Benefits of Teleconsultation of Specialty in Cardiometabolic Diseases in the Rural Area of Ecuador
Miguel Ochoa-Andrade1,2,*, Joao Recalde2, Marco Fornasini3 and Manuel E Baldeón3
1Hospital General del Sur de Quito – Instituto Ecuatoriano de Seguridad Social (IESS), Quito, Ecuador
2Facultad de Ciencias Médicas, Universidad Central del Ecuador, Quito, Ecuador
3Escuela de Medicina, Facultad de Ciencias de la Salud y de la Vida, Universidad Internacional del Ecuador, Quito, Ecuador
Received Date: 08/08/2022; Published Date: 26/08/2022
*Corresponding author: Miguel Jacob Ochoa-Andrade, Hospital General del Sur de Quito - Instituto Ecuatoriano de Seguridad Social, calle Pinllopata s/n intersección Moraspungo, Quito, 170601, Ecuador
Abstract
Introduction: Telemedicine is an important alternative for the comprehensive care of patients with cardiometabolic diseases in communities with difficult access, with limited economic resources. Quick and timely access to specialty care would improve their quality-of-life expectancy.
Methods: A prospective cohort study was carried out to evaluate the impact of a teleconsultation of specialty service in a rural parish in the province of Pichincha-Ecuador, between January 2019 and September 2020. The data for the analysis were collected from medical records, and the people who received the telemedicine service were directly interviewed about their level of satisfaction in relation to the cost, time, and insight on the service.
Results: During the study, 111 patients with cardiometabolic diseases who presented the following pathologies were treated: arterial hypertension (46.8%), type-2 diabetes mellitus (27.9%), hypothyroidism (14.4%) and prediabetes (4.5%). Only 35 patients required teleconsultation care with specialist doctors. During the follow-up of the patients, a significant reduction in blood glucose levels from 190 to 124 mg/dl, p=0.02, was observed. Glycosylated hemoglobin fell from 10% to 7%, p=0.05, systolic blood pressure fell from 128.9 ± 25.0 to 115.6 ± 13.2, and diastolic from 74.6 ± 11.5 to 60.2 ± 23.7, p=<0.01.
Conclusion: The control of patients with cardiometabolic diseases could be followed up through the implementation of teleconsultation of specialty, with evidence of improvement in their clinical and laboratory status, cost reduction, time savings, and a high level of satisfaction among users.
Keywords: Telemedicine; Specialty teleconsultation; Type-2 diabetes mellitus; Arterial hypertension; Rural population; Cardiometabolic diseases
Introduction
Telemedicine is the health service offered through the use of information technology tools that allow communication between a patient and a remote health professional in real-time. Ideally, this communication should be interactive, with the purpose of solving a specific health problem [1-3]. A good quality telemedicine program should generate a wide acceptance, level of satisfaction among users, and demonstrate its positive impact on their health and life quality [4].
One of the most innovative and relevant applications of telemedicine is the monitoring and follow-up of patients with chronic diseases to save time, and money and decrease the number of complications associated with these diseases [4,5].
In recent years, thanks to the technological development, telemedicine has become a fundamental foundation for the comprehensive management (diagnosis, treatment and follow-up) of patients in communities with difficult access, with a shortage of specialized health personnel, with limited economic resources and difficulty transferring to specialized medical care centers [4,5].
Few telemedicine programs have been implemented in Ecuador despite the fact that the geography is quite uneven, which limits the speed with which patients can be relocated. Additionally, the few programs that have been implemented have been elementary in terms of the technology used and have generally not been integrated with the public health system in order to generate greater benefits for users [4,5].
Pacto parish is located in one of the most remote rural areas of the province of Pichincha, the second most populated province in Ecuador. This location separates it from the secondary and tertiary care centers of the national health system. There is no history of the use of telemedicine in this parish, despite the fact that the health centers have access to the internet and operate regularly [6].
A recent study on arterial hypertension in the province of Pichincha (which includes the population of the present study) found that the prevalence of arterial hypertension (> 140/90 mmHg) was 27%, predominantly in men older than 50 years of age in urban communities, with low monthly income and low educational level. The study also found that of patients with high blood pressure, only 19% are adequately controlled [7]. In addition, in this same population, a prevalence of 42% of metabolic syndrome, 10% of type-2 diabetes mellitus, and 66.2% hypercholesterolemia have been reported, which demonstrates the high frequency and severity of these problems in this community [8].
