Decrease of Hb and Hypo Proteinemia : Possible Predictors of Complication in Neonates with Late-Onset Sepsis in a Developing Country?
Na Cai*
Department of Pediatrics, Army Medical University, China
Received Date: 28/02/2022; Published Date: 18/03/2022
*Corresponding author: Na Cai, Department of Pediatrics, Army Medical University, Chongqing 400038, China
Abstract
Objective: The main purpose of our study was to determine the predictors for complication in neonates with LOS.
Material and methods: This were a retrospective cohort study conducted in neonatal intensive care unit between June 2016 to February 2020. Neonates with LOS were enrolled in this study. According to whether merged complication after LOS, neonates were divided into complication group and non-complication group. The demographic data, perinatal conditions, blood cell count analysis, blood culture, hypo proteinemia within 1 week after the onset and treatment measures were compared.
Results: A total of 87 neonates with LOS were enrolled in this study. Significant differences were observed between the complication and non-complication group with regard to haemoglobin (Hb), decrease of Hb, hypo proteinemia and red blood cell transfusion (P < 0.05). Further comparison found that neonates with LOS who had moderate and more severe anemia at the time of onset were more likely to have complications than those with mild or no anemia. The results of binomial stepwise logistic regression suggested that significant decrease of Hb (OR=0.045,P=0.025<0.05)and hypo proteinemia(OR=0.266,P=0.007<0.05)were independent predictors for complication in neonates with LOS. A receiver operating characteristic analysis showed that the AUC was 0.807 for decrease of Hb.
Conclusion: Significant decrease of Hb and hypo proteinemia were independent predictors for complication and may predict the occurrence of complication in neonates with LOS in the early stage.
Keywords: Sepsis; Complications; Hemoglobin; Anemia; Decrease of Hb; Hypoalbuminemia
Introduction
Neonatal Sepsis (NS) is one of the most common infectious diseases in newborns with high morbidity and mortality, and remains as the third major cause of neonatal death, especially in developing countries [1-2]. Sepsis can cause many diseases, such as septic shock, neonatal Necrotizing Enterocolitis (NEC), meningitis, osteomyelitis [3]. The occurrence of these diseases not only increases the mortality of newborns, and also cause short-term and long-term sequelae, such as intestinal stenosis, short bowel syndrome, neurological and skeletal system sequelae, etc [4-6], Seriously affect the quality of newborns’s life. Therefore, exploring the predictors of complications of NS help to take targeted prevention measures to reduce the incidence of complications and mortality. Up to now, there are many studies on the severity and prognosis of sepsis all over the world, but very few studies on the predictors for complications with NS, especially quantitative indicators. Hence, we hope that through this study, we can obtain quantitative indicators which are easy to obtain in clinical practice to predict the occurrence of complications, with a view to reducing the incidence of complications and provide new clues for optimizing the treatment strategy in the early clinical stage.
The occurrence of LOS is often accompanied by varying degrees of reduction in Hemoglobin (Hb). The decrease of Hb may cause ischemic and hypoxic damage to the body, causing redistribution of blood and microcirculation disorders, which may eventually have an adverse effect on the tissues and organs of neonates, thereby aggravating the condition. But this is limited to theoretical speculation. On the other hand, a large number of inflammatory mediators are released after LOS, which can inhibit albumin synthesis. In addition, a large amount of albumin in the body quickly synthesizes acute-phase protein, causing the albumin level to drop. Studies have shown that hypoalbuminemia was a risk factor for prognosis of sepsis in adults. Regrettably, there was no study focused on the relationship between the decrease of Hb and Hypoproteinemia and the complication in neonates with LOS. As such, our current study is unique in that it mainly focused on predicted approach of the the complication in neonates with LOS which has a potential to change the current recommendation in developing countries.
