Occupational Burnout & Sleep Disorder in Nurses During the Pandemic COVID-19
Bakalis Vissarion1,*, Gkouletsa Krystallia2, Paschalidou Ioanna-Chrysa3 Tsimpida Dialechti4
1Department of Nursing, University of Thessaly, Greece
2Department of Nursing, University Hospital of Larissa Fellow, University of Thessaly, Greece
3General Hospital of Thessaloniki “Ippokrateio”, Greece
4General Hospital of Larissa, Fellow, Department of Nursing, University of Thessaly, Greece
Received Date: 17/01/2023; Published Date: 20/02/2023
*Corresponding author: Bakalis Vissarion, Department of Nursing, University of Thessaly, Greece
Abstract
Introduction: The repeated lockdowns imposed due to COVID-19 Pandemic of the last 2 years and the pressure it exerted on the health system, upset everyone’s balance, on a personal and professional level. This is also one of the reasons why Burnout is more and more common among health professionals, as a set of various symptoms. One of the most common characteristic symptoms of Burnout is that of sleep.
Purpose: Burnout, among other things, undoubtedly affects the quality of sleep. The purpose of this study was to focus and analyze the relationship between Burnout and sleep disorders experienced by nurses.
Methodology: A cross-sectional approach was used. The questionnaire was administered via the Internet. All of the participants were nursing professionals who had provided care during the COVID-19 pandemic, and data were collected between June and August 2020. Socio-demographic and work characterization instruments, the Athens Insomnia Scale, and the Maslach Burnout Inventory were used.
Results: 370 nursing professionals (nurses and nursing assistants) responded. A little more than half (52.2%) presented a sleep disorder, and 50% presented burnout. Professional category was a factor found to be associated with having a sleep disorder. Among the participants with sleep disorders, according to Athens Insomnia Scale results, all of the participants presented a high or moderate level of emotional exhaustion and a high level of burnout related to personal accomplishment.
Conclusions: According to the findings, nursing professionals experienced a high rate of burnout and sleep disorders during the COVID-19 pandemic. The findings point to the significance of identifying and evaluating the frequency of sleep disorders as well as professional exhaustion. It is necessary to develop interventions with the goals of improving these professionals' working conditions and the quality of their sleep.
Keywords: Burnout; Work exhaustion; Quality of sleep
Introduction
Burnout has been extensively studied by many researchers over the years. However, the first report was recorded in 1974 by the German psychiatrist-psychotherapist Freudenberger and was about burnout among mental health workers [1]. The exhausted worker is paralleled as a candle whose flame flickers just before going out. Thus, this condition was characterized as "inability to perform or burnout due to excessive demands on the individual's energy, strength, or capabilities."
In 2019, the World Health Organization (WHO) recognized Burnout as a professional phenomenon. The Covid-19 pandemic and the lockdowns had a drastic influence on people's professional and personal lives, but also on the working environment in general. For this reason, more and more studies are being conducted in order to ascertain the opinions of citizen-professionals, regarding burnout, the factors that contribute to it and the effects on the organization, always taking into account the pandemic.
The problem of Burnout consists of a wide range of effects on the health professional [2,3]. Thus, as a result we have the loss of professional interest and job satisfaction, a decrease in professional performance and efficiency, culminating in mental and physical exhaustion. As a result, the employee forms a negative image of himself and his self-esteem is affected. Of course, physical symptoms also make their presence felt, such as overfatigue, general exhaustion, frequent headaches and migraines, insomnia, various musculoskeletal problems, gastrointestinal disorders and so much more [4].
This particular syndrome has high rates of occurrence with frequent reference in the field of health professionals, such as nurses. More specifically, we would say that nurses are more prone to chronic work stress due to the high level of interpersonal relationships and emotions that develop with colleagues and patients. It could be said that due to the fact that they are closer and in constant contact with the patient and his relatives, resulting in their emotional involvement and in many cases the blurring of the dividing line between personal and professional contact [5,6].
