Implementation of an Evidence-Based Group Treatment Protocol in Adult Inpatient Settings: Seeking the Triple Aim
Bradley C Riemann, Rachel C Leonard1,*, Jessica A Cook1, Lynsey R Miron2, Brenda E Bailey1, Dalton L Kick1, Brian C Kay1 and Jerry L Halverson1
1Department of Behavioral Health, Rogers Behavioral Health, USA
2Department of Behavioral Health, University of St. Thomas, Morrison Family College of Health, USA
Received Date: 01/11/2022; Published Date: 16/11/2022
*Corresponding author: Rachel C Leonard, PhD, Department of Behavioral Health, Rogers Behavioral Health, 34700 Valley Road, Oconomowoc, WI, 53066, USA
Abstract
Objective: The Triple Aim initiative seeks improvements in patient experience and health while reducing cost. This mandate presents unique challenges for psychiatric inpatient units due to necessary high staffing levels and short lengths of stay. The objective of the current study was to determine the effects of a standard, inpatient treatment protocol on Triple Aim elements.
Methods: Cohorts of participants prior and post protocol launch were compared on a variety of Triple Aim-related metrics. Data was collected from August 2017-June 2019 on three adult inpatient psychiatric units within the same not-for-profit behavioral health system and included
7593 individuals. Of those, 1435 completed all relevant assessments and were included in the analyses. Main study measures included patient satisfaction, average length of stay, depression severity, suicide risk, clinician rated global improvement, 30-day readmission rate and cost per patient day.
Results: Comparing pre to post protocol launch, the post cohort had statistically significant increases in satisfaction with groups and likelihood to recommend and global improvement at discharge as well as reductions in depression severity, suicide risk, and average length of stay. Reductions in 30-day readmission rate as well as cost per patient day were also found but were not significant.
Conclusions: Inpatients exposed to a group-based treatment protocol experienced enhanced gains relative to previous patients in the same facilities. These gains align with the Triple Aim mandate and were achieved within lower ALOS’s.
Keywords: Inpatient; Protocol; Readmission; Satisfaction; Cost
Introduction
Nearly 10 million people receive inpatient psychiatric treatment in the United States annually and up to 170,000 on any given day [1,2]. Inpatient utilization is associated with significant cost and high readmission rates [3], calling into question the effectiveness of “traditional” inpatient treatment, which often focuses on stabilization through medical interventions and monitoring without evidence-based care or protocols to address patients’ lifetime course of illness [4]. In fact, calls to reform inpatient psychiatric care have identified need for improvement in treatment effectiveness, duration of treatment, patient risk at discharge, readmission rates, and overall cost [5]. Many of these areas are included within the Triple Aim [6], an initiative to improve healthcare consisting of three components: improving patient experience (TA1), improving health (TA2), and reducing cost (TA3). Deficits in the current system represent a critical missed opportunity to provide effective, life-saving care while mitigating the risk of rehospitalization.
Inpatient protocols using evidence-based psychotherapeutic interventions have not been widely researched or disseminated, though there is evidence that Cognitive-Behavioral Therapy (CBT) and Dialectical Behavioral Therapy (DBT) are effective for individuals experiencing an acute mental health crisis [7,8]. Discharge from inpatient hospitals also poses a critical challenge, with international estimates indicating that nearly 20% of all suicides occur in the three months following discharge [9-13]. In fact, individuals discharging from inpatient psychiatric care are at higher risk for a range of adverse outcomes including death, self-harm, committing a violent crime, and hospitalization due to interpersonal violence [14].
Providing training to inpatient staff on evidence-based interventions has also been found to improve perceptions of the treatment environment amongst those involuntarily admitted [15].
The inpatient setting provides a unique opportunity to implement intensive intervention while closely monitoring patients. The current study sought to examine the impact of a structured, empirically informed treatment protocol on identified deficiencies in inpatient treatment and consistent with goals of the TA including patient satisfaction (TA1), treatment effectiveness (TA2) and cost (TA3;[6]).
Method
Participants
A total of 7593 individuals admitted into one of three adult psychiatric inpatient units within a large not-for-profit behavioral healthcare system during the designated study period. Participants either received traditional treatment (TT; n = 1960) or the new protocol (NP; n = 5633), depending on the date and the specific inpatient unit to which they admitted (see below for additional details about the timing of new protocol implementation). Of the total admitted, 1435 provided responses on all relevant measures at admission and discharge [TT n = 186 (9.49% of pre-launch admissions)]; [NP n = 1249 (22.17% of post-launch admissions)] and therefore constitute the final study sample. The increase in retention rate for the NP group was due to data collection process improvements initiated during the study. Sex of participants was obtained via self-report. All participants consented to have data analyzed and reported in an aggregated form.