Methods
Study subjects
This was a retrospective cohort study conducted in neonatal intensive care unit (NICU). Neonates with LOS (age > 3 days) diagnosed by a neonatal specialist at at the First Hospital Affiliated to Army Medical University, China between June 2016 to February 2020. According to whether merged complications after LOS, neonates were divided into complication and non-complications group. Exclude: (1) Intrauterine infection leads to early-onset sepsis (Age ≤ 3 days), meconium aspiration syndrome; (2) Those with genetic metabolic diseases (Newborns will be screened for genetic metabolism 3 days after birth); (3) Hb reduction caused by intracranial hemorrhage, gastrointestinal hemorrhage, pulmonary hemorrhage; (4) Decrease of Hb caused by iatrogenic blood drawing.
This study was approved by the Ethics Committee of the First Hospital Affiliated of Army Medical University. All methods were performed in accordance with the relevant guidelines and regulations. The informed consent for participation in the study was obtained from legal guardians.
Clinical definitions
The diagnostic criteria for LOS refer to the Guidelines for the Diagnosis and Treatment of Neonatal Sepsis (2003) revised by the Chinese Medical Association [7]. Diagnostic criteria for sepsis: infants have fever or low body temperature, less crying, poor response and feeding and other clinical manifestations. At the same time, blood culture or sterile body cavity cultured pathogenic bacteria. Or have the above clinical manifestations and have at least the following two: ①Blood cell count analysis: the white blood cell (WBC) count < 5 × 109/L, or increased (when the age ≤ 3d, WBC > 25 × 109/L; the age > 3d, WBC > 20 × 109/L); ②Cell classification: immature neutrophils / total neutrophils (I/T) ≥ 0.16; ③Platelet count (PLT) < 100 × 109/L; ④C-reactive protein (CRP) ≥ 8 mg/L. Complications caused by LOS include septic shock, NEC, meningitis, osteomyelitis, Diffuse intravascular coagulation (DIC). For the diagnosis of complications, refer to the fourth edition of Practical Neonatology [3]. Hemoglobin (Hb) in the neonatal period < 145 g/L is anemia, 144 - 120 g/L is mild, - 90 g/L is moderate, - 60g/L is severe, and < 60 g/L is extremely severe [8]. Diagnostic criteria for hypoproteinemia: serum albumin (Alb) < 25g/L [9].
Data collection
Demographic data were obtained from the electronic medical records and included mother's prenatal condition, such as whether there was premature rupture of membranes, amniotic fluid meconium pollution, maternal hypertension and diabetes, etc. At the same time, the information of neonates, such as gender, gestational age, birth weight, age of onset, comorbidities, blood cell count analysis, blood culture, albumin within 1 week after the onset and treatment measures (after the occurrence of LOS and before the occurrence of complications) was also recorded. When patients first showed the symptoms of LOS (such as fever, poor response and feeding), the blood samples collected for the first time would be examined. Laboratory parameters such as WBC, PLT, Hb, the decrease of Hb, blood culture and albumin were measured.
In addition, we collected the most recent Hb before LOS and interval between two Hb collections ( the most recent Hb before LOS and Hb at the early stage of LOS). There were no differences in the most recent Hb before LOS and sample collection interval between the two groups. At the same time, we calculated the amount of venous blood collection in the early stage of LOS in the two groups to avoid the decrease of Hb caused by iatrogenic blood collection. There was no significant difference in venous blood collection between the two groups. Calculate the decrease of Hb: the most recent Hb before LOS - Hb at the early stage of LOS.
Statistical analysis
SPSS 20.0 was used for statistical analysis. The continuous variables of non-normal distribution were rendered as median interquartile range (IQR) percentiles and were compared using Mann-Whitney U-tests. Categorical variables were presented as absolute number and percentage. Differences in categorical variables were assessed for significance using Chi-square test and Fisher’s Exact test. Multivariate logistic regression analysis was used to assess the independent predictors for complication in neonates with LOS. The receiver operating characteristic (ROC) method was conducted to evaluate the utility of different variables in predicting complications in neonates with LOS. The sensitivity and specifcity were compared by analyzing the area under the ROC curve. P < 0.05 was considered significant.
