Catheter-Associated Urinary Tract Infection, About 321 Cases
Adil Kbirou*, Mahmoud Alafifi, Saleh Abdelkerim Nedjim, El Mostapha Abdi, Amine Moataz, Mohammed Dakir, Adil Debbagh, Rachid Aboutaieb
Urology Department, University Hospital Center IBN ROCHD, Casablanca
Received Date: 23/12/2021; Published Date: 07/01/2022
*Corresponding author: Adil Kbirou, Urology Department, University Hospital Center IBN ROCHD, Casablanca, Morocco.
Summary
Introduction: Urinary catheterization is a common clinical practice that comes with a number of risks and complications. These complications include the frequently reported infection, which may be the result of poor care hygiene.
The purpose: of this study is to investigate the link between the catheter and urinary tract infection by describing the various risk factors, indications, ecology, and bacterial resistance profile.
Materials and Methods: This is a retrospective study of 321 patients who presented with a catheter-associated urinary tract infection during their follow-up at the urology department of the university hospital center IBN ROCHD from January 1 to December 31, 2019.
Results: Patients range in age from 17 to 92 years old. Males outnumbered females in the sex ratio H/F 1.55. The most common reason was bladder tumor in 37% of the cases, followed by prostate adenoma in 32% of the cases. Cytobacteriological examination of urine (CBEU) discovered Gram Negative bacteria as the main germs (89 %), with Escherichia coli predominating in 64 % of cases.
Conclusion: This study suggests that strict urinary catheterization procedures are needed to ensure compliance with good practices and, as a result, reduce the risk of urinary tract infection.
Introduction
Urinary catheterization is now the most common invasive gesture in urology, often misunderstood but implicated in the appearance of urinary tract infection [1]. Catheter associated urinary tract infections are accounting for 70-80 percent of all infections [2]. It is a major public health issue due to its association with a significant morbidity-mortality rate, the emergence of multidrug-resistant bacteria posing therapeutic challenges, and the significant economic and financial impact associated with its use.
The goal of our study was to investigate the relationship between Urinary catheterization and Catheter associated urinary tract infections by describing epidemiological, clinical, and bacteriological characteristics in the urology department of the IBN ROCHD university hospital center.
Materials and Method
This is a retrospective, descriptive study that took place in the urology department of IBN ROCHD university hospital center from January 1 to December 31, 2019 and included 321 patients with Catheter associated urinary tract infections. We gathered the following information from medical records: age, gender, indication, location, and duration of the urinary catheterization, and results of the cytobacteriological examination of the urine (isolated germ and antibiogram).
Results
Our department treated 321 patients with Catheter associated urinary tract infections identified in our study. The average age of the patients was 61 years, with extremes ranging from 17 to 92 years, and the most affected age group (57 percent) ranged from 60 to 79 years (Figure 1).

Figure 1: Distribution of patients by age group.
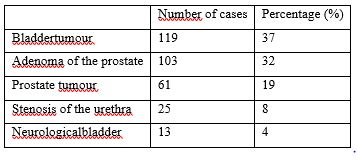
The sex ratio H/F was 1.55, indicating a male predominance. In terms of etiologies, bladder tumors were found in 37% of cases, followed by prostate adenoma in 32% of cases, prostate cancer in 19% of cases, urethral stenosis in 8% of cases, and neurological bladder in 4% of cases (Table 1).
Table 1: Distribution of patients based on the etiology of the obstruction.
In terms of urinary catheterisation aspects, the emergency department was the most common location for catheterisation, with 205 patients (67 percent) catheterised there, 67 patients (21 percent) in the operation room, and 39 patients (12 percent) in other departments. The majority of patients (78%) had urinary catheterisation for more than two weeks, whereas 22 percent had it for less than two weeks (figure 2).
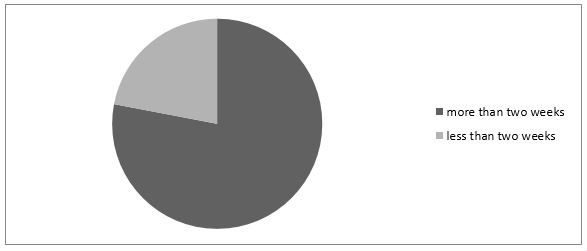
Figure 2: Patient distribution based on the length of the bladder urinary catheter.