One of the main, most intense and early symptoms of Burnout is sleep disturbances. These may be due to psychological (stress) and organic factors. For example, the increased adrenaline, due to the nature and situations created during a schedule, the many and alternating shifts and working hours ascertained contribute to the change and disruption of the circadian rhythm. Nurses spend their days off work mainly trying to make up for lost sleep and rebuilding their strength [7-10].
A quality sleep contributes to concentration, easier learning, good memory, as well as good metabolism and a fairly good immune and cardiovascular system, giving a more general well-being. On the contrary, poor sleep quality is responsible for the lack of concentration, thus greater susceptibility to causing accidents and serious consequences for the quality of the services provided to the patient, with the possibility of serious nursing errors with all the ramifications at the legal and moral level, the triggering of psychiatric diseases, mental and physical fatigue, etc. [11-13]. Poor sleep quality, which is due to Burnout, has an impact on the emotional and mental health of the professional nurse, thus inevitably also on his performance in the face of any professional demands and not only that.
At this point it should be mentioned that female nurses are at greater risk of heart disease, metabolic problems, hypertension and disorders related to diabetes [14]. There is new research from Columbia University, which was published on November 24, 2021, and which deals with the impact of sleep deprivation on healthcare professionals during the Covid-19 pandemic and the disruption it causes to their mental health [15]. As a result of this research, healthcare professionals who reported poor quality sleep were twice as likely to experience symptoms of depression, 50% more likely to experience psychological distress and 70% more likely to experience anxiety, compared to those who had better quality rest [15].
This array of problems presented to health professionals is capable of exacerbating the already existing problems in the health sector. In particular, the departure - resignation of a large percentage of professionals due to increased psychological pressure which they felt from the very first period of the onset of the pandemic, leads the respective health system to even greater pressure. By extension, this results in employees who remain in their positions working more shift-hours, with greater stress, thus less quality hours of sleep and rest [15].
Undoubtedly, the good functioning of the human body is based on good rest, a good and quality sleep, which helps to balance the mind and body properly. This sequence is disrupted when the employee is in Burnout. Sleep disorders, which are intertwined with the existence of Burnout, are among the most common among health professionals and especially among those who work in a cyclical schedule and it affects everyone, regardless of age. Of course, it should be noted that the more years of work someone has, the more often sleep disorders appear during the 24 hours, such as sleepiness, which is one of the most common disorders [16].
Fatigue due to lack of sleep, especially the absence of a night's rest, leads the professional to frustration and makes him less efficient. According to studies that have been done, the primary concern for a person's health should be proper and quality sleep and adequate rest [16].
Burnout symptoms are often underestimated by professionals. They try to solve any problems they find, alone, without medical or psychological help from an expert. The wrong attempt at "self-healing" most often results in the worsening of symptoms and their progression into chronic serious problems with multi-level consequences both on the health of the health professional and on the services, he provides [8,17].
Purpose
Burnout, among other things, undoubtedly affects the quality of sleep. The purpose of this study was to focus and analyze the relationship between Burnout and sleep disorders experienced by nurses.
Methodology
This was a cross-sectional, quantitative study. The selection of participants was non-probabilistic and was carried out using an online questionnaire. Inclusion criteria for the study were: 18 years of age or older and employed as a nurse or nurse's aide working in the provision of care during the COVID-19 pandemic.
Between June and August 2022, participants were invited by posting invitations to groups and communities on a variety of social media platforms spread across the nation. Participants were enrolled as participants in this study after agreeing to sign a digital consent form and receiving an invitation to the study via email. The questionnaire was then made available to the participants. The snowball method was used to distribute the online questionnaire, and after participating, each participant was asked to spread the study further.
Statistical analysis
Data was extracted from Google Forms directly into a Microsoft Excel spreadsheet and double-checked for accuracy. After the elimination of incomplete questionnaires, the data were transferred to the SPSS 25 software. The data were processed using descriptive statistics. The reliability of the instruments used was assessed using Cronbach's alpha coefficient, with coefficients in the range 0–1 and values equal to or greater than 0.70 indicating reliability.
The Chi-square test was used to compare the qualitative variables of the Maslach Burnout Inventory (MBI) and the Athens Insomnia Scale (AIS).