Procedure
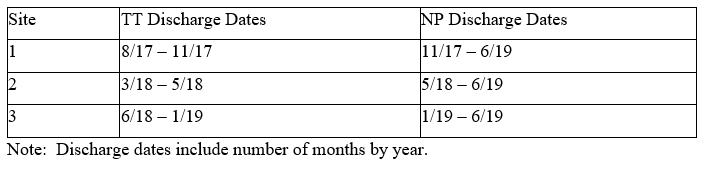
Prior to starting the NP, automated outcome data collection was initiated at each site to establish baseline data for the TT group. Sites 1, 2 and 3 collected TT data for three months, two months, and six months, respectively. Timelines were not consistent across site due to implementation factors. The NP launched first at Site 1 and was strategically spread in a staggered fashion to monitor clinical outcomes before initiating at the other locations. Date ranges for TT were determined using the date each site started collecting outcome data. See Table 1 for TT and NP data collection timelines by site.
Table 1: Data Collection Timelines by Site.
Method
Traditional Treatment (TT)
TT offered variable modes and amounts of psychosocial treatment at each site and consisted of daily psychiatry visits, social service groups, recreation therapy, optional spirituality services, access to substance-related programming (e.g., Alcoholics Anonymous) and structured and non-structured nursing support. Structured group therapy time provided by licensed staff, paraprofessionals, and other support staff varied from 4-6 hours per day across sites.
New Protocol (NP)
The NP was developed based on review of diagnoses and problems identified within the inpatient sites, and review of the literature related to identified targets. The NP includes 15 psychoeducational and skill-based groups targeting: suicide risk, non-suicidal self-injury, and distress tolerance (six groups); motivation for treatment and goal setting (three groups); depression psychoeducation and behavioral activation (three groups); and anxiety psychoeducation and CBT-based anxiety management (three groups). Five 40-50-minute groups were offered daily on a three-day rotation basis. Patients received workbooks [16] upon admission containing group material and homework assignments completed during a staff-supported 45-minute daily assignment period. The NP schedule also included daily check in/out groups. Psychiatry visits, recreation therapy, optional spirituality and substance-related services, and nursing related structured and non-structured supervised time remained consistent to TT. NP groups were led by bachelor’s prepared paraprofessionals or master’s level clinicians. Group leaders received didactic training, written training guides and structured “shadow shifts” to prepare them to deliver NP content. Ongoing, weekly supervision was also provided by a licensed psychologist familiar with the protocol. A structured fidelity monitoring process was used to ensure adherence.
Analytic Plan
Data analyses were completed in R Statistics 3.5.1 [17]. T-tests and chi-squared analyses utilized the base ‘stats’ package.
Measures
Average cost per patient day (ACPPD). ACPPD is calculated by dividing total unit staffing cost per day by the number of patients in treatment. Cost data reported are for all patients treated during designated timelines not just for study participants and aggregated across all sites.
Average length of stay (ALOS). ALOS is calculated using the number of days present on the unit between admission and discharge. Day of admission and discharge count as full days.
Clinical Global Impressions Scale – Improvement (CGI-I; [18]). The CGI-I is a 1-item clinician rating of improvement in overall condition (very much improved, much improved, minimally improved, no change, minimally worse, much worse, or very much worse) from admission to discharge [18] and was completed by the attending psychiatrist. The percentage considered very much improved is reported. The validity of the CGI-I has been questioned [19], leading to recommendations that it be used with other measurements of improvement (e.g., self-report scales), which we have included in this study.
Columbia Suicide Risk Severity Rating Scale Screener – Since Last Contact (C-SSRSS; [20]). The C-SSRSS was administered at discharge by psychiatric nurses to measure Suicidal Ideation (SI) severity and risk. This version includes six questions assessing SI, plan, and intent answered in a yes/no format, which inform characterization as low, medium, or high risk. High-risk determination is made if the patient reports SI with intent, SI with intent and plan, or history of suicidal behavior or preparation in the last 90 days. The percentage of patients in the high-risk category at discharge is reported.