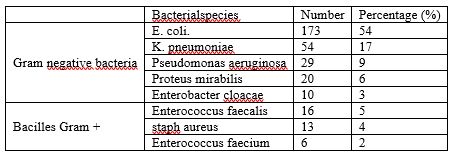
Bacteriologically, cytobacteriological examination of urine (CBEU) found Gram bacteria as the main germs – in 89 percent of isolated strains with predominance of Escherichia coli (54.10%), followed by Klebsiella pneumoniae (17%) and Pseudomonas aeruginosa (9%). Gram+ bacilli were isolated in 11% of cases, with Enterococcus faecalis (5%) predominating.
Table 2: Distribution of Isolated Bacterial Species in CBEU.
Along with natural resistances, the study of enterobacteriaceae sensitivity revealed a low sensitivity to Ampicillin (23%), Amoxicillin + Clavulanic acid (31%), a moderate sensitivity to Quinolones (68%), Nitrofurans (62%), and Trimethoprim (61%), and a high sensitivity to aminosides (78%) (amikacin and gentamicin), imipenem (96%), and Colistine (98%). (Figure 3).

Discussion
Healthcare-associated urinary tract infections are common in the elderly and are frequently associated with the use of an endo-urinary device. Urinary tract infections caused by urethral catheterization are frequent, accounting for around 30% of nosocomial infections [1]. It is critical to differentiate between a symptomatic UTI and colonization caused by prolonged urethral catheterization [3]. Bacterial colonisation during indwelling catheter has been demonstrated to be unavoidable. The probability of equipment colonisation (positive CBEU without clinical symptoms) is around 3-8 percent day [2]. According to the 2012 French national prevalence study of Nosocomial Infections (NI), healthcare-associated urinary tract infections accounted for nearly one-third of all healthcare-associated infections (HAIs). They were found in 1.6 percent of the population. The occurrence of a urinary catheterisation was the main risk factor [4].
A descriptive cross-sectional study performed at the Casablanca University Hospital in Morocco revealed that the prevalence of HCAI was 10.3 percent, with urinary tract infections being the most common (28.9 percent), followed by bacteremia (22.7 percent). The presence of an invasive device was shown to be strongly linked with the occurrence of HCAI [5]. Our analyses demonstrate the high prevalence of urinary tract infections on urinary catheters and highlight the importance of preventing this type of infection to reduce morbidity and mortality. Clinically, the typical local symptoms of urinary tract infections are absent, due to the decompression and persistent drainage of urine [3]. Urgency is not a symptom of infection in the presence of an endoureteral catheter. A prospective study of 1497 catheterized patients found that more than 90% of those with bacteriuria or candiduria more than 103 CFU/ml were asymptomatic [6]. In roughly a quarter of patients, local signs such as painful micturition, pollakiuria, or suprapubic tenderness may develop following catheter removal [7,8]. A change in the odour or appearance of the urine is not always indicative of UTI. However, the recent onset of hyperthermia (> 38°C), chills, hypothermia (36°C), or hypotension that cannot be explained by another evident cause requires a CBEU to search for bacteriuria. Low- Back pain, cognitive alterations or deteriorating functional dependency, general malaise or tiredness with no other known cause should all be considered signs of a urinary tract infection [8,9]. In these cases, if there is considerable bacteriuria and no spontaneous remission of symptoms, specialized therapy is necessary.