Results are presented using the means of the estimates derived from the adjusted prevalence ratio with their corresponding 95% confidence intervals and p values, considering a significance level of 5% (p < 0.05).
Results
A total of 370 professional nurses completed the questionnaire, of which 325 (87.8%) were female and 45 were male (12.2%), with 31.6% belonging to the 36-40 age group. In addition, 61.6% of the participants were married, 58.8% were permanent employees, 32.4% had a TE degree and 25.9% had 11-15 years of experience.
52.2% of the respondents characterized the duration of their sleep as slightly insufficient. Even 43.5% reported a slightly reduced feeling of well-being during the day. Finally, 58.4% suffer from mild daytime sleepiness.
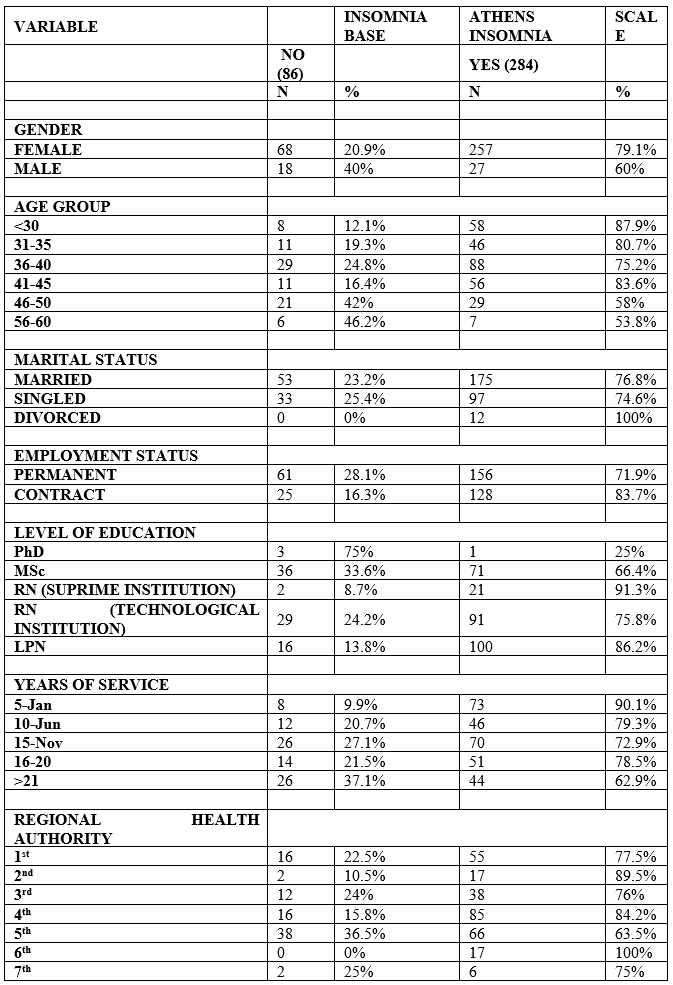
The prevalence of sleep disorders assessed using AIS was 76.8 %. Socio-demographic and occupational variables reported during the pandemic according to the occurrence of sleep disorders measured through the AIS are presented in Table 1.
Table 1: Distribution of socio-demographic and occupational variables and changes reported during the pandemic according to sleep disturbances measured using the Athens Sleep Scale.
