Tubes to Compare between Thromboelastogram Parameters in Patients with Congenital Dysfibrinogenemia
Xiang Liqun, Lin Faquan, Luo Meiling, Wu Yangyang, Yan Jie*
Department of Clinical Laboratory, the First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, China.
Received Date: 10/11/2021; Published Date: 06/12/2021
*Corresponding author: Yan Jie, Department of Clinical Laboratory, the First Affiliated Hospital of Guangxi Medical University, Nanning 530021, Guangxi, China
Abstract
Objective: To investigate the use of two different brands of sodium citrate vacuum blood collection tubes in determining the parameters of thromboelastography in patients with congenital dysfibrinogenemia (CD).
Methods: Venous blood specimens of 21 CD patients and 43 healthy controls were collected using Ruiqi or BD sodium citrate vacuum blood collection tubes. Thromboelastogram parameters (R, CI, fibrinolysis at 30 min after maximum amplitude [LY30], angle, and K) were compared using independent sample t test for comparing the means between the two groups.
Results: Significant differences were found between CD patients and healthy controls in R, LY30, and CI when blood was collected using the Ruiqi vacuum blood collection tube; and in R and CI, with BD vacuum blood collection tube (P<0.05). Comparing between Ruiqi and BD vacuum blood collection tubes, significant differences occurred in R, angle, and CI in CD patients (P<0.05); and in R, K, angle, LY30, and CI in healthy controls (P<0.05).
Conclusion: The comparability of R, angle, and CI measured in CD patients was poor when using Ruiqi and BD sodium citrate vacuum blood collection tube for thromboelastogram; therefore, a suitable sodium citrate vacuum blood collection tube should be chosen for assessing the risk of bleeding or thrombosis in patients with CD.
Keywords: Congenital dysfibrinogenemia; Vacuum blood collection tube; Thromboelastography; Bleeding, thrombosis
Introduction
Congenital Dysfibrinogenemia (CD), a qualitative disorder of fibrinogen, results from an abnormal fibrinogen molecular structure, and leads to dysfunctional blood coagulation. Its clinical manifestations are significantly heterogeneous, and include: no clinical symptoms, bleeding, or thrombosis. Female patients can also manifest with menorrhagia, placental abruption, repeated miscarriages, or abnormal postpartum bleeding [1]. Presently, there are limited literatures on CD treatment; therefore, the Hemophilia Centre Physicians’ Organization in the UK suggested a personalized treatment for CD, based on personal and family history [2]. For patients with personal or family history of thrombosis, low-molecular-weight heparin should be used for thromboprophylaxis. When bleeding occurs, fibrinogen infusion can be administered. If there is no evidence of bleeding or thrombosis, no special treatment is required except close observation and monitoring [3,4]. Therefore, accurate assessment of the risk of bleeding and thrombotic events in CD patients is key to treatment.
Thromboelastogram (TEG) is a method used for assessing the global hemostatic and fibrinolytic function. TEG simulates the human body environment, activates the coagulation system, and dynamically analyzes the whole process of blood clot formation, fibrin clot dissolution, clot firmness, and elasticity, via the thromboelastographic instrument [5]. Compared with the routine coagulation test, TEG provides a more comprehensive assessment of the body’s coagulation function. Currently, TEG plays an important role in guiding blood transfusion in trauma patients or pre-operatively [6,7], and its application in CD patients has gradually been promoted [8-10]. In order to provide more clinically accurate and reliable results, the quality control of TEG measurement is particularly important. The selection of vacuum blood collection tube is an important part of the quality control measures, before the experimental analysis. Therefore, in this study, using two different brands of sodium citrate vacuum blood collection tubes, TEG parameters were compared to determine the suitable vacuum blood sample collection tube to use in collecting blood to measure TEG and to accurately assess the risk of bleeding or thrombotic events in CD patients.
Materials and Methods
Study participants and study setting
Twenty-one patients diagnosed with CD in our hospital and 43 healthy controls were included in this study. The blood cell counts of the participants were normal; the liver and kidney functions were normal. None of the participants had diseases of the blood system, and none had recently used drugs that could affect the coagulation and anticoagulation systems.
Instruments and Reagents
Thromboelastometer Zy5000 and supporting reagents were supplied by Yi Zeyu Company (Shanxi Yuzeyi Medical Technology Co., Ltd.CN) and two lots of sodium citrate vacuum tubes were obtained from Ruiqi (Chengdu Ruiqi Technology Industrial Co., Ltd.CN) and BD(BectonDickinson, New Jersey, USA). The sodium citrate concentrations in both tubes were 3.2% (equivalent to 0.109 mol/L), respectively, and the ratio of the anticoagulant to blood was 1:9.