Press Ganey Surveys (PGS; [21]). The PGS is a 30-item, commonly used measure of patient satisfaction and was completed by patients at discharge and sent to the measure developers to tabulate results and report them back to our institution. Two items were used for this study “likelihood I would recommend this program” and “helpfulness of group therapy”. Each item is scored on a zero to five scale. “Top Box” scores, or percentage of patients rating the item five out of five were analyzed for this study.
Quick Inventory of Depressive Symptomatology – Self-Report (QIDS-SR; [22]). The QIDS-SR is a 16-item self-report measure of depression severity. Scores range from 0 to 27, with higher scores indicating greater depression severity. Zero to five is considered “no depression”, six to 10 “mild”, 11-15 “moderate”, 16-20 “severe” and 21 or greater “very severe”. The QIDS-SR was completed within 24 hours of admission and discharge. The QIDS-SR has demonstrated acceptable psychometric properties, including validity and sensitivity to change; [23]).
Readmission rate (RR). RR is the percentage of individuals who discharged and readmitted to inpatient within the next 30 days. Two RR’s are reported.
RR1. RR1 is the percentage of individuals who readmitted to one of the study inpatient units.
RR2. RR2 is the percentage of individuals who readmitted to any inpatient facility based on a rolling 12-month Medicare claims data quarterly report provided by Lake Superior Quality Network (LSQN). It is important to note that date ranges of the LSQN data do not align with other dates reported herein and were non-modifiable. All data provided by LSQN was rounded to one decimal point prior to our institution receiving it.
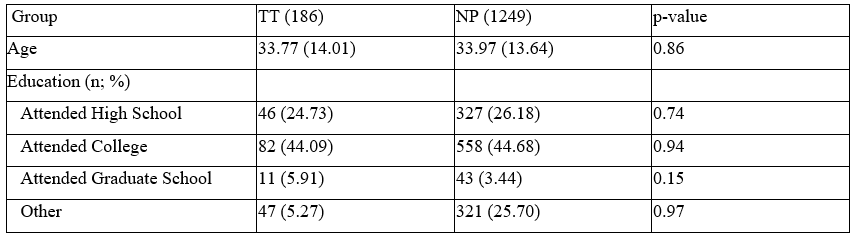
Results
Overall, 838 (58.40%) of participants self-reported as female with 597 (41.60%) reporting male. The average age was 33.94 years (SD = 13.68, range = 18-80). The majority reported as White (1199; 83.55%) with the remaining participants reporting as Black (197; 13.73%), Asian (16; 1.11%), American Indian or Alaskan Native (10; 0.70%), and Native Hawaiian or Pacific Islander (3; 0.21%). Of these participants, (84; 5.90%) identified their ethnicity as Hispanic or Latino. Data was not collected on socioeconomic status. Data by group related to age and education can be found in Table 2.
Table 2: Age and Education.
Data by group related to sex and race can be found in Table 3.
Table 3: Sex and Race.

No group differences were found except for percentage reporting White [TT = 130 (69.89%) and NP = 1069 (85.59%); χ²(1) = 27.89, p < 0.001] and Black [TT = 49 (26.34%) and NP = 148 (11.85%); χ²(1) = 27.51, p < 0.001]. Patients were diagnostically complex averaging 2.90 (SD = 1.23) diagnoses for the TT and 2.78 (SD = 1.32) for the NP group [NS; t(219) = 1.13, p = 0.258]. Differences between groups for Bipolar and Related Disorders [TT = 3 (1.61%) versus NP = 70 (5.60%), χ²(1) = 4.14, p = 0.042], Schizophrenia Spectrum and Psychotic Disorders [TT = 38 (20.43%) versus NP = 139 (11.13%), χ²(1) = 12.34, p < 0.01] and Trauma and Stress Related Disorders [TT = 56 (30.11%) versus NP = 260 (20.82%), χ²(1) = 7.62, p < 0.01] were found. See Table 4 for a summary of patients meeting criteria for major diagnostic categories by group.
Table 4: Diagnoses by Disorder Category.

Remaining results are reported separately by group and organized by Triple Aim category.
Improving Patient Experience (TA1)
Patient Satisfaction
Sample sizes varied slightly between the two items examined due to a subset completing one but not both questions. Also, sample sizes reported here are different than the overall groups due to responses being anonymous and thus not being able to separate them out from the total sample. Top Box percentage of patients that would recommend the program increased from 190 (48.13%) in the TT group (n = 396) to 989 (53.06%) in the NP group (n = 1864) and was found to be significant (χ²(4) = 19.23, p < 0.001). The percentage of patients indicating they found group therapy to be helpful also increased from 170 (42.73%) in the TT group (n = 398) to 862 (46.13%) in the NP group (n = 1868) and was found to be significant (χ²(4) = 70.06, p < 0.001).