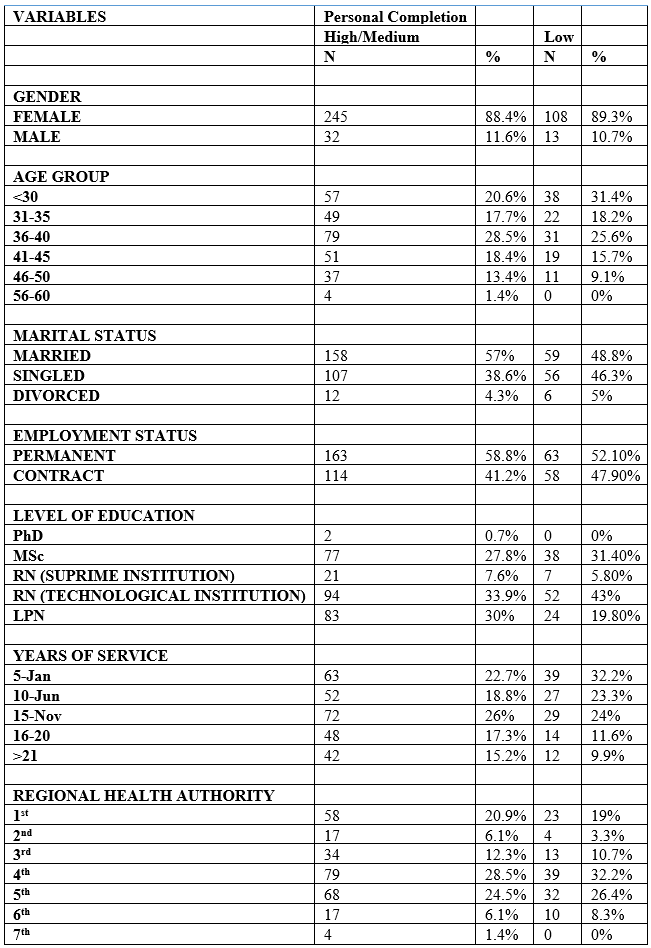
Burnout was identified in 50% of the sample. Mean MBI scores according to the Emotional Exhaustion, Depersonalization, and Personal Fulfillment subscales were 28.8 (SD = 12.7), 9.12 (SD = 6.52), and 34.9 (SD = 7.79), respectively. Regarding the thresholds established for the classification of burnout, for the Emotional Exhaustion subscale, the level was high in 50% of the participants, moderate in 25.4% and low in 24.6%. For the Depersonalization subscale, the level was high in 29.9% of participants, moderate in 44.3%, and low in 25.8%. and for the Personal Fulfillment subscale, the level was high in 32.0% of participants, moderate in 35.2%, and low in 32.7%.
Table 2: Distribution of socio-demographic and work variables and changes reported during the pandemic according to the level of burnout measured using the Maslach Burnout Inventory subscales.
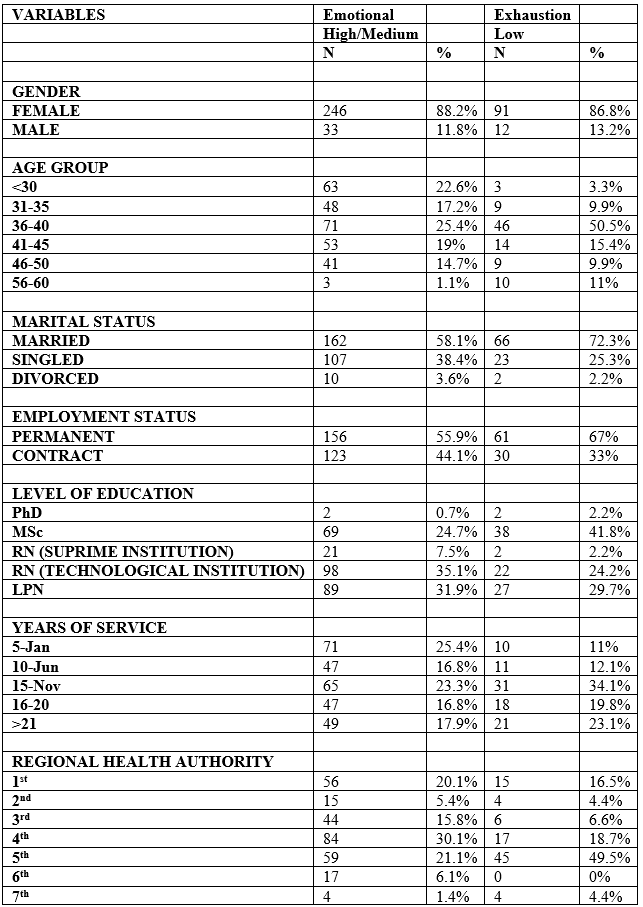
Table 3: Distribution of socio-demographic and work variables and changes reported during the pandemic according to the level of burnout measured using the Maslach Burnout Inventory subscales.