Method
Study design
A prospective, descriptive cohort study was carried out on the impact of teleconsultation specialty programs in cardiometabolic diseases, in the rural parish of Pacto, Ecuador during the period between January 2019 and September 2020.
Study population
Included were all the people (n=111) that, with cardiometabolic pathologies, attended a health service center, located in the Decentralized Autonomous Government (GAD) building in the rural parish of Pacto.
In collaboration with the community leaders and mass media, patients with cardiometabolic diagnoses were summoned to the teleconsultation specialty service, which was offered during the weekends.
According to the problems and complications found in patients with cardiometabolic illness by the general MD in the initial appointment, specialty teleconsultations were carried out by experts in Internal Medicine and Endocrinology in Quito city.
Sociodemographic data
Personal pathological history, habits and occupation of the study population were retrieved from medical records (Table 1).
Anthropometrical data
For the measure of anthropological data, the body composition analyzer TANITA BC-549 IRONMAN was used for establishing weight. For size measurement size meter brand Seca 217 was used. Body mass index (BMI) was determined using the formula BMI=Weight/Height2. Low weight (<20 kg/m2), normal weight (20-25 kg/m2), overweight (25-30 kg/m2) and obesity (≥30 kg/m2) were considered [9].
Blood pressure measurement
Blood pressure levels were taken manually with the Riester Exacta 1350 adult aneroid sphygmomanometer by the general MD in charge of the telemedicine office. The technique suggested by the Pan American Health Organization (PAHO) was followed, focusing on three aspects: the patient´s condition, the team, and the observer [10,11].
Fasted measurement of capillary glucose and glycosylated hemoglobin
Capillary glucose levels were quantified with the GlobalMed TOTALVITALS GLUCOMETER GMD50700021 glucometer, as well as glycosylated hemoglobin (HbA1c) levels were quantified with the SIEMENS DCA VANTAGE analyzer.
Table 1: Prevalence of hypertension, prediabetes, type-2 diabetes mellitus, and hypothyroidism according to sociodemographic variables of the users of the telemedicine program.
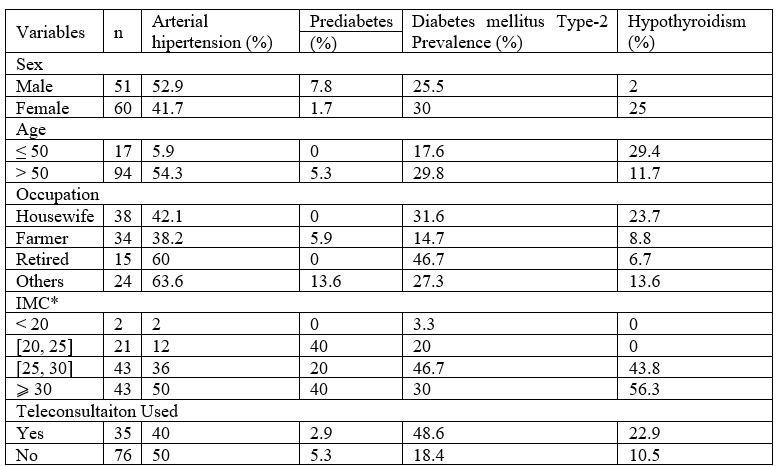
*The percentages in the columns correspond to the frequency of cardiometabolic pathologies in relation to their frequency according to the body mass index. For the rest of the variables, the cell numbers correspond to the percentages of the pathologies corresponding to each of the rows.
Out of the total population that received care in the specialty teleconsultation service, approximately 32% (n=35) required to be examined by a specialist in internal medicine or endocrinology due to the presence of clinical and biochemical alterations, (Table 1, 2). Most of these patients were over 50 years old, overweight and/or obese.
Table 2: Prevalence of hypertension, prediabetes, type-2 diabetes mellitus and hypothyroidism according to sociodemographic variables in patients who required a specialty teleconsultation.

