Meij E, Emanuel M. Hysterectomy for heavy menstrual bleeding. Women`s Health, 2016; 12(1): 63-69. Doi:10.2217/whe.15.87.
- Polite FG, DeAgostino-Kelly M, Marchand GJ. Combination of laparoscopic salpingectomy and endometrial ablation: a potentially underused procedure. J Gynecol Surg, 2021; 37(1): 1-5. https://doi.org/10.1089/gyn.2020.0097.
- Hicks-Courant KD. Growth in salpingectomy rates in the United States since 2000. Am J Obstet Gynecol, 2016; 215: 666.
- Madsen C, Baandrup L, Dehlendorff C, Kjaer SK. Tubal ligation and salpingectomy and the risk of epithelial ovarian cancer and borderline ovarian tumours: A nationwide case-control study. Acta Obstet Gynecol Scand, 2015; 94: 86.
- Daly MB, Dresher CW, Yates MS, et al. Salpingectomy as a means to reduce ovarian cancer risk. Cancer Prev Res, 2015; 8: 342.
- Most Bailey V. Hospitals lack effective cost reduction programs, survey finds. TechTarget. REVCYCLE INTELLIGENCE, 2022.

