Platelet-to-Lymphocyte, Neutrophil-to-Lymphocyte, Lymphocyte-to-Monocyte and Aspartate-to-Alanine Aminotransferase Ratios in Carotid Artery Stenosis Underwent Stenting: Novel parameters in carotid artery stenosis
Yüksel Dereli1, Özgür Altınbaş2,*
1Necmettin Erbakan University, Meram Medical Medical Faculty, Department of Cardiovascular Surgery, Turkey
2Gaziantep University, Vocational School of Health Services, Department of Operating Room Services, Turkey
Received Date: 06/12/2021; Published Date: 28/12/2021
*Corresponding author: Özgür Altınbaş, Gaziantep University, Vocational School of Health Services, Department of Operating Room Services, Gaziantep, Turkey
Abstract
Backround: Atherosclerosis is the major risk factor in the development of arterial diseases. Carotid artery stenosis is one of the arterial diseases that may cause stroke or cranial ischemic infarction. Relationship between atherosclerosis and inflammation was revealed in the literature. Various parameters are used to detect the inflammatory process. In this study we aimed to discuss the association between platelet-to-lymphocyte, neutrophil-to-lymphocyte, lymphocyte-to-monocyte, aspartate-to-alanine aminotransferase ratios and carotid artery stenosis in patients who underwent carotid artery stenting.
Methods: Fifty-three patients who had carotid artery stenosis between 50%-70% and 53 healthy subjects with no carotid artery stenosis and additional chronically diseases were included to the study. Platelet-to-lymphocyte, neutrophil-to-lymphocyte, lymphocyte-to-monocyte, aspartate-to-alanine aminotransferase ratios were calculated and groups were compared in terms of these markers.
Results: Platelet-to-lymphocyte, neutrophil-to-lymphocyte and aspartate-to-alanine aminotransferase ratios were statistically significantly higher and lymphocyte-to-monocyte ratio was statistically significantly lower in patients with carotid artery stenosis.
Conclusion: Novel parameters included platelet-to-lymphocyte, neutrophil-to-lymphocyte, lymphocyte-to-monocyte and aspartate-to-alanine aminotransferase ratios are inexpensive, easy and reproducible methods in determining the prediction of carotid artery stenosis.
Keywords: Platelet-to-lymphocyte ratio; neutrophil-to-lymphocyte ratio; lymphocyte-to-monocyte ratio; aspartate-to-alanine aminotransferase ratio; carotid artery stenting
Introduction
Carotid Artery Stenosis (CAS) is a vascular disorder due to atherosclerotic process in carotid arteries. Although patients with carotid artery stenosis can be symptom free for several years, it may lead to worse outcomes like ischemic stroke, transient ischemic attack or other neurological problems [1]. Early detection, prevention and treatment of the disease are important because of its nature which may result in mortality and morbidity. Different imaging modalities include Duplex Ultrasound (DUS), Computed Tomography Angiography (CTA) and Magnetic Resonance Angiography (MRA) are used for these purposes [2]. Beside this, as the recent studies reveal the important role of the inflammation in the pathophysiological process of the atherosclerotic disease, novel laboratory parameters were started to be used in the early detection and the prediction of this course [3]. Platelet-to-lymphocyte (Plt/Lym), neutrophil-to-lymphocyte (Neut/Lym), lymphocyte-to-monocyte (Lym/Mono) and aspartate-to-alanine aminotransferase (AST/ALT) ratios are four of these novel markers for inflammation-associated diseases [4-7]. In this study we aimed to evaluate these four parameters in patients with CAS who underwent carotid artery stenting.
Methods
Between January 2019 and January 2021, 53 patients who underwent carotid MRA and who has stenosis over 50% and under 70% in the right or left internal carotid arteries with neurological symptoms and to whom carotid artery stenting were performed, were included to this study. Control group was consisted of 53 healthy subjects with no CAS or additional diseases. Written informed consent was taken from all participants and the Clinical Ethics Committee of the institution approved this retrospective study protocol with the decision no 2021-3339.
Decision of the carotid artery stenting was given in the council of the cardiovascular surgery and procedure was performed by the department of interventional radiology. Patients were followed in cardiovascular department after the procedure.
Clinical data about the accompanied diseases such as Diabetes Mellitus (DM), Coronary Artery Disease (CAD), Cerebrovascular Disease (CVD), Hypertension (HT), Peripheral Artery Disease (PAD) and Chronic Obstructive Pulmonary Disease (COPD) were recorded. Demographic data of the participants such as gender and age were also noted. All participants underwent carotid Doppler ultrasound and carotid MRA was performed to the patients additionally. The degree of stenosis was evaluated according to the North American Symptomatic Carotid Endarterectomy Trial (NASCET) 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCA Guideline on the Management of Patients with Extracranial Carotid and Vertebral Artery Disease Criteria [8].
