In-Hospital Cardiac Arrest; a Descriptive Analysis into Cardiopulmonary Resuscitation
Zubaria Altaf, Pocholo Isidro, Almunzer Zakaria, Sara Kazkaz,
Senior Quality Improvement Reviewer, Al Wakra Hospital, Hamad Medical Corporation, Qatar
Quality Improvement Reviewer, Al Wakra Hospital, Hamad Medical Corporation, Qatar
Assistant Executive Director Quality Improvement and Patient Safety, Al Wakra Hospital, Hamad Medical Corporation, Qatar
Research Specialist, Al Wakra Hospital, Hamad Medical corporation, Qatar
Received Date: 28/02/2022; Published Date: 14/03/2022
*Corresponding author: Sara Kazkaz, Research Specialist, Al Wakra Hospital, Hamad Medical corporation, Qatar.
Abstract
This study is a retrospective descriptive review of all Cardiopulmonary Resuscitation (CPR) attempts at Al Wakra Hospital (AWH) conducted during one year i.e., 1st Jan 2020 to 31st Dec 2020. AWH is a 329 bedded Multispecialty Secondary care facility, part of Hamad Medical Corporation (HMC), the largest Governmental Healthcare organization in Qatar. In 2020, AWH had 11,862 inpatient admissions which are inclusive of Adult, Pediatric, Neonatal, Geriatric populations. There were also 1,184 admissions to the different Intensive Care Units (Medical, Surgical, Pediatric, and Neonatal). AWH has a Rapid Response Team (RRT) and Code Blue (CPR) team which is responsible for the respective codes. Code Blue team comprises one ICU Physician, one Respiratory Therapist, one Registered Nurse, all trained in Advanced Life Support. All CPR attempts were documented and recorded in CPR Record Sheets which were reviewed and the Electronic Medical Records (Cerner) were sourced for data gathering. One copy of CPR record sheets was kept in Cerner (Patient File) and one was sent to the Quality department for review/audit. After obtaining the list of CPR attempts over the year 2020, patients were identified, and medical records reviewed. The parameters recorded were demographic information, location, comorbidities and other relevant history, duration of CPR, initial CPR outcome, patient disposition, patient status on disposition (quality of life), etc. All these variables were considered to support the objective of this study i.e., to perform a descriptive analysis of in-hospital CPR. Based on the analysis of 110 patients for whom CPR was done, the percentage of immediate survival on the initial CPR was 53.64%. However, only 8.18% were eventually discharged to home while 11.82% were discharged to other HMC facilities.
Keywords: CPR; In-hospital Cardiopulmonary Resuscitation; Resuscitation; Code Blue; Cardiac Arrest; Survival post CPR
Introduction
A cardiopulmonary arrest is a disastrous event with a high rate of mortality [1]. Cardiopulmonary arrest is the absence of functional ventilation and circulation in a person [2]. With the evolution of time, Cardiopulmonary Resuscitation (CPR) became an integral part of medical care in all patients facing imminent death2. Survival of different age groups undergoing CPR from published literature as concluded by Saklayen, Liss, and Markert is 15.2 % upon discharge from the hospital [3]. The CPR success rate is related to the circumstances of cardiopulmonary arrest (in-hospital vs out-of-hospital, witnessed vs unwitnessed, etc). While innovations such as the defibrillators used by emergency medical service personnel, which allow for prompt CPR, resulted in improved out-of-hospital CPR outcomes [4].
This study is a retrospective descriptive review of all Cardiopulmonary Resuscitation (CPR) attempts at Al Wakra Hospital (AWH) conducted for 1 year i.e., 1st Jan 2020 to 31st Dec 2020. All CPR in-hospital attempts are recorded in the CPR Record Sheets, a copy of which is kept as an uploaded file in the patient’s medical records (Cerner), and 1 copy is sent to the Quality department for review/audit. CPR Sheets can provide information on the Patient’s Demographics, time date location of the Cardiac arrest, circumstances throughout the code event, method of ventilation, defibrillations, medications administered, and immediate outcome of the CPR. This documented information will be utilized to study the survival rate/outcome in these patients regardless of the gender and comorbidity status upon arrest, also describing the other variables that were involved in the patient’s prearrest state of health. Similar research has not been done in Qatar before therefore, this study will serve as a reference for other healthcare facilities in Qatar to compare their survival rates and also to study the factors involved in the outcome of these patients.
The objective of this study was to describe the rate of immediate survival and rate of survival upon discharge in patients undergoing in-hospital cardiopulmonary resuscitation at AWH for 1 year i.e., 2020. In addition, the study highlights the co-variables and demographic factors identified amongst this patient population.
Methods and Tools
Retrospective review of data and CPR Record Sheets from 1st Jan 2020- 31st Dec 2020. Data will be collected from Cerner (Patient Files) & CPR Records sheets for all patients undergoing active Cardiopulmonary resuscitation at AWH in the year 2020. Descriptive analysis will be carried out to briefly explain the demographic & clinical factors involved in the outcome i.e., Survival of the patient undergoing cardiopulmonary resuscitation within the vicinity of Al Wakra Hospital.
