Extended-Spectrum Beta-Lactamase – Producing Enterobacteriaceae Causing Urinary Tract Infections in Children in Qatar
Mahmoud Alhandi Omar Helal MD1,2*, Khalid Al Ansari3,4 and Colin Powell3,5
1Division of Pediatric Emergency Medicine, Department of Pediatrics, Hamad Medical Corporation, Qatar
2Pediatric Nephrology Department, Aleppo University, Faculty of Medicine, Syria
3Emergency Department, Sidra Medicine, Doha, Qatar
4Weill Cornell Medical College, Cornell University, Doha, Qatar
5School of Medicine, Cardiff University, Cardiff, UK
Received Date: 02/02/2023; Published Date: 13/03/2023
*Corresponding author: Mahmoud Alhandi Omar Helal, MD. Department of Paediatric, Hamad Medical Corporation, PO Box 3050, Doha, Qatar
Abstract
Objectives: Urinary Tract Infections (UTI) in children are most frequently due to Enterobacteriaceae. Multidrug-resistant Escherichia coli including Extended-Spectrum Beta-Lactamase (ESBL) producing organisms are becoming more prevalent. The aim of this study was to describe a cohort of children with ESBL producing organism urinary tract infections and the organism susceptibility patterns.
Methods: This retrospective study evaluated a cohort of children with ESBL- induced UTI, admitted to our Pediatric Emergency Centre during a 2.5-years period.
Results: In a total of 633 patients with urinary tract infection, 115 (18.2%) grew Gram-negative urinary isolates with an ESBL strain. Among of them (80%) female, (25.2%) had urinary tract abnormalities and (4.3%) had neuromuscular disorders. The most common bacteria were E coli (77.4%) then Klebsiella pneumonia (14.8%). All of the ESBL organisms were sensitive to carbapenems, with 98.7% sensitive to Amikacin, and 83% sensitive to Gentamicin. Gentamicin was used in (56.5%), Amikacin (23.5%) and Ertapenem/Meropenem (20.0%) of cases. The duration of treatment was 5-7 days but two cases relapsed.
Conclusions: The proportion of urinary tract infection induced by ESBL organisms was almost 1 in 5 of patients. Carbapenems and aminoglycoside remained the corner stone in treatment of the urinary tract infection by ESBL produced organisms with very high efficacy, most cases responded to treatment within 5-7 days of intravenous single antibiotic.
Keywords: Extended spectrum beta –lactamase; Urinary Tract Infection in children; Aminoglycoside
Abbreviations: UTI: Urinary Tract Infections; ESBL: Extended Spectrum Beta Lactamase
Introduction
Urinary Tract Infections (UTIs) are the most common bacterial infections in paediatric practice. The emergence of multi resistant extended-spectrum β-lactamase–producing Enterobacteriaceae (ESBL) as a cause of UTI is a major concern because therapeutic options are limited.
The World Health Organization and the European Commission have recognized the importance of studying the emergence and determinants of acquired anti-microbial resistance and the need to initiate appropriate strategies for their control [1]. In particular, the ESBL-producing Escherichia coli are emerging worldwide. The ESBL-producing strains are becoming resistant to most of the oral and intravenous antibiotics. Furthermore, they are often cross-resistant to trimethoprim/sulfamethoxazole and quinolones. This combination of properties can significantly affect the course and outcomes of infections, both in the community and in the hospital setting. International guidelines emphasize oral antibiotics as first-line treatment of UTIs in children [2]. There are no oral antibiotics for first-line treatment is active against ESBL and there are few intravenous antibiotics options. Carbapenems remain the standard treatment for severe infections due to ESBL [3], but uncontrolled use of carbapenems has led to the emergence of carbapenemas producing Enterobacteriacae which are resistant to many antibiotics.
Reserving carbapenems when alternative treatment exists is a therapeutic challenge. Recent French guidelines recommend amikacin as a first-line treatment after reviewing the increase in prevalence of ESBL strains and the need to spare the carbapenems. In this study, we describe the patients with an ESBL- producing urinary tract infection in children hospitalized from a paediatric emergency department and characterize the antibiotic susceptibility patterns of these organisms and compare the antibiotic choices along with duration of treatment.
Materials and Methods
Study design: A retrospective cohort study
Study setting: Pediatric Emergency Department (PED) at Hamad General Hospital in Qatar state, which is the main PED in Qatar state which has 4 stations all over Doha city connected to each other by electronic systems (Cerner TM) for documentations, with annual patients visiting of average 335,000 and also providing primary care.
Study duration: January 2015 to August 2017
Patient identification: All patients who had a microbiological diagnosis of UTI, using the electronic medical records (Cerner), over that time period.
Microbiological methods: The method for assessment of ESBL production is Phoenix instrument with E-test for confirmation. The Phoenix has a built-in algorithm that flags isolates as potential ESBL producers and this is confirmed phenotypically by using E-test strips that contain ceftazidime and cefotaxime with and without clavulanic acid. Antibiotic susceptibility testing was conducted by using the Clinical and Laboratory Standards Institute cut off method. Antibiotic susceptibilities of the ESBL organisms obtained were assessed.