Participants were divided into two; control group and patient group. Data from all patients were collected from hospital medical records.
Exclusion criteria were active infection, hematologic disease, chronic inflammatory or autoimmune diseases, any diagnosed cancer and renal failure.
Venous blood samples were obtained from participants for hemogram and biochemical analysis. Complete blood cell counts and automated differential counts were determined via an automated hematology analyzer (Cell-Dyn 3700, Abbott, Germany) which provided total white blood cells count, platelet, neutrophil, lymphocyte, monocyte, eosinophil, and basophils counts/ ml. The baseline Plt/Lym, Neut/Lym and Lym/Mono ratios were calculated by dividing the absolute counts of these parameters. Aspartate and alanine aminotransferases were determined via Cobas 8000, Roche, Germany and AST/ALT ratio was also calculated by dividing the absolute counts of these parameters.
Statistical Analysis
Data were expressed as mean±Standard Deviation (SD) or percentage. Statistical analysis was performed using GraphPad Instat version 3.05 (GraphPad Software Inc., San Diego, CA, USA). For comparisons of the differences between mean values of two groups, the unpaired Student’s t test was used. The Chi-square test was used for calculation of the significance of differences in gender. All statistical tests and p values were two-sided, and p<0.05 was considered statistically significant.
Results
Fifty-three patients with CAS and 53 healthy subjects were included to the study. There were no marked differences in the terms of age and the gender between the groups (Table 1).
Table 1: Comparison of demographical parameters between patients with CAS and control group.

Plt/Lym, Neut/Lym, Lym/Mono and AST/ALT ratios between the groups were compared and Plt/Lym, Neut/Lym and AST/ALT ratios are statistically significantly higher in patients than the control group. However, Lym/Mono ratio was statistically significantly lower in patients than the control group (Table 2).
Table 2: Comparison of the results of the Plt/Lym, Neut/Lym, Lym/Mono and AST/ALT ratios between the gruops.
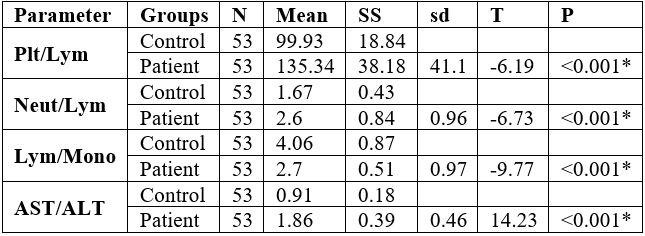
*p < 0.001
Plt: Platelet, Lym: Lymphocyte, Neut: Neutrophil, Mono: Monocyte
AST: Aspartate aminotransferase, ALT: Alanine aminotransferase
Discussion
Atherosclerosis is the most common underlying pathology of CAD, PAD and CVD. The main lesions in atherosclerosis are lipid deposition and fibrous matrix proliferation which develop into the formation of an atherosclerotic plaque that restricts blood flow and causes critical tissue hypoxia [9]. Several studies reveal the important role of the inflammation in all stages of the atherosclerotic process and atherosclerosis is usually considered a chronic inflammatory disease. Molecular and cellular pathways of inflammation promote atherosclerosis [10].
Several markers such as C-reactive protein, serum amyloid-A, fibrinogen, tumor necrosis factor-alpha, interleukin-Ia and interleukin-6 are used for determination of the inflammation [11]. In addition to these markers Plt/Lym, Neut/Lym, Lym/Mono and AST/ALT ratios are the recently introduced parameters used in detection of the inflammatory linked diseases [4-7].
Carotid artery stenosis is one of the diseases related with atherosclerosis and associated with inflammation. It is a main cause of stroke and treatment modalities usually include carotid endarterectomy and carotid artery stenting. Despite variety of diagnostic techniques, novel biochemical parameters can be used in the prediction and prognosis of the disease [12].
Plt/Lym ratio is initially served as a systemic biomarker to predict the prognosis of inflammation related disorders. Although higher platelet or lower lymphocyte counts accepted as the response to inflammatory stimuli, Plt/Lym ratio is more valuable than those alone in revealing inflammation [13]. Lymhopenia is usually detected in inflammatory states due to lymphocyte apoptosis. Thrombocytosis is also a common finding in inflammation as a result of increased proliferation in megakaryocytic series [14]. Integration of these clinical manifestations explains the association of higher Plt/Lym ratio with inflammation. Massiot et al [12] suggested that high Plt/Lym ratio was positively correlated with the degree of internal carotid artery stenosis and was an independent predictor of stroke. Similarly, in our recent study, Plt/Lym ratio is statistically significantly higher in the patients with CAS, than control group.