The vast majority of Healthcare-associated urinary tract infections are monomicrobial. Gram-negative bacilli (GNB) represent at least 2/3 of the microorganisms isolated. E. coli is in the majority with frequencies varying according to the studies from 26 to 46.2% [3], whereas our study found BGN as the main germs in 89% of the isolated strains with a predominance of Escherichia coli (54.10%). Regarding the results of antibiotic sensitivity testing, we highlight the increase in antibiotic resistance to the isolated germs, especially enterobacteria, which correlates with some studies [6-7] where multidrug resistant germs were isolated. The high incidence could be due to various reasons such as patient gender, infection control policies, catheter care, duration of bladder catheterisation and the etiology of catheterisation. Reducing the duration of catheterisation and limiting its indications has been shown to decrease the prevalence of catheter-related UTIs [11,12]. Prevention is the key element in the management of catheter-associated UTIs by avoiding excessive catheterisation and restricting it to relevant inpatient or perioperative indications, preferring alternatives to catheterisation (e.g. ultrasound measurement of bladder residuals, intermittent evacuation catheterisation, etc.), and avoiding the use of other methods, Prefer alternatives to catheterisation (ultrasound measurement of bladder residue, intermittent evacuation catheterisation, penile sheath, suprapubic catheter) and ensure early removal of the catheter by using mnemonics [13], insert the catheter under strict aseptic conditions and use a closed drainage system throughout the duration of the catheterisation (no disconnection).
Conclusion
Our study reveals a high frequency of Catheter-associated urinary tract infection and emphasises the importance of following preventive measures, especially impressive hand hygiene, strict adherence to Urinary catheterization indications and aseptic measurements during the catheterization, and training of staff, to limit the emergence of multidrug-resistant strains.
References
- Vallée M, Robert G, Rigaud J, Luyckx F. Technique et gestion du sondage vésical chez l’homme. Progrès En Urologie, 2018.
- Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associatedurinary tract infection in adults: 2009 International clinical practice guidelines from the infectiousdiseases Society of America. Clin Infect Dis, 2010; 50(5): 625-663.
- Révision des recommandations de bonne pratique pour la prise en charge et la prévention des infections urinaires associées aux soins (IUAS) de l’adulte, 2015.
- Enquête nationale de prévalence des infections nosocomiales et des traitements antiinfectieux en établissements de santé, France, mai-juin 2012.
- Hassoune S, Ouhadous M, Bouri HE, Nani S, Barrou H. Prévalence des infections associées aux soins au centre hospitalier universitaire de Casablanca, Maroc, 2014. Revue d’Épidémiologie et de Santé Publique, 2016; 64.
- Tambyah PA, Maki DG. The relationshipbetweenpyuria and infection in patients withindwellingurinarycatheters:a prospective study of 761 patients. Arch Intern Med, 2000; 160: 673-677.
- Harding GK, Nicolle LE, Ronald AR, Preiksaitis JK, Forward KR, Low DE, et al. How long shouldcatheter-acquiredurinary tract infection in womenbetreated ? A randomizedcontrolledstudy. Ann Intern Med, 1991; 114: 713-719.
- Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention and treatment of catheter-associatedurinary tract infection in adults: 2009 international clinical practice guidelines from the infectiousdiseases society of America. Clin Infect Dis, 2010; 50: 625-663.
- McGeer A, Campbell B, Emori TG, Hierholzer WJ, Jackson MM, Nicolle LE, et al. Definitions of infection for surveillance in long-term care facilities. Am J Infect Control, 1991; 19: 1-7.
- Johansen TEB, Botto H, Cek M, Grabe M, Tenke P, Wagenlehner FME, et al. Critical review of currentdefinitions of urinary tract infections and proposal for an European Association of Urology section for infections in urology classification system. Int J Antimicrob Agents, 2011; 38s: 64-70.
- Parry MF, Grant B, Sestovic M. Successfulreduction in catheter-associatedurinary tract infections: Focus on nurse-directedcatheterremoval. American Journal of Infection Control, 2013; 41(12): 1178–1181.
- Oman KS, Makic MBF, Fink R, Schraeder N, Hulett T, Keech T, et al. Nurse-directed interventions to reducecatheter-associatedurinary tract infections. American Journal of Infection Control, 2012; 40(6): 548–553.
- Espinasse F, Page B, Cottard-Boulle B. Risques infectieux associés aux dispositifs médicaux invasifs. Revue Francophone Des Laboratoires, 2010; 426.