Results
Comparison of general data between the two groups
Total 87 neonates with LOS were included, 56 in the non-complication group and 31 in the complication group, including 14 cases of NEC, 6 of septic shock, 8 of meningitis, 2 of osteomyelitis, and 1 of DIC. Demographic characteristics of the two groups were presented in Table 1, including their gender, gestational age, birth weight, age of onset, perinatal situation, comorbidities, etc. The results showed that there were no signifcant differences were observed regarding these data among the complication group and non-complication group(P > 0.05).
Table 1: The baseline clinical characteristics of the complication and non-complication group.

PROM > 18 h indicates Premature rupture of membranes > 18 hours, NRDS indicates neonatal respiratory distress syndrome. The continuous variables of non-normal distribution were rendered as median interquartile range (IQR) percentiles and were compared using Mann-Whitney U-tests. Categorical variables were presented as absolute number and percentage, and were compared using Chi-square test and Fisher’s Exact test. P < 0.05 was considered significant.
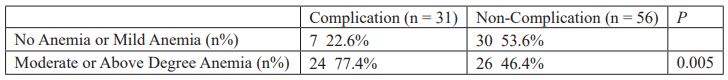
Significant differences in Hb, decrease of Hb, hypo proteinemia and red blood cell transfusion
Significant differences were observed between the complication and non-complication group with regard to Hb, decrease of Hb, hypo proteinemia within 1 week after the onset and red blood cell transfusion (P < 0.05). No significant difference in WBC, PLT, blood culture and mechanical ventilation was observed between the two groups (P > 0.05, Table 2). Further analysis of the impact of different degrees of anemia on the incidence of complication suggested that neonates with moderate or more severe anemia were more likely to have complications than those with mild or no anemia (P < 0.05, Table 3).
Table 2: Comparison of laboratory indicators and treatment measures between the two groups.

WBC indicates white blood cell, PLT indicates Platelets and Hb indicates hemoglobin. The continuous variables of non-normal distribution were rendered as median interquartile range (IQR) percentiles and were compared using Mann-Whitney U-tests. Categorical variables were presented as absolute number and percentage, and were compared using Chi-square test and Fisher’s Exact test. P < 0.05 was considered significant.
Table 3: Comparison of the severity of anemia between the two groups.
Significant decrease of Hb and hypoproteinemia were independent predictors for complication in neonates with LOS
Binomial stepwise logistic regression was used with whether complication occurred as the dependent variable, and the above statistically significant indicators, including Hb, decrease of Hb, hypo proteinemia and red blood cell transfusion were used as independent variables to test whether each factor had a significant effect on complication. The results suggested that significant decrease of Hb(OR=0.045,P=0.025<0.05)and hypo proteinemia(OR=0.266,P=0.007<0.05)were independent predictors for complication in neonates with LOS. (Table 4).
Table 4: Logistic regression analysis results.
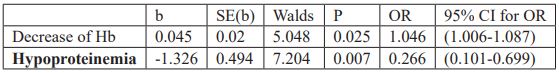
Hb indicates Hemoglobin.
The high predictive value of decrease of Hb for complication in neonates with LOS
The Receiver Operating Characteristic (ROC) analysis of LOS showed that Area Under the Curve (AUC) was 0.807, suggesting that decrease of Hb may predict the occurrence of complication in neonates with LOS (Table 5, Figure 1).
Table 5: The ROC curve of the decrease of Hb for predicting complication in sepsis.


Figure 1: The ROC curve of decrease of Hb for predicting complication in neonates with LOS.