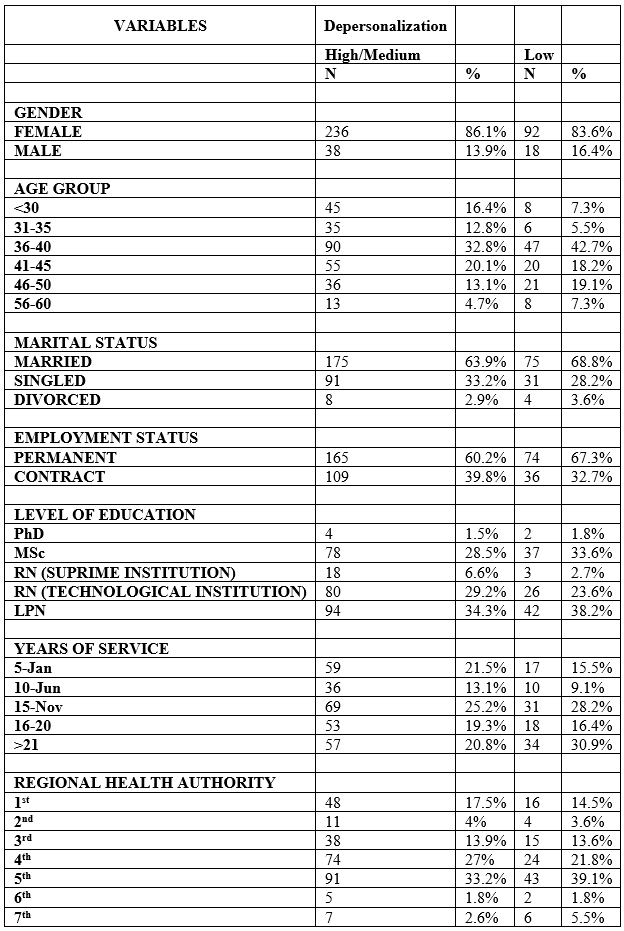
Table 4: Distribution of socio-demographic and work variables and changes reported during the pandemic according to the level of burnout measured using the Maslach Burnout Inventory subscales.
Based on the AIS, with regard to sleep disturbances, a difference was found in the level of burnout between the subscales Emotional Exhaustion, Depersonalization and Personal Fulfillment of the MBI. Among the participants with sleep disorders, all showed high and moderate levels of emotional exhaustion and high levels of related personal fulfillment.
Table 5: Distribution of subscales of the Maslach burnout inventory according to the presence of sleep disturbances measured using the Athens Insomnia Scale (N = 370).

Fatigue can rise as a result of the additional demands placed on nurses, such as an increase in care requirements and team member tension and stress. Health care workers' working conditions affect their health [18] emphasized that mental health professionals should respond to this imperative by developing appropriate methods and tools to reduce rates of post-traumatic stress, anxiety, and depression among health professionals working in the COVID pandemic -19. These conditions will assist health professionals in minimizing the negative emotions that frequently arise during the process of providing patient care. In addition, the risk of contracting COVID-19 is increased by poor sleep quality and stress brought on by direct contact between healthcare workers and the virus [19].
In this study, 76.8% of participants had scores indicative of sleep disorders, according to the AIS. In Spain, a study involving 100 healthcare workers and 70 non-healthcare workers found that insomnia developed or worsened in 57.0% of healthcare workers compared to 34.2% in group of non-health workers [20].
According to the AIS, 76.8% of participants in this study had scores that pointed to sleep disorders. Studies have shown that sleep disorders are common and that their prevalence is higher in healthcare professionals than in the general population and that, as a result of the pandemic, sleep disorders have intensified [21-24]. In a study conducted in Spain with 100 healthcare professionals and 70 non-healthcare professionals, insomnia developed or got worse in 57% of healthcare professionals, compared to 34% of non-healthcare professionals [20].