Improving Health (TA2)
Depression severity
The NP group (M = 17.89, SD = 5.61) reported greater depression severity upon admission compared to the TT group [M = 15.97, SD = 6.10; t(234) = -2.65; p < 0.01]. The two groups did not differ, however, on discharge QIDS-SR scores with the TT group averaging 9.39 (SD=5.33) and the NP group 9.82 [SD = 5.21; t(240) = 0.85, p = 0.40]. Both groups experienced significant reductions in QIDS-SR from admission to discharge. The TT group reduced by 6.58 points [t(363) = 13.07, p < 0.01, dz = 1.08] and the NP group by 8.07 points [t(2482) = 43.30, p < 0.01, dz =1.44]. The difference in reduction from TT group to NP group was statistically significant [t(242) = -3.28, p < 0.01].
Suicide risk
Significantly fewer participants in the NP group (43; 3.44%) were rated as high risk on the C-SSRSS at discharge compared to the TT group [22 (11.83); t(202) = 3.45, p < 0.01]. It is important to note that someone could rate high risk but not be acutely unsafe. Anyone deemed a risk to themselves or others would not be discharged.
Physician-rated improvement
Psychiatrists rated 46 (24.84%) of the TT group (n = 186) as very much improved on the CGI at discharge compared to 400 (31.99%) of the NP group (n = 1249). This difference was significant [χ² (6), p = 0.04], with a greater percentage of patients in the “very much improved” category in NP than in TT.
Reducing Cost (TA3)
Average cost per patient day
ACPPD in the TT group varied depending on site due to significant variation in treatment and schedules offered. NP unit staffing grids still included some discrepancies due to the need to leverage more costly agency staff during certain NP months. Even with agency staff usage, a 3.67% decrease in ACPPD was found comparing TT to NP. This difference although financially meaningful was not statistically significant [t(18.16) = 1.13, p = 0.27].
Improving Health (TA2) and Reducing Cost (TA3)
ALOS
The TT group had a statistically longer ALOS (6.47 days; SD = 3.19), compared to the NP group [5.73 days; SD = 2.78; t(228) = 2.96, p < 0.01].
Readmission Rates
RR1
RR1 rates were 10.75% (n = 20) for the TT group compared to 6.89% (n = 86) for the NP group, which constitutes a 35.96% reduction. This difference while trending toward significance and clinically meaningful, was not statistically significant (χ² (2), p = 0.08).
RR2
LSQN reported 2016 RR2 rates (prior to NP launch at any site) were 22.0% (n = 126 out of 574). The last report received was for April 2018 to March 2019 (Sites 1 and 2 had NP for full year but Site 3 only had NP for last three months). This report indicated the RR2 was 15.7% (n = 90 out of 573), constituting a 28.6% reduction. Statistical analysis of these data were not possible as overall percentages and number of participants were the only data points made available.
Discussion
Those presenting to the inpatient level of care are in the throes of a mental health crisis and may be particularly vulnerable to adverse mental health outcomes [13,24,25]. Inpatient treatment is expensive and, unfortunately, rehospitalization within relatively short periods of time (e.g., 30-days) is also common. Therefore, it is essential that protocols are identified that maximize clinical impact.
This is in line with the Triple Aim (TA), which mandates improved patient experience (TA1) and improved health (TA2) while reducing cost (TA3; [6]). This important health care initiative presents unique challenges for psychiatric inpatient units due to necessary high staffing levels and short treatment durations. The current study sought to examine the impact of a structured, empirically informed treatment protocol (NP) on data related to the TA within a diagnostically complex sample. The NP emphasized group-based skills related to motivation for treatment engagement, safety planning, safety skills, and CBT-based anxiety and depression management. This protocol was created by a large not-for-profit behavioral health care system for use in its three Wisconsin-based, adult inpatient units. To assess the effectiveness of this protocol, patient data collected prior to the protocol implementation (TT) was compared to data collected after protocol implementation (NP). Results indicate that patients in the NP group experienced greater patient satisfaction related to two key items investigated (TA1), greater reductions in depression severity (despite higher depression levels at admission), lower suicidal risk at discharge, and higher rates of being rated by their physician at discharge as “very much improved” (TA2). This was achieved while experiencing a nonsignificant, but financially meaningful overall reduction in ACPPD (TA3), which was in part due to using paraprofessionals to lead some of the protocol groups. This cost reduction was achieved despite an aggregated inflation rate of 4.0% over the nearly two-year study period (based on Consumer Price Index; [26]) and an annual 3.0% compensation increase all staff received as part of their employee benefit package. Additionally, those in the NP group had a shorter ALOS and nonsignificant, but clinically meaningful lower 30-day readmission rates based on internal and external data (TA2 and TA3).