*The percentages in the columns correspond to the frequency of cardiometabolic pathologies in relation to their frequency according to the body mass index. For the rest of the variables, the cell numbers correspond to the percentages of the pathologies corresponding to each of the rows.
The teleconsultations lasted approximately 20 minutes. The patients received remote specialty care in a similar way to what they would have received in person. Table 3 shows the changes in blood pressure, glucose level, and glycosylated hemoglobin of the people managed by specialty teleconsultation. As expected, changes in blood pressure and metabolic control were significantly improved by treatment administered by participating specialists. The average follow-up time for patients in the study was 12 months.
Table 3: Follow-up analysis of biological variables of patients managed by specialty teleconsultation.

*SBP: systolic blood pressure; **DBP: diastolic blood pressure, ***HbA1c: glycosylated hemoglobin; DE: deviation extender.
With the purpose of evaluating user satisfaction with the teleconsultation program, a survey was carried out, the results of which are summarized in Table 4, the same ones that reflect a high level of user satisfaction with the specialty teleconsultation program. When the patients were asked about the savings on time and money, they obtained by using the teleconsultation program, an important benefit of the participants was evidenced, in Table 5.
Table 4: Quality/satisfaction of the specialty teleconsultation program by patients’ evaluation.
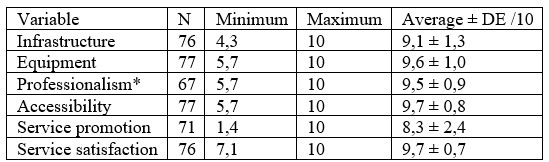
*Professionalism includes: doctor’s presentation, their interest in the patient, commitment, punctuality, communication quality.
Table 5: Cost of the specialty teleconsultation program analysis.

The users of the telemedicine service reported that they at least earned on average 24 hours of time in your care (without taking into account the time that elapses from the request for the appointment and the date of the medical consultation, which is usually between 2 to 6 months). They also indicated that they saved USD$19.1±2.9 in transportation and USD$50.2±31.6 between care and other expenses. Therefore, the total savings in direct costs was approximately USD $70, additionally, the indirect costs for losing a work day would be at least USD $13.33/day. The total sum of savings for each teleconsultation would correspond to around USD $83.33.
Discussion
Cardiovascular diseases such as type-2 diabetes mellitus and arterial hypertension could require advice from specialists, as indicated by the PAHO in its guidelines for the evaluation and management of cardiovascular risk [15].
Approximately 40% of the Ecuadorian population lives in rural areas where there are limited human resources and physical infrastructure to provide high-quality specialty health services. In Ecuador, it has been registered that income poverty at the national level in 2021 was 27.7%, with 20.8% for the urban area and 42.4% for the rural area [16].
According to the World Health Organization (WHO), pathologies such as high blood pressure and type-2 diabetes mellitus are the main causes of human health conditions and generate a high burden of premature death. These pathologies are on the rise rapidly in low- and middle-income countries. Due to its high rate of complications such as heart disease, encephalopathy, and kidney disease, among others; they represent a high human, social and economic cost for low- and middle-income countries [17-20].
Ecuador has a high and increasing problem in the frequency of chronic diseases, according to the National Institute of Statistics and Censuses (INEC) of Ecuador, mortality statistics show that this type of pathology is among the top ten causes of death [21].
The use of telemedicine has been associated with a depletion in waiting times (diagnosis/treatment), complications, and the number of referrals from primary care and hospital levels, regardless of the geographic location of the served population [4].
The use of telecommunications and portable modern telemedicine equipment gives us the possibility of improving comprehensive care and monitoring of patients with chronic diseases [4]. Some studies, including ours, have documented a significant decrease in blood pressure levels, especially in high-risk hypertensive patients [22-24].
According to reports on the clinical efficiency of the use of telemedicine for the management of patients with type-2 diabetes mellitus, there is agreement with the results obtained in our study, with a significant post-intervention reduction, compared to conventional treatments, thus demonstrating that the intervention teleconsultations are more effective than the usual ones [25,26].