In addition to sleep disorders, poor sleep quality is described as common among healthcare professionals [25,26]. An important finding of this study is that most participants reported poor sleep quality, with a higher prevalence among nursing assistants. This situation may be due to the characteristics of the activities performed by these professionals, together with the precarious labor market [27].
Nursing assistants are more likely to develop sleep problems because of the nature of their work, which includes prolonged and continuous work in close proximity to patients, numerous and exhausting work shifts, low levels of autonomy, dissatisfaction with work responsibilities, and a lack of preparation to deal with emotional issues. However, due to the small number of participants in these occupational categories (particularly nursing assistants) included in this study, caution should be exercised regarding this finding. However, this study's findings suggest that nursing assistants may encounter even more issues than nurses, highlighting the significance of further research into this group of workers.
Sleep was self-rated as poor or very poor by 52.2% of participants. Other studies have reported a similar finding, viz. For example, poor quality sleep has been identified in 77.4% of nurses [25] and 64.0% of healthcare professionals experienced poor sleep quality compared to 31.0% in a group of non-workers [20]. Poor sleep quality and sleep disturbances are important health indicators that can affect the quality of care and increase the risk of errors [28], as well as negatively affect the team. In addition, occupational demands are frequent causes of insufficient sleep and may increase the risk of occupational accidents [29].
In addition, burnout was identified in 50% of the participants and, when analyzing the mean scores for the MBI subscales, it was observed that they showed a high level of burnout in emotional exhaustion (28.8), a moderate level in depersonalization (9.1), and a high level of personal fulfillment (34.9). Exhaustion, negative attitudes, dissatisfaction with their performance, physical symptoms and insomnia are commonly reported by workers with burnout syndrome [27]. [30] found a high level of pandemic-related burnout among healthcare workers, with less personal and professional burnout for the support group, which included nursing assistants. Pursuing a professional activity should be a source of satisfaction and confirm the importance of that person's role in society. However, high workload and different levels of stress can negatively affect the health of nurses leading to burnout [31,32].
Limitations
This study is subject to several limitations. The first was that the cross-sectional design that was used doesn't let you look at variables over time or how they relate to each other. The second was that self-report instruments, which may be less accurate at identifying symptoms, were used to assess sleep disturbances as well as physical and emotional exhaustion. In addition, no primary sleep disorder-related questions were posed to participants.
Conclusion
A significant number of the nurses who participated in this study were found to suffer from burnout and sleep disturbances. According to the Athens Insomnia Scale, occupational categories were associated with sleep disorders, with nurses having a lower prevalence of disorders than nursing assistants.
During abnormal times like the current pandemic, nurses, particularly nursing assistants, should have their sleep disturbances and burnout assessed on a regular basis. In addition, professional nurses' physical and mental health should be improved and the quality of care maintained by implementing interventions to improve the work environment and sleep quality. It is essential to disseminate information and guidance on sleep issues and burnout, as well as their effects on nurses. It is also important to recommend preventative measures, keep an eye out for early signs and symptoms, offer advice on how to change one's lifestyle, and refer patients for treatment when it is necessary.
References
- Bradley HB. Community-based Treatment for Young Adult Offenders. 2016; 15(3): 359–370. Http://Dx.Doi.Org/10.1177/001112876901500307.
- Cañadas-De la Fuente GA, Vargas C, San Luis C, García I, Cañadas GR, de la Fuente EI. Risk factors and prevalence of burnout syndrome in the nursing profession. International Journal of Nursing Studies, 2015; 52(1): 240–249. https://doi.org/10.1016/J.IJNURSTU.2014.07.001
- Molina-Praena J, Ramirez-Baena L, Gómez-Urquiza JL, Cañadas GR, de la Fuente EI, Cañadas-De la Fuente GA. Levels of Burnout and Risk Factors in Medical Area Nurses: A Meta-Analytic Study. International Journal of Environmental Research and Public Health, 2018; 15(12). https://doi.org/10.3390/IJERPH15122800
- Liamou Ε. Burnout and the covid-19 health crisis, 2022.