The NP group had more participants reporting their race as White and fewer as Black. Therefore, it is possible that factors related to culture impacted the findings. Although groups did not differ in the average number of diagnoses per participant, the NP group had a greater percentage of those diagnosed with Bipolar and Related Disorders and fewer with Schizophrenia Spectrum and Psychotic Disorders and Trauma and Stress Related Disorders. It is possible that these differences in the diagnostic makeup of the groups played a role in the superior outcomes experienced by patients in the NP group.
Future studies would benefit from examining the impact of the NP in samples with greater diagnostic and cultural diversity.
Due to the “real world” nature of this study several significant limitations exist. First, participants were not randomly assigned to TT or NP groups nor was a placebo control group utilized. Also, only those patients who completed all relevant self-report questionnaires were included, resulting in a large amount of missing data. The percentage of those “retained” in the NP group was higher indicating improvements in the process of data collection. In addition, participants in both groups had variable durations of treatment. Furthermore, uneven timelines and sample sizes also weakened the study. Also, the reduction in readmission rates reported only constitute a subset of our sample. RR1 was for all patients but only those returning to treatment within the same not-for-profit behavioral health organization. RR2 cut across organizations and was based on claims data but only for the Medicare subset of the sample. Both were reported in order to capture a more complete picture. In the future, obtaining data sharing agreements with all payers would be helpful in more fully examining readmission rates across all facilities in a given geographical area. Finally, we did not examine the long-term benefit of the NP beyond 30-days post discharge. Future studies would benefit from examining the impact on readmission rates over longer periods of time.
Conclusion
Limitations notwithstanding, complex patients exposed to a standard, empirically informed, group-based treatment protocol experienced enhanced gains relative to previous patients in the same facilities. These gains align with the TA mandates and were achieved within lower ALOS’s then previously obtained. These effects may be durable given the reduced readmission rates within 30 days of discharge and emphasize the importance of measurement-based care initiatives.
Declarations
Funding: No funding was received by any means in support of this research.
Conflicts of interest/Competing interests. Authors have no conflicts or competing interests to disclose.
Ethics approval. This study was approved by our internal Institutional Review Board and was conducted in accordance with the ethical standards of the 1964 Declaration of Helsinki.
Consent to participate. All participants consented to have data analyzed and reported in an aggregated form.
Consent for publication. All participants consented to have data analyzed and reported in an aggregated form.
Availability of data and material. Data is available upon request.
Code Availability. Not applicable.
Disclosures, acknowledgments, and funding information:
The authors have no conflicts of interest or financial support to disclose.
The authors would like to acknowledge Dr. Heather Jones for her work on protocol implementation and feedback on this manuscript.
References
- Substance Abuse and Mental Health Services Administration, National Mental Health Services Survey (N-MHSS). Data on Mental Health Treatment Facilities. BHSIS Series S-98, HHS Publication No. (SMA), 2016; 17-5049. 2017.
- Owens PL, Fingar KR, McDermott KW, Muhuri PK, Heslin KC. Inpatient Stays Involving Mental and Substance Use Disorders, 2016: Statistical Brief #249. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US), 2019.
- Heslin KC, Weiss AJ. Hospital Readmissions Involving Psychiatric Disorders, 2015.
- Clarke A, Glick ID. The Crisis in Psychiatric Hospital Care: Changing the Model to Continuous, Integrative Behavioral Health Care. Psychiatric services (Washington, D.C.), 2020; 71(2): 165–169.
- Glick ID, Sharfstein SS, Schwartz HI. Inpatient psychiatric care in the 21st century: the need for reform. Psychiatric services (Washington, D.C.), 2011; 62(2): 206–209.
- Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health affairs (Project Hope), 2008; 27(3); 759–769.