Clinical demographics:
Patient characteristics evaluated for ESBL risk were extracted from the institution's electronic patient records.
a. Pediatric patients who presented with symptoms and signs suggested of urinary tract infections or
b. Nonspecific complaints and were diagnosed as UTI with urine cultures growing Gram-negative bacteria
Results
There were 633 patients who visited our PED with symptoms suggestive of UTI who had positive urine cultures. 115 out of total 633 (18%) urine samples found to be ESBL. They were admitted to hospital for treatment with intravenous (IV) antibiotics. None of these 115 patients were sick and all of them received the first dose of the antibiotic in the hospital then completed the IV course of antibiotics in the antibiotic clinic as outpatients.
During the period from 2015 to 2017, over 800.000 paediatric patients visited the PED. A total of 633 patients identified to have urinary tract infection, Urinary Tract Infection (UTI) is defined as positive leucocyte esterase or nitrite by urine dipstick or >5 WBCs/hpf or ≥ 5 × 104 colonies/mL in a catheterized urine specimen or, in older children, by clean catch specimens with ≥ 105 colonies/mL. All urine cultures (633) grew Gram-negative organisms. The proportion of patients with ESBL-producing isolates was 115 (18%) cases out of total number of patients with UTI (633).
Most of the ESBL organisms isolated were sensitive to carbapenems (100%), Amikacin (98.7%). Gentamicin was used in (56.5%), amikacin (23.5%) and ertapenem/ meropenem (20%). Two cases had 2nd UTI with the same initial bacteria (E-coli and K. Pneumoniae) within one month from treatment and were treated successfully. Fever was identified in 23 cases (26.45%) on presentation, abdominal pain in 21 cases (24.15%), urinary symptoms in 77 cases (67.3%), and poor feeding with irritability especially between infants 8 cases (6.9%). There were (25.21%) of patients known to have urinary tract abnormalities and (4.34%) had neuromuscular disorders.
Table1: Characteristics of a cohort with ESBL urinary tract infection.
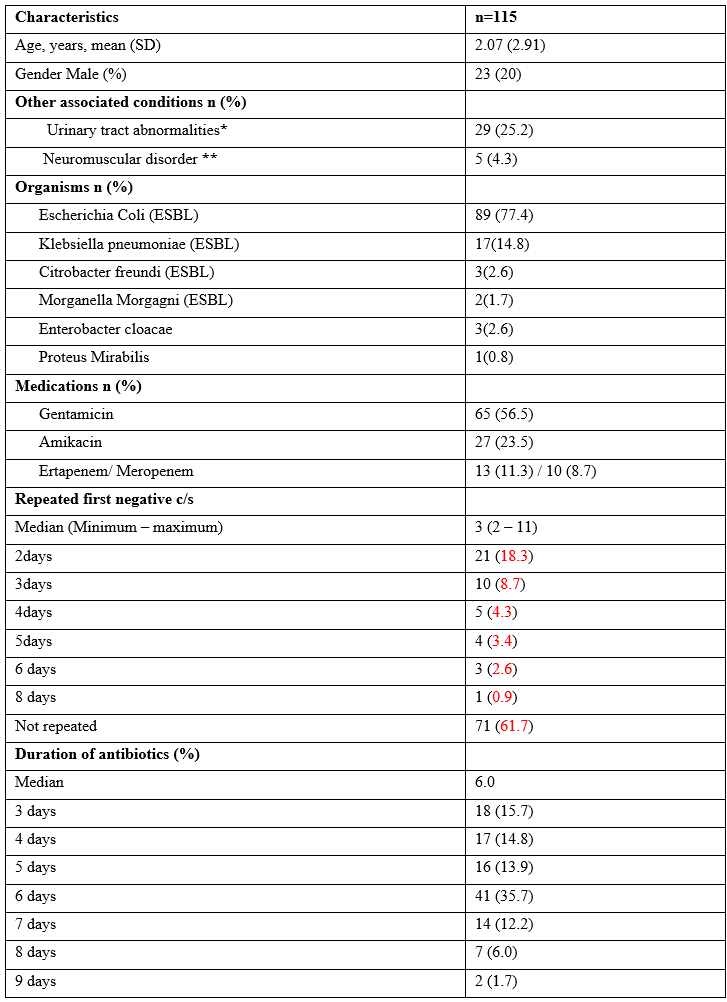
*Urinary Abnormalities-Ureterocele, left side hydro nephrosis, Vesico-ureteric reflux, bilateral hydro nephrosis with VUR, ectopic kidney, unilateral mild nephron calcinosis, multi cystic kidney
**Neuro muscular-spina bifida with cyst, Microcephaly
Discussion
Our study suggests that amikacin could be the drug of choice for UTIs due to ESBL in children. Furthermore, amikacin can be administrated as a daily single dose. Moreover, pharmacokinetics and pharmacodynamics of aminoglycosides, in particular their reduced bile and digestive elimination suggest a lower impact on intestinal flora [4]. Carbapenems are considered the most reliable treatment for infections caused by ESBL-producing bacteria as we mentioned above [5]. Despite their utility, resistance has emerged, which has led to finding alternative antibiotics for UTIs. Han et al. recently described their positive retrospective experience with aminoglycosides in UTIs due to ESBL-E [6]. The daily administration of an aminoglycoside with 30-min IV infusion for average 5 days has been shown to promote tissue diffusion and renal concentration while limiting renal and hearing toxicity [7]. Nitrofurantoin and Fosfomycin are commonly used to treat cystitis in adults [8] but there are no data on their efficiency in UTI by ESBL in children. The tolerance of nitrofurantoin needs to be investigated further in children [5].