Similarly, there is evidence on the benefits of managing hypertension through telemedicine with promotion of patient self-management, especially when there is supervision by a team of health professionals and a community pharmacist24; in our study, we had the participation of health personnel in the rural parish of Pacto where the controls were carried out with subsequent consultation with specialist doctors in patients with associated comorbidities and one of the advantages and similarity with the reported studies was the availability of medicine antihypertensive for immediate management in requiring cases.
Regarding patient satisfaction with the use of telemedicine, there are reports with positivity rates of 95 to 100% compared to face-to-face medical attention, indicating cut in time, travel costs, decrease in bureaucracy, better access and continuity of care [27]; The anonymous evaluation carried out in our study on satisfaction obtained a similar average, with an approximate score of 9/10, in which infrastructure, equipment, professionalism, accessibility, promotion and satisfaction of the service provided were inquired.
In other countries of the region such as Mexico, telemedicine in the current pandemic has made it possible to maintain health services in most medical specialties, limit the spread of SARS CoV-2 infection, and provide security to service providers by safeguarding their integrity [28].
Additionally, patients benefited directly from saving time to access a 24-hour specialty consultation; however, this saving in time can be considered relative, because in Ecuador, in the systems of the Comprehensive Public Health Network for taking an appointment to access a specialist can vary between 2 and 6 months, due to the high demand for the specialty service.
To estimate the savings that the patients in the study had by receiving the specialty consultation in a timely manner, it was considered that in Ecuador the unified minimum wage for the year 2020 was USD $40013, which represents a working day of USD $13.33/day. The attended people did not have to travel to the specialty centers and hence did not have to miss a work day. On the other hand, in this program, the patients received free medication for the donations and the service of the aforementioned public and private entities that participated in the study. Due to these benefits and the empathy towards the service providers, patients reported a high degree of satisfaction with this type of care. In this study, the specialty teleconsultation service was only offered for two days a week; perhaps the benefits would be even greater if the services were offered more frequently.
Conclusion
The implementation of teleconsultation in rural areas with a high prevalence of cardiometabolic diseases and with difficult access to specialized medical services can improve the clinical and laboratory control of these patients. A specialty teleconsultation service can help reduce costs, and waiting times for specialty care and generate a high level of satisfaction among users. Public and private health services should consider telemedicine a valid alternative to their patients´ treatment.
Acknowledgement
The authors are grateful for the opening of the Decentralized Autonomous Government of the Parroquia of Pacto, to carry out the specialty teleconsultation program, with the support of the infrastructure for medical care. We also thank the company PROSIRIOS and the Seguro Campesino of the Ecuadorian Institute of Social Security, who provided support with the delivery of medicine to people with a history of cardio-metabolic diseases.
Funding acknowledgements
This work was supported by the Corporación Ecuatoriana para el Desarrollo de la Investigación y la Academia - CEDIA [grant numbers USD $33.000]
Declaration of conflicting interests
The authors declare no conflict of interest.
References
- Mahajan V, Singh T, Azad C. Using Telemedicine During the COVID-19 Pandemic. Indian Pediatrics, 2020; 57(7): 652-657.
- Julien HM, Eberly LA, Adusumalli S. Telemedicine and the Forgotten America. Circulation, 2020; 142(4): 312-314.
- Llordachs F. Clinic Cloud y el desarrollo de la telemedicina. Online Referencing, 2021.
- Organización Panamericana de la Salud. Marco de Implementación de un Servicio de Telemedicina, 2016.
- Márquez Velásquez JR. Teleconsulta en la pandemia por Coronavirus: desafíos para la telemedicina pos-COVID-19. Rev. colomb. Gastroenterol, 2020; 35(1): 5-16.
- Gobierno Parroquial Pacto. Mi parroquia, 2022.
- Felix C, Baldeon ME, Zertuche F, Fornasini M, Paucar MJ, Ponce L, et al. Low levels of awareness, treatment, and control of hypertension in Andean communities of Ecuador. The Journal of Clinical Hypertension, 2020; 22(9): 1530–1537.
- Baldeón ME, Felix C, Fornasini M, Zertuche F, Largo C, Paucar MJ, et al. Prevalence of metabolic syndrome and diabetes mellitus type-2 and their association with intake of dairy and legume in Andean communities of Ecuador. PLOS ONE, 2021; 16(7): e0254812.