Discussion
There was a total of 110 unique patients for whom CPR was done in the year 2020. A significant portion (73.64%) had multiple CPR attempts throughout their hospital stay. For a patient to be considered as having multiple CPR attempts, the patient should have had at least one code blue activation following an initial CPR with the successful Return of Spontaneous Circulation (ROSC) regardless of the time interval between the two events. However, for this study, the initial survival is determined by a successful ROSC that is maintained within the same location by the same CPR team. Any patient who was initially resuscitated but had another code blue episode and expired while being attended by the same team in the same hospital location will still be considered as an unsuccessful initial survival. Any patient that was successfully transferred to a higher level of care (e.g., Emergency Department to Intensive Care Unit) following ROSC will automatically be considered as having a successful initial survival.
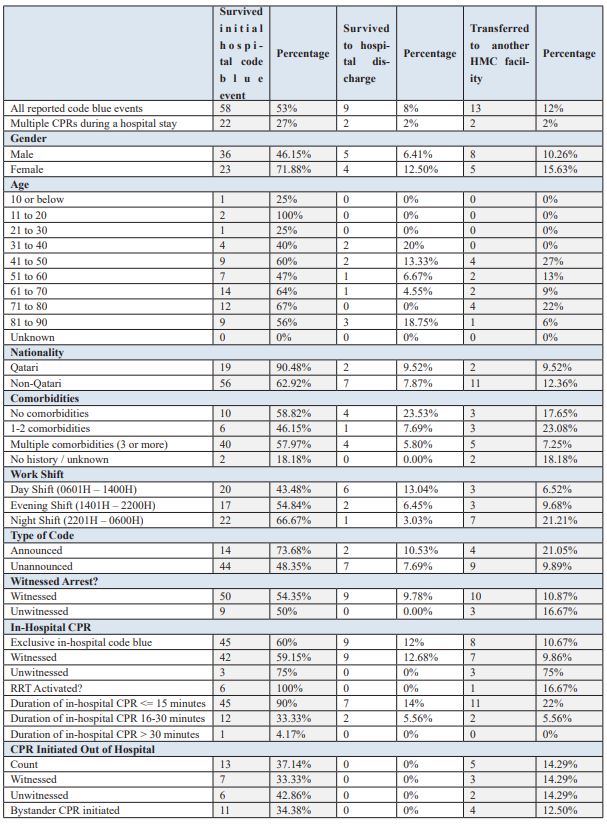
Table 1: Al Wakra Hospital CPR Data, 2020.

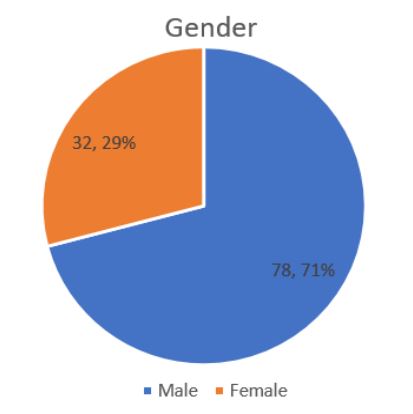
Figure 1: Gender of code blue patients.

Figure 2: Age range of code blue patients.
Of all CPR events in 2020, 70.91% were male patients while only 29% were female. The youngest patient identified was three weeks old while the oldest was 89 years old, and the median age is 63 years. The distribution curve is skewed to the left with the most incidences of code blue falling in between 61 to 70 years followed closely by the 71 to 80 age range. Four patients were brought to Emergency Department without any identification and were classified as unknown patients thus their ages could not be retrieved.
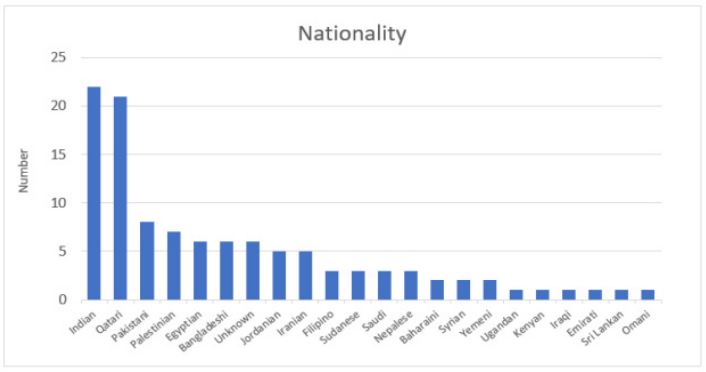
Figure 3: Nationality.
There is a diverse composition of nationalities making up the list of code blue events, the majority of which are expatriates from India with 22 cases or 20% of all events. Furthermore, 80.91% of all recorded events were non-nationals. Qataris make up the rest of 19.09% with 21 cases, the second-highest in terms of nationality.
The most common comorbidities observed were hypertension and diabetes which were present in 56.36% and 54.55% of all the patients respectively. 15.45% had no reported comorbidities, 11.82% had at least one to two, and 62.73% had more than three. Healthcare providers were unable to extract the past medical history from 11 patients (10%).

Figure 4: Code blue locations within AWH.