- Gómez-Urquiza JL, Monsalve-Reyes CS, San Luis-Costas C, Fernández-Castillo R, Aguayo-Estremera R, Cañadas-de la Fuente GA. Factores de riesgo y niveles de burnout enenfermeras de atenciónprimaria: unarevisiónsistemática. Atención Primaria, 2017; 49(2): 77–85. https://doi.org/10.1016/J.APRIM.2016.05.004
- Membrive-Jiménez MJ, Gómez-Urquiza JL, Suleiman-Martos N, Velando-Soriano A, Ariza T, de la Fuente-Solana EI, et al. Relation between Burnout and Sleep Problems in Nurses: A Systematic Review with Meta-Analysis. Healthcare (Basel, Switzerland), 2022; 10(5). https://doi.org/10.3390/HEALTHCARE10050954
- Ghazwin MY, Kavian M, Ahmadloo M, Jarchi A, Javadi SG, Latifi S, et al. The Association between Life Satisfaction and the Extent of Depression, Anxiety and Stress among Iranian Nurses: A Multicenter Survey. Iranian Journal of Psychiatry, 2016; 11(2): 120. /pmc/articles/PMC4947220/
- Hsieh ML, Li YM, Chang ET, Lai HL, Wang WH, Wang SC. Sleep disorder in Taiwanese nurses: a random sample survey. Nursing & Health Sciences, 2011; 13(4): 468–474. https://doi.org/10.1111/J.1442-2018.2011.00641.X
- Huang CLC, Wu MP, Ho CH, Wang JJ. Risks of treated anxiety, depression, and insomnia among nurses: A nationwide longitudinal cohort study. PloS One, 2018; 13(9). https://doi.org/10.1371/JOURNAL.PONE.0204224
- Jacobsen HB, Reme SE, Sembajwe G, Hopcia K, Stoddard AM, Kenwood C, et al. Work-family conflict, psychological distress, and sleep deficiency among patient care workers. Workplace Health & Safety, 2014; 62(7): 282–291. https://doi.org/10.1177/216507991406200703
- Eanes L. CE: The potential effects of sleep loss on a nurse’s health. The American Journal of Nursing, 2015; 115(4): 34–40. https://doi.org/10.1097/01.NAJ.0000463025.42388.10
- Kemper KJ, Mo X, Khayat R. Are Mindfulness and Self-Compassion Associated with Sleep and Resilience in Health Professionals? Journal of Alternative and Complementary Medicine (New York, N.Y.), 2015; 21(8): 496–503. https://doi.org/10.1089/ACM.2014.0281
- Zhang Y, Duffy JF, de Castillero ER. Do sleep disturbances mediate the association between work-family conflict and depressive symptoms among nurses? A cross-sectional study. Journal of Psychiatric and Mental Health Nursing, 2017; 24(8): 620. https://doi.org/10.1111/JPM.12409.
- Zhang C, Tait C, Minacapelli CD, Bhurwal A, Gupta K, Amin R, et al. The Role of Race, Sex, and Age in Circadian Disruption and Metabolic Disorders. Gastro Hep Advances, 2022; 1(3): 471–479. https://doi.org/10.1016/J.GASTHA.2022.02.015
- Diaz F, Cornelius T, Bramley S, Venner H, Shaw K, Dong M, et al. The association between sleep and psychological distress among New York City healthcare workers during the COVID-19 pandemic. Journal of Affective Disorders, 2022; 298: 618–624. https://doi.org/10.1016/J.JAD.2021.10.033
- Młynarska A, Bronder M, Kolarczyk E, Manulik S, Młynarski R. Determinants of Sleep Disorders and Occupational Burnout among Nurses: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 2022; 19(10). https://doi.org/10.3390/IJERPH19106218
- Stewart NH, Arora VM. The Impact of Sleep and Circadian Disorders on Physician Burnout. Chest, 2019; 156(5): 1022–1030. https://doi.org/10.1016/J.CHEST.2019.07.008
- Horesh D, Brown AD. Traumatic stress in the age of COVID-19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy, 2020; 12(4): 331–335. https://doi.org/10.1037/tra0000592