- Suárez-Carmona W, Sánchez-Oliver A. Índice de masa corporal: ventajas y desventajas de su uso en la obesidad. Relación con la fuerza y la actividad física. Nutr Clin Med 2018; XII(3): 128-139.
- Organización Panamericana de la Salud. HEARTS en las Américas: medición de la presión arterial, 1997.
- Gómez-León Mandujano Amir, Morales López Sara, Álvarez Díaz Carlos de Jesús. Correct technique for taking blood pressure in the outpatient. Rev. Fac. Med, 2016; 59(3): 49-55.
- Barranco Expósito C, Cívicos Juárez MA, Cáceres Rodríguez C, Díaz Vivela LF, Hernández Hernández M, Puyol Lerga MB. La calidad de servicio percibida en centros ocupacionales de personas con discapacidad: validación de la escala SERVQUAL. Trabajo social y salud, 2004; 47: 73-79.
- Amaya L. Salario básico unificado en ecuador: así quedó el sueldo para el 2022. Online Referencing, 2021.
- The World Medical Association. Declaración de Helsinki de la AMM – Principios éticos para las investigaciones médicas en seres humanos, 2022.
- World Health Organization. Prevention of Cardiovascular Disease. Guidelines for assessment and management of cardiovascular risk, 2010.
- Instituto Nacional de Estadísticas y Censos. Encuesta Nacional de Empleo, Desempleo y Subempleo (ENEMDU), 2021.
- World Health Organization. Hypertension, 2022.
- Alfonso Prínce José Claro, Salabert Tortoló Idalmi, Alfonso Salabert Iria, Morales Díaz Mariuska, García Cruz David, Acosta Bouso Anilexys. Arterial hypertension: an international health problema. Rev.Med.Electrón, 2017; 39(4): 987-994.
- Lira M. Burden of Hypertension as a Cardiovascular Risk Factor. REV. MED. CLIN. CONDES, 2015; 26(2): 156-163.
- García-Zamora Sebastián, Rosende Andrés, Casetta Brunilda, Grande-Ratti María F., Carli Natalia, Bertarini Maria F. et al. Benefits and potential risks of intensive goals in the treatment of arterial hypertension. Systematic review and meta-analysis of clinical trials. Arch. Cardiol. Méx, 2020; 90(4): 480-489.
- Instituto Nacional de Estadísticas y Censos. Boletín Técnico. Registro Estadístico de Defunciones Generales, 2020.
- Lee JY, Lee SWH. Telemedicine Cost–Effectiveness for Diabetes Management: A Systematic Review. Diabetes Technology & Therapeutics, 2018; 20(7): 492–500.
- Sood A, Watts SA, Johnson JK, Hirth S, Aron DC. Telemedicine consultation for patients with diabetes mellitus: a cluster randomised controlled trial. Journal of Telemedicine and Telecare, 2018; 24(6): 385-391.
- Omboni S, Caserini M, Coronetti C. Telemedicine and M-Health in Hypertension Management: Technologies, Applications and Clinical Evidence. High Blood Press Cardiovasc Prev, 2016; 23(3): 187-196.
- Tchero H, Kangambega P, Briatte C, Brunet-Houdard S, Retali GR, Rusch E. Clinical Effectiveness of Telemedicine in Diabetes Mellitus: A Meta-Analysis of 42 Randomized Controlled Trials. Telemed J E Health, 2019; 25(7): 569-583.
- Zhai YK, Zhu WJ, Cai YL, Sun DX, Zhao J. Clinical- and cost-effectiveness of telemedicine in type 2 diabetes mellitus: a systematic review and meta-analysis. Medicine (Baltimore), 2014; 93(28): e312.
- Nguyen M, Waller M, Pandya A, Portnoy J. A Review of Patient and Provider Satisfaction with Telemedicine. Curr Allergy Asthma Rep, 2020; 20(11): 72.
- Monraz-Pérez S, Pacheco-López A, Castorena-Maldonado A, et al. Telemedicina durante la pandemia por COVID-19. Neumol Cir Torax, 2021; 80(2): 132-140.