Discussion
The neonatal immune system is immature, highly susceptible to many microorganisms and prone to sepsis, especially premature infants and low birth weight infants. Long-term use of invasive procedures and intravenous nutrition increase the incidence of sepsis. Due to the low immunity and weak resistance of the newborn, sepsis often develops rapidly from subclinical symptoms to severe systemic infection symptoms, causing damage to systemic organs and the occurrence of diseases, such as NEC, meningitis, septic shock, DIC, etc, making sepsis become an important cause of neonatal death [10]. Therefore, it is great significance to analyze the specific risk factors of complications and death of sepsis, taking active control measures to reduce the incidence of complications and mortality. Our study found that there was significant difference in Hb, decrease of Hb, hypoproteinemia within 1 week after the onset and red blood cell transfusion between the complication group and non-complication group. Further logistic regression showed that significant decrease of Hb and hypoproteinemia were independent predictors for complication in neonates with LOS.
The effect of anemia and decrease of Hb on the complications and prognosis of neonates with LOS
Sepsis is often accompanied by anemia or a decrease in hemoglobin concentration. Many causes can lead anemia, such as iatrogenic blood loss, reduced serum iron levels, shortened red blood cell life and increased destruction, etc. In addition, vascular endothelial glycocalyx shedding and intravenous fluid administration lead to blood thinning [11-13], which is also manifested by a decrease in Hb, causing thinning ‘anemia’. But in the early stage of sepsis, the decrease of Hb is mostly caused by increased destruction of red blood cells and damage to the glycocalyx layer. In severe infection, a large number of inflammatory factors are released, on the one hand, directly destroying red blood cells, causing a decrease in Hb. On the other hand, a large number of inflammatory factors destroy the glycocalyx layer of the vascular endothelium, causing dilution anemia. Therefore, we speculate that the decrease of Hb may reflect the level of inflammation in the body, the more obvious the decrease in Hb, the more severe the inflammation. After the occurrence of sepsis, the body may have microcirculation disturbances, leading to tissue ischemia and hypoxia. When severe infection occurs, a large number of inflammatory factors are secreted in the body, which leads to true anemia or dilute ‘anemia’ through various mechanisms. The significantly reduced Hb further causes ischemia and hypoxia, and redistribution of blood in the body, causing or aggravating the microcirculation disorder. Eventually, sepsis and significantly reduced Hb complement each other and cause adverse effects on tissue organs. Studies have shown that anemia is a high-risk factor of NEC [14-18], and the incidence of NEC in children with moderate or above anemia is higher than that without anemia or mild anemia [19]. Jung SM [20] found that low hemoglobin levels (< 9.0 g/dL) were observed in approximately 20% of patients with septic shock, and the severity of decrease in these levels correlated with mortality, the lower the Hb, the higher the mortality rate. Loftus TJ [21] found that reducing anemia may improve the prognosis of sepsis patients. This study found that the incidence of complications in children with sepsis was closely related to the severity of anemia and the degree of Hb reduction at the onset. Moderate or above anemia and significantly reduced Hb are more likely to have complications. At the same time, this study found that after the occurrence of sepsis and before the occurrence of complications, the transfusion of red blood cells may increase the incidence of complications. Many studies have also shown that the transfusion of red blood cells can lead to the occurrence of NEC [22-23], and increase the chance of surgery in children with NEC and reduce the survival rate [24]. A foreign study on blood transfusion after sepsis in children showed that after sepsis-related anemia, compared to the restrictive strategy group, there had a significantly higher incidence of acute respiratory distress syndrome and acute lung injury in the liberal transfusion group. Moreover, mortality was significantly higher, and liberal transfusion might be associated with a worse outcome [25]. In addition, other studies found that the transfusion of red blood cells may increase the mortality of critically ill patients [26-27]. It should be pointed out that the anemia associated with sepsis is not all true anemia, and sometimes it may be caused by blood dilution related to fluid load [28-29]. Therefore, after the occurrence of sepsis, even if the Hb is reduced, it is necessary to strictly grasp the blood transfusion pointer and carefully infuse red blood cells.