Neut/Lym ratio is a fast, easy and inexpensive method for evaluating inflammatory status and has been recently introduced biomarker for investigation of cardiovascular risk. Ratio of absolute neutrophil count to absolute lymphocyte count is used for the calculation of this marker [15]. Hyun et al [16] suggested that higher Neut/Lym ratios can be used in the prediction of carotid artery stenosis in patients with ischemic stroke. Positive correlation was found between high Neut/Lym ratio and carotid artery intima-media thickening in that study [16]. Koklu et al [17] emphasized that Neut/Lym ratio were higher in the symptomatic patients than those in the asymptomatic patients with intermediate CAS. Deser et al [18] revealed that in patients with severe CAS had higher Neut/Lym ratio and was positively correlated with the degree of the stenosis. Our study had parallel results with the literature that Neut/Lym ratio was statistically significantly higher in patients with CAS, who underwent carotid artery stenosis than control group.
Lym/Mono ratio has been recently introduced systemic inflammation parameter which could widely available and reproducible and can be calculated by dividing the absolute lymphocyte count to absolute monocyte count. Low Lym/Mono ratio has been found correlated with the severity of CAD and accepted as a risk factor for atherosclerosis [19]. Lym/Mono ratio integrates the lymphocyte and monocyte count into a single index and low value of this parameter shows significant data about the worse outcomes in patients with CAS in the literature. Park et al [20] revealed that low Lym/Mono ratio was associated with undesired outcome in patients with acute ischemic stroke. Gong et al [21] suggested that Lym/Mono ratio can be used in the prediction of clinical outcome in patients who had acute ischemic stroke. All the patients included to our study were symptomatic in terms of neurological signs and Lym/Mono ratio was statistically significantly lower than the control group.
AST/ALT ratio was first described by De-Ritis and being used to evaluate inflammatory status and vascular events recently. Ratio of absolute AST count to absolute ALT count is the calculation method of this marker [22]. Yokoyama et al. [23] studied the relation between the AST/ALT ratio and cardiovascular disease and emphasized that increased AST/ALT ratio was an independent predictor of all-cause and cardiovascular mortality. According to the study planned by Muzurovic et al. [24] there was a correlation between elevated AST/ALT ratio and PAD. Hoke et al. [25] emphasized that De-Ritis ratio could be used in risk scoring to predict outcomes after carotid artery stenting. In accordance with the literature De-Ritis ratio was statistically significantly higher in patients with CAS than control group in our study.
Conclusion
In conclusion platelet-to-lymphocyte, neutrophil-to-lymphocyte, lymphocyte-to-monocyte and aspartate-to-alanine aminotransferase ratios are easy, inexpensive, fast and reproducible parameters parameters that can be used in determining the prediction of carotid artery stenosis. We reached this conclusion using a retrospective study. Larger prospective and multicenter studies must be performed to explain the relationship between the CAS and these parameters.
Acknowledgement: We thank to Prof. Dr. Niyazi Gormus for his contributions to our manuscript.
Author contributions: Design, OA; Conceptualization and methodology, OA; Data collection, YD, OA; Data analysis and interpretation, OA, YD; Drafting the article, YD, OA; Revising and the final approval of the manuscript, OA, YD.
Conflicts of interest: The authors declared no conflicts of interest
Funding/Support: The authors received no specific funding for this work
Ethics considerations: Written informed consent was taken from all participants before the study. The study was conducted in accordance with the Declaration of Helsinki, and the Clinical Ethics Committee of Necmettin Erbakan University approved this retrospective study protocol with the decision no 2021-3339.
Study was conducted in Necmettin Erbakan University, Meram Medical Medical Faculty, Department of Cardiovascular Surgery, Konya, Turkey
References
- Krist AH, Davidson KW, Mangione CM, Barry MJ, Cabana M, Caughey AB, et al. US Preventive Services Task Force. Screening for Asymptomatic Carotid Artery Stenosis. US Preventive Services Task Force Recommendation Statement. JAMA, 2021; 325(5): 476-481.
- Saxena A, Lim ST. Imaging modalities to diagnose carotid artery stenosis: progress and prospect. BioMed Eng OnLine, 2019; 18: 66-89.
- Wang X, Xie Z, Liu X, Huang X, Lin J, Huang D, et al. Association of platelet to lymphocyte ratio with non-culprit atherosclerotic plaque vulnerability in patients with acute coronary syndrome: an optical coherence tomography study. BMC Cardiovasc Disord, 2017; 17: 175-184.
- Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD. The platelet-to-lymphocyte ratio as an inflammatory marker in rheumatic diseases. Ann Lab Med, 2019; 39(4): 345-357.
- Zhang WB, Zeng YY, Wang F, Cheng L, Tang WS, Wang WQ. A high neutrophil-to-lymphocyte ratio predicts hemorrhagic transformation of large atherosclerotic infarction in patients with acute ischemic stroke. Aging, 2020; 12(3): 2428-2439.