In our cohort, the susceptibility pattern of isolated ESBL was similar to that found in hospitals from Northwest England and North Wales between 2007 and 2012 [9]. In the Study for Monitoring Antimicrobial Resistance Trends (SMART) in Canada and the United States, susceptibility to amikacin remained high, between 95.4% and 100% [10]. This variability in antimicrobial susceptibility patterns among ESBLs between studies depends on local epidemiology according to the levels and types of plasmid-mediated resistance genes
One limitation of the study is that 60% of patients did not have their urine cultured after finished the antibiotic course. These patients were followed up by telephone and by tracked electronically for an unexpected PED visit for urine related complaints over the 2 weeks following the initial infection. Only 2 children had prolonged urinary symptoms but none had side effects.
Conclusion
The emergence of extended-spectrum β-lactamase – producing Enterobacteriaceae (ESBL) as a cause of UTI presents could become a serious problem. We believe that amikacin should increasingly play a key role in the therapy of UTI due to ESBL in children, hence avoiding the use of carbapenems. Most cases can be treated for 5-7 days effectively and without any side effects.
Acknowledgments: We acknowledge Medical Research Centre at Hamad Medical Corporation, and Abdulaziz Mahmoud Helal, for their support.
Authors’ contributions:
MAOH. And KA. Designed the study;
MAOH. And CP. collected data;
MAOH. And CP. analysed the data;
MAOH, KA. And CP. wrote the main manuscript.
All authors reviewed and agreed to the published version of the manuscript.
Funding: No Funding
Availability of data and materials: All data generated or analysed during this study are included in this article. Further inquiries can be directed to the corresponding author.
Declarations
Ethics approval and consent to participate: This study was approved by the Institutional Review Board (IRB) of the Medical Research Center at Hamad Medical Corporation.
Consent for publication: Not applicable.
Competing interests: The authors declare no conflict of interest.
References
- World Health Organization. Report on infectious diseases 2000: overcoming antimicrobial resistance, 2000.
- Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management, Roberts KB. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infants and children 2 to 24 months. Paediatrics, 2011; 128: 595–610. https:// doi.org/10.1542/peds.2011-1330 PMID: 21873693
- Paterson DL. Recommendation for treatment of severe infections caused by Enterobacteriaceae producing extended-spectrum beta-lactamases (ESBLs). Clin. Microbiol. Infect, 2000; 6: 460–463.
- Craig WA. Optimizing aminoglycoside use. Crit Care Clin, 2011; 27: 107–121. https://doi.org/10.1016/j. ccc.2010.11.006 PMID: 21144989
- Sanchez GV, Baird AMG, Karlowsky JA, et al. Nitrofirantoin retains antimicrobial activity against multidrug-resistant urinary Escherichia coli from US outpatients. J Antimicrob Chemother, 2014; 69: 3259–3262. https://doi.org/10.1093/jac/dku282 PMID: 25063776
- Han SB, Lee SC, Lee SY, Jeong DC, Kang JH. Aminoglycoside therapy for childhood urinary tract infection due to extended-spectrum β-lactamase-producing Escherichia coli or Klebsiella pneumoniae. BMC Infect Dis, 2015; 15: 414. https://doi.org/10.1186/s12879-015-1153-z PMID: 26464143
- ANSM (Agence nationale de se´curite´ du me´dicament et des produits de sante´). Mise au point sur le bon usage des aminosides administre´s par voie injectable: gentamicine, tobramycine, ne´. [tilmicine, amikacine Internet], 2011.
- Falagas ME, Vouloumanou EK, Togias AG, et al. Fosfomycin versus other antibiotics for the treatment of cystitis: a meta-analysis of randomized controlled trials. J Antimicrobial Chemother. 2010; 65: 1862–1877.
- Drew RJ, Ormandy EE, Ball K, Lambert SE, Paulus S, Williams NJ et al. Antimicrobial Susceptibility Patterns Among Extended-Spectrum β-Lactamase-Producing Enterobacteriaceae in a Large Pediatric Hospital in the United Kingdom. J Pediatric Infect Dis Soc. 2015; 4: e147–150. https://doi.org/10.1093/ jpids/piu094
- Lob SH, Nicolle LE, Hoban DJ, Kazmierczak KM, Badal RE, Sahm DF, et al. Susceptibility patterns and ESBL rates of Escherichia coli from urinary tract infections in Canada and the United States, SMART 2010-2014. Diagn Microbiol Infect Dis. 2016; 85: 459–465. https://doi.org/10.1016/j.diagmicrobio.2016.04.022