- Wang S, Xie L, Xu Y, Yu S, Yao B, Xiang D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occupational Medicine, 2020; 70(5): 364–369. https://doi.org/10.1093/occmed/kqaa074
- Herrero San Martin A, Parra Serrano J, Diaz Cambriles T, Arias Arias EM, Muñoz Méndez J, del Yerro Álvarez MJ, et al. Sleep characteristics in health workers exposed to the COVID-19 pandemic. Sleep Medicine, 2020; 75: 388–394. https://doi.org/10.1016/j.sleep.2020.08.013
- Aydin Sayilan A, Kulakaç N, Uzun S. Burnout levels and sleep quality of COVID‐19 heroes. Perspectives in Psychiatric Care, 2021; 57(3): 1231–1236. https://doi.org/10.1111/ppc.12678
- Beck F, Léger D, Fressard L, Peretti‐Watel P, Verger P. Covid‐19 health crisis and lockdown associated with high level of sleep complaints and hypnotic uptake at the population level. Journal of Sleep Research, 2021; 30(1). https://doi.org/10.1111/jsr.13119
- Qiu D, Yu Y, Li RQ, Li YL, Xiao SY. Prevalence of sleep disturbances in Chinese healthcare professionals: a systematic review and meta-analysis. Sleep Medicine, 2020; 67: 258–266. https://doi.org/10.1016/j.sleep.2019.01.047
- Salari N, Khazaie H, Hosseinian-Far A, Ghasemi H, Mohammadi M, Shohaimi S, et al. The prevalence of sleep disturbances among physicians and nurses facing the COVID-19 patients: a systematic review and meta-analysis. Globalization and Health, 2020; 16(1): 92. https://doi.org/10.1186/s12992-020-00620-0
- Khatony A, Zakiei A, Khazaie H, Rezaei M, Janatolmakan M. International Nursing. Nursing Administration Quarterly, 2020; 44(1): E1–E10. https://doi.org/10.1097/NAQ.0000000000000397
- Zeng LN, Yang Y, Wang C, Li XH, Xiang YF, Hall BJ, et al. Prevalence of Poor Sleep Quality in Nursing Staff: A Meta-Analysis of Observational Studies. BehavioralSleepMedicine, 2020; 18(6): 746–759. https://doi.org/10.1080/15402002.2019.1677233
- Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, Andrade SM de. Physical, psychological and occupational consequences of job burnout: A systematic review of prospective studies. PLOS ONE, 2017; 12(10): e0185781. https://doi.org/10.1371/journal.pone.0185781
- Weaver AL, Stutzman SE, Supnet C, Olson DM. Sleep quality, but not quantity, is associated with self-perceived minor error rates among emergency department nurses. International Emergency Nursing, 2016; 25: 48–52. https://doi.org/10.1016/j.ienj.2015.08.003
- Mukherjee S, Patel SR, Kales SN, Ayas NT, Strohl KP, Gozal D, et al. An Official American Thoracic Society Statement: The Importance of Healthy Sleep. Recommendations and Future Priorities. American Journal of Respiratory and Critical Care Medicine, 2015; 191(12): 1450–1458. https://doi.org/10.1164/rccm.201504-0767ST
- Kulkarni A, Khasne RW, Dhakulkar BS, Mahajan HC. Burnout among Healthcare Workers during COVID-19 Pandemic in India: Results of a Questionnaire-based Survey. Indian Journal of Critical Care Medicine, 2020; 24(8): 664–671. https://doi.org/10.5005/jp-journals-10071-23518
- Nogueira L de S, Sousa RMC de, Guedes E de S, Santos MA dos, Turrini RNT, Cruz D de A L M da. Burnout and nursing work environment in public health institutions. RevistaBrasileira de Enfermagem, 2018; 71(2): 336–342. https://doi.org/10.1590/0034-7167-2016-0524
- Silva R M da, Vieira LJE de S, Garcia Filho C, Bezerra IC, Cavalcante AN, BorbaNetto FC de, et al. Precarização do mercado de trabalho de auxiliares e técnicos de Enfermagem no Ceará, Brasil. Ciência&SaúdeColetiva, 2020; 25(1): 135–145. https://doi.org/10.1590/1413-81232020251.28902019