- Yayla C, Akboga MK, Yayla KG, Ertem AG, Efe TH, Sen F, et al. A novel marker of inflammation in patients with slow coronary flow: lymphocyte-to-monocyte ratio. Biomark Med, 2016; 10(5): 485-493.
- Kim HJ, Kim SY, Shin SP, Yang YJ, Bang CS, Baik GH, et al. Immunological measurement of aspartate/alanine aminotransferase in predicting liver fibrosis and inflammation. Korean J Intern Med, 2020; 35(2): 320-330.
- Brott TG, Halperin JL, Abbara S, Bacharach JM, Barr JD, Bush RL, et al. ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCA guideline on the management of patients with extracranial carotid and vertebral artery disease. J Am Coll Cardiol, 2011; 57(4): 16-94.
- Wolf D, Ley K. Immunity and Inflammation in Atherosclerosis. Circ Res, 2019; 124(2): 315-327.
- Geovanini GR, Libby P. Atherosclerosis and inflammation: overview and updates. Clin Sci, 2018; 132(12): 1243-1252.
- Saadeddin SM, Habbab MA, Ferns GA. Markers of inflammation and coronary artery disease. Med Sci Monit, 2002; 8(1): 5-12.
- Massiot N, Lareyre F, Pons AV, Pelletier Y, Chikande J, Carboni J, et al. High Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio are Associated with Symptomatic Internal Carotid Artery Stenosis. J Stroke Cerebrovasc Dis, 2019; 28(1): 76-83.
- Reda AA, Moharram MA, Rasheed AE. Platelet to lymphocyte ratio as a predictor of severity of coronary artery disease. Menofia Med J, 2019; 32: 167-171.
- Yuksel M, Yildiz A, Oylumlu M, Akyuz A, Aydin M, Kaya H, et al. The association between platelet/lymphocyte ratio and coronary artery disease severity. Anatol J Cardiol 2016;15(8):640-647
- Forget P, Kahfia C, Defour JP, Latinne D, VanPel MC, De Kock M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Research Notes, 2017; 10(12): 233-238.
- Hyun S, Kwon S, Cho SY, Park S, Jung WS, Moon SK, et al. Can the neutrophil-to-lymphocyte ratio appropriately predict carotid artery stenosis in patients with ischemic stroke?- A retrospective study. J Stroke Cerebrovasc Dis, 2015; 24(11): 2646-2651.
- Koklu E, Yuksel IO, Arslan S, Bayar N, Cagırcı G, Gencer ES, et al. Is elevated neutrophil-to-lymphocyte ratio a predictor of stroke in patients with intermediate carotid artery stenosis? J Stroke Cerebrovasc Dis, 2016; 25(3): 578-584.
- Deser SB, Yucel SM, Demirag MK, Guclu MM, Kolbakir F, Keceligil HT. The association between platelet/lymphocyte ratio, neutrophil/lymphocyte ratio, and carotid artery stenosis and stroke following carotid endarterectomy. Vascular, 2019; 27(6): 604-611.
- Ren H, Liu X, Wang L, Gao Y. Lymphocyte-to-Monocyte Ratio: A Novel Predictor of the Prognosis of Acute Ischemic Stroke. J Stoke Cerebrovasc Dis, 2017; 11: 2595-2602.
- Park MG, Kim MK, Chae SH, Kim HK, Han J, Park KP. Lymphocyte-to-monocyte ratio on day 7 is associated with outcomes in acute ischemic stroke. Neurol Sci, 2018; 39: 243-249.
- Gong P, Liu Y, Gong Y, Chen G, Zhang X, Wang S, et al. The association of neutrophil to lymphocyte ratio, platelet to lymphocyte ratio, and lymphocyte to monocyte ratio with post-thrombolysis early neurological outcomes in patients with acute ischemic stroke. J Neuroinflammation, 2021; 18: 51-62.
- Rief P, Pichler M, Raggam R, Hafner F, Gerger A, Eller P, et al. The AST/ALT (De-Ritis) ratio: A novel marker for critical limb ischemia in peripheral arterial occlusive disease patients. Medicine (Baltimore), 2016; 95(24): e5074.
- Yokoyama M, Watanebe T, Otaki Y, Takahashi H, Arimoto T, Shishido T, et al. 2016. Association of the aspartate aminotransferase to alanine aminotransferase ratio with BNP level and cardiovascular mortality in the general population: The Yamagata Study 10-year follow up. Dis Markers, 2016; 2016(1): 1-9.
- Muzurovic E, Lely AJ, Gurnell M. AST to ALT Ratio and Peripheral Arterial Disease in a Hypertensive Population- Is there a Link? Angiology, 2021; 20: 1-3.
- Hoke M, Ljubuncic F, Steinwender C, Huber K, Minar E, Koppensteiner R, et al. A validated risk score to predict outcomes after carotid stenting. Circulation, 2012; 5(6): 841-849.