Further logistic regression showed that decrease of Hb was an independent predictor for complication in neonates with LOS. By comparing the ROC curves of the decrease of Hb,the results showed that the AUC was 0.807 for the decrease of Hb, which suggests that decrease of Hb (cut-off value: 14.5) may predicted the occurrence of complication in neonates with LOS.
The effect of hypoproteinemia on the complications and prognosis of neonates with LOS
This study found that the incidence of hypoproteinemia in the complication group was significantly higher than that in the non-complication group. Logistic regression showed that hypoproteinemia was an independent predictor for complication in neonates with LOS. Hypoproteinemia is a common complication of sepsis and albumin can be reduced by about 10–15 g/L within 1 week after sepsis. After infection, a large number of inflammatory mediators such as interleukin - 1 (IL - 1), IL - 6 and tumor necrosis factor - α are released, which can inhibit albumin synthesis. In addition, when children have sepsis, the body will have fever, stress and inflammation. These symptoms will accelerate metabolism, a large amount of albumin in the body quickly synthesizes acute-phase protein, causing the albumin level to drop [30]. At the same time, increased permeability and destruction of vascular endothelial integrity can also lead to hypoalbuminemia [9]. Hypoproteinemia can cause the plasma colloid osmotic pressure to drop and a large amount of fluid remains in the tissue gap, which reduces the effective blood volume of the body and causes damage to multiple organ functions. In addition, albumin can clear free radicals in the body and inhibit the production of oxygen free radicals by multinuclear cells. But when sepsis occurs, a large number of inflammatory factors are secreted, leading to proinflammatory and anti-inflammatory imbalances in the body, the activity of free radicals is out of control, and a large number of free radicals are produced. The occurrence of hypoalbuminemia leads to a weakening of the body's ability to scavenge free radicals and promote the development of sepsis. Therefore, it is necessary to pay attention to children with hypoalbuminemia after the occurrence of infection. For those with sepsis complicated with hypoalbuminemia, the hypoalbuminemia should be actively corrected to reduce the incidence of complications.
Conclusion
A careful analysis of the decrease of Hb and hypo proteinemia within 1 week after LOS, which is easily accessible and affordable, represents a valuable tool to predict the occurrence of complication in neonates with LOS in the early stage.
Conflict of interest
The authors declare that there is no conflict of interest.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant/Award Number: 82170565).
Ethical approval
This study was approved by the Ethics Committee of the First Hospital Affiliated of Army Medical University. All methods were performed in accordance with the relevant guidelines and regulations. The informed consent for participation in the study was obtained from legal guardians.
References:
- Logan A, Freemam J, Kent B, Pooler J, Creanor S, Vickery, J, et al. Standing practice in rehabilitation early after stroke (SPIRES): a functional standing frame programme (prolonged standing and repeated sit to stand) to improve function and quality of life and reduce neuromuscular impairment in people with severe sub-acute stroke - a protocol for a feasibility randomised controlled trial. Pilot and feasibility studies. 2018; 4: 66.
- Mehrholz J, Wagner K, Meissner D, Grundmann K, Zange C, Koch R, et al. Reliability of the Modified Tardieu Scale and the Modified Ashworth Scale in adult patients with severe brain injury: a comparison study. Clinical rehabilitation. 2005; 19: 751-759.
- Banky M, Williams G. Tardieu scale. Journal of physics. 2017; 63: 126.
- Gajdosik R, Bohannon R. Clinical Measurement of Range of Motion Review of Goniometry Emphasizing Reliability and Validity. Physical therapy., 1988, 67, 1867-1872.
- Van Rijn SF, Zwerus EL, Koenraadt KL, Jacobs WC, Van den Bekerom MP, Eygendaal D. The reliability and validity of goniometric elbow measurements in adults: A systematic review of the literature. Shoulder & elbow. 2018; 10: 274-284.