The majority of the incidents came from the Adult Emergency Department (45 cases) which can be further stratified into the following: 1. Out-of-hospital arrests brought to the Adult Emergency Department by the Emergency Medical Services (EMS or ambulance service) with ongoing resuscitation (30 cases); 2. Arrests that occurred within the unit (13 cases); and arrests brought in by private transportation (2 cases). The Critical Care units composed of the Medical Intensive Care Unit (MICU), Surgical Intensive Care Unit (SICU), and the High-Dependency Unit (HDU), which is a step-down critical care unit, had a combined 42 code blue events for the year.
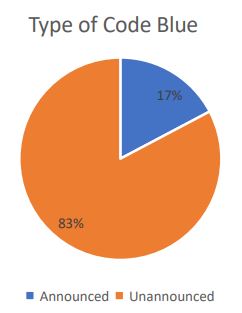
Figure 5: Code blue type.
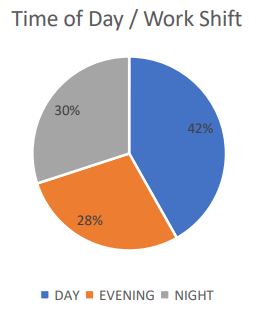
Figure 6: Time of Day / Work Shift.
Code blue activations within these units, including Operating Theaters and other Emergency Departments, are categorized as “unannounced” or “silent” code because these are not being announced through the facility’s overhead paging system and that the units have their code blue responders available 24/7 within the department. This is in direct contrast with a code blue activated in the inpatient wards wherein external help is required via the facility’s designated code blue team, which are staff usually assigned inside the critical care units. Out of the 110 code blue activations, only 17% were announced with all 19 cases having a code blue team response time of 5 minutes or less.
CPR events can happen at any time of the day with 42% of the cases occurring between 6 am to 2 pm, considered as the “day shift”. 30% of the events occurred during the “night shift”, from 10 pm until 6 am. The evening shift, from 2 pm until 10 pm, had the lowest number of code blue events at 28%.
Witnessed arrests account for 83.64% of all events with 92 cases while there were only 18 unwitnessed arrests. 68.18% of the arrests (75 cases) happened within the facility (in-hospital) while 27.27% (30 cases) occurred outside and were brought in arrested by ambulance (EMS). One case was an out-of-hospital arrest but was revived by EMS during transit. The patient came to AED with a pulse but had another episode within the hospital. 4 cases were brought in arrested by a private vehicle.
The mean duration of all in-hospital code blue events, from the time of activation to the time of announcement of termination is 21 minutes with a median of 16 minutes. This excludes any CPR conducted by the EMS outside of the facility. For the code blue events that happened exclusively within the hospital, the mean duration is at 18 minutes.
Figure 7: Initial survival.

Figure 8: Hospital disposition.
Code blue initial survival and hospital disposition were also examined. Half of the patients in which code blue was activated were successfully revived with the initial CPR survival at 52.73% (58 patients); however, only 9 patients (8.18%) were eventually discharged to home while 2 cases (1.81%) were transferred to a long-term healthcare facility. There were 11 patients (10%) who were transferred to other HMC facilities for the continuation of care after being stabilized in AWH. The hospital length of stay of the 9 patients who eventually got discharged to home ranged from 8 days up to 3 months with a median value of 15 days.
58.82% of patients without any comorbidities survived the initial code blue event, 41.18% of which either survived hospital discharge or were transferred to other HMC facilities. Initial survival for patients having 1 to 2 comorbidities was 46.15% but only one patient got to be discharged while 3 were transferred. For patients with three or more comorbidities, initial survival was 57.97%, discharged to home was 5.8% and 7.25% were transferred.
Initial survival in witnessed arrests is 54.35% and 50% in unwitnessed arrests. However, the percentage who got discharged was 9.78% for the witnessed and 0% for the unwitnessed events.
Table 2: Code Blue Survival Data, 2020.
Conclusion
This review does not aim to provide any correlation between the survival rates and the multiple variables or factors presented in this study. However, the rich information that can be derived from the data could still prove useful to other healthcare organizations in referencing rates from a secondary care multi-specialty hospital like Al Wakra Hospital in Qatar. Continuation of data collection and further studies with longer time frames may be done in the future to develop a more robust and more in-depth analysis of the state of cardiopulmonary resuscitation efforts not just within the facility but in other healthcare facilities within the country as well.
Conflict of Interest: None
References:
- Fowler R, Chang MP, Idris AH. Evolution and Revolution in Cardiopulmonary Resuscitation. Current Opinion in Critical Care, 2017; 23(3): 183–187.
- Goldberg A. Cardiopulmonary Arrest. The New England Journal of Medicine, 1974.
- Saklayen M, Liss H, Markert R. In-hospital cardiopulmonary resuscitation. Survival in 1 hospital and literature review. Medicine, 1995; 74(4): 163–175.
- Schluep M, Gravesteijn BY, Stolker RJ, Endeman H, Hoeks SE. One-Year Survival After In-Hospital Cardiac Arrest: A Systematic Review and Meta-Analysis. Resuscitation, 2018; 132: 90–100.