- Paton F, Wright K, Ayre N, Dare C, Johnson S, Lloyd-Evans B, et al. Improving outcomes for people in mental health crisis: a rapid synthesis of the evidence for available models of care. Health technology assessment (Winchester, England), 2016; 20(3): 1–162.
- Tebbett-Mock AA, Saito E, McGee M, Woloszyn P, Venuti M. Efficacy of dialectical behavior therapy versus treatment as usual for acute-care inpatient adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 2020; 59(1): 149-156. https://doi.org/10.1016/j.jaac.2019.01.020.
- Dougall N, Lambert P, Maxwell M, Dawson A, Sinnott R, McCafferty S, et al. Deaths by suicide and their relationship with general and psychiatric hospital discharge: 30-year record linkage study. The British journal of psychiatry : the journal of mental science, 2014; 204: 267–273.
- Huisman A, Kerkhof AJ, Robben PB. Suicides in users of mental health care services: treatment characteristics and hindsight reflections. Suicide & life-threatening behavior, 2011; 41(1): 41–49. https://doi.org/10.1111/j.1943-278X.2010.00015.x.
- Large M, Sharma S, Cannon E, Ryan C, Nielssen O. Risk factors for suicide within a year of discharge from psychiatric hospital: a systematic meta-analysis. The Australian and New Zealand journal of psychiatry, 2011; 45(8), 619–628.
- Nordentoft M, Erlangsen A, Madsen T. Postdischarge Suicides: Nightmare and Disgrace. JAMA psychiatry, 2016; 73(11): 1113–1114.
- Olfson M, Wall M, Wang S, Crystal S, Liu SM, Gerhard T, et al. Short-term Suicide Risk After Psychiatric Hospital Discharge. JAMA psychiatry, 2016; 73(11); 1119–1126.
- Walter F, Carr MJ, Mok P, Antonsen S, Pedersen CB, Appleby L, et al. Multiple adverse outcomes following first discharge from inpatient psychiatric care: a national cohort study. The lancet. Psychiatry, 2019; 6(7): 582–589.
- Wykes T, Csipke E, Williams P, Koeser L, Nash S, Rose D, et al. Improving patient experiences of mental health inpatient care: a randomised controlled trial. Psychological medicine, 2018; 48(3): 488–497. https://doi.org/10.1017/S003329171700188X.
- Leonard RC, Jones HM, Bailey BE, Young PR, Arzikovic AJ, Scanlon NM, et al. Adult Inpatient Treatment Workbook. Rogers Behavioral Health, 2018.
- R Core Team. R: A language and environment for statistical computing, 2018.
- Busner J, Targum SD. The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont (Pa.: Township)), 2007; 4(7): 28–37.
- Forkmann T, Scherer A, Boecker M, Pawelzik M, Jostes R, Gauggel S. The clinical global impression scale and the influence of patient or staff perspective on outcome. BMC Psychiatry, 2011; 11(83).
- Posner K, Brown GK, Stanley B, Brent DA, Yershova KV, Oquendo MA, et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. The American journal of psychiatry, 2011; 168(12): 1266–1277.
- Press Ganey Associates, 2020.
- Rush AJ, Trivedi MH, Ibrahim HM, Carmody TJ, Arnow B, Klein DN, et al. The 16-Item Quick Inventory of Depressive Symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biological psychiatry, 2003; 54(5): 573–583. https://doi.org/10.1016/s0006-3223(02)01866-8.
- Trivedi MH, Rush AJ, Ibrahim HM, Carmody TJ, Biggs MM, Suppes T, et al. The Inventory of Depressive Symptomatology, Clinician Rating (IDS-C) and Self-Report (IDS-SR), and the Quick Inventory of Depressive Symptomatology, Clinician Rating (QIDS-C) and Self-Report (QIDS-SR) in public sector patients with mood disorders: a psychometric evaluation. Psychological medicine, 2004; 34(1): 73–82.
- Chung DT, Ryan CJ, Hadzi-Pavlovic D, Singh SP, Stanton C, Large MM. Suicide Rates After Discharge from Psychiatric Facilities: A Systematic Review and Meta-analysis. JAMA psychiatry, 2017; 74(7): 694–702.
- Holley HL, Fick G, Love EJ. Suicide following an inpatient hospitalization for a suicide attempt: a Canadian follow-up study. Social psychiatry and psychiatric epidemiology, 1998; 33(11): 543–551.
- U.S. Bureau of Labor Statistics. CPI Inflation Calculator, 2020.