Procedure
After obtaining informed consent from each participant, 5mL fasting venous blood was collected, 1.8mL was loaded into the Ruiqi vacutainer tube, and 2.7mL was loaded into the BD vacutainer tube. The specimen was reversed 5-8 times and fully mixed, and the thromboelastogram was determined within 2 hours.
Statistical analysis
Data, expressed as the mean±standard deviation(`x±s), were analyzed by IBM SPSS Statistics for Windows, version 22.0(IBM Corp., Armonk, N.Y., USA). Independent sample t test was used to compare the means between the two groups (CD patients and healthy controls). The paired t test was used to compare data for the paired design. P<0.05 was regarded as statistically significant.
Results
Significant differences were found between CD patients and healthy controls in reaction time (R), fibrinolysis at 30 min after maximum amplitude (LY30), and coagulation index (CI) when blood was collected using Ruiqi vacutainer tube for blood collection; and R and CI when using BD vacutainer tube (P<0.05, Table 1).
Table 1: Comparison between TEG parameters measured in CD patients and healthy controls when using the same brand of blood collection tubes.
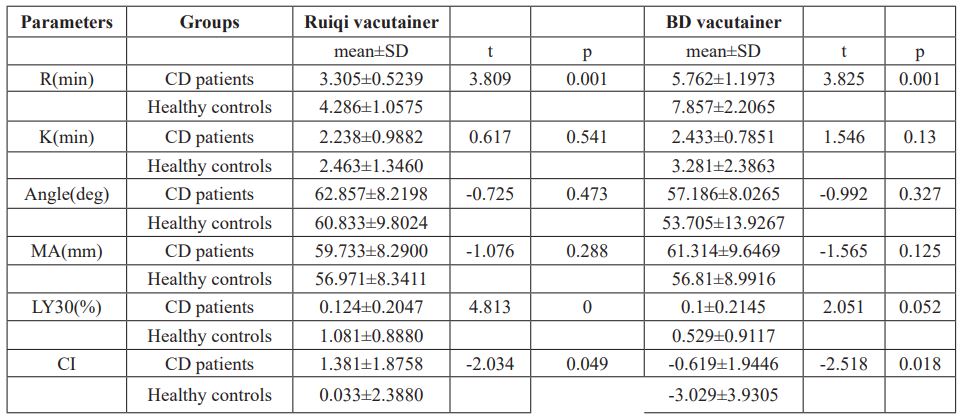
TEG, thromboelastogram; CD, congenital dysfibrinogenemia; R, reaction time; K, K time; MA, maximum amplitude; LY30, fibrinolysis at 30 min after maximum amplitude; CI, coagulation index
R, angle, and CI were significantly different between using Ruiqi and BD vacutainer tubes for blood sample collection in CD patients (P<0.05, Table 2); and R, K, angle, LY30, and CI between using Ruiqi and BD vacutainer tubes in healthy controls (P<0.05, Table 3).
Table 2: Comparison of TEG parameters in CD patients using the two brands of blood collection tubes.
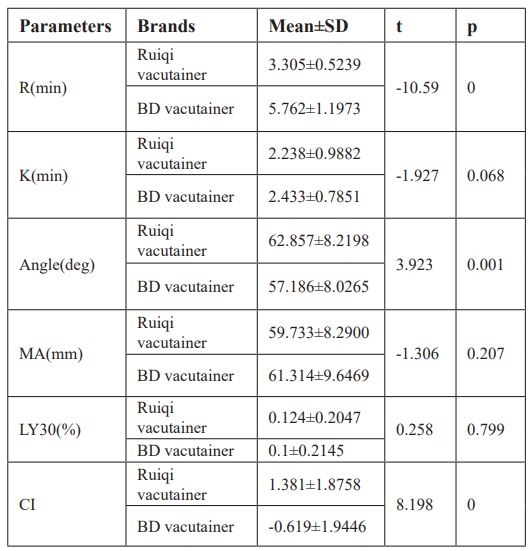
TEG, thromboelastogram; CD, congenital dysfibrinogenemia; R, reaction time; K, K time; MA, maximum amplitude; LY30, fibrinolysis at 30 min after maximum amplitude; CI, coagulation index
Table 3: Comparison of TEG parameters in healthy controls using the two brands of blood collection tubes.

TEG, thromboelastogram; CD, congenital dysfibrinogenemia; R, reaction time; K, K time; MA, maximum amplitude; LY30, fibrinolysis at 30 min after maximum amplitude; CI, coagulation index
Discussion
CD is characterized by blood coagulation dysfunction induced by abnormal fibrinogen molecular structure. Fibrinogen plays an important role in the coagulation process; first, thrombin recognizes and cleaves to the peptide bond of fibrinogen AαArg16-Gly17 and BβArg14-Gly15, and releases fibrin peptides A and B from the Aα and Bβ chains, respectively to form fibrin monomers. Second, fibrin monomers aggregate to form a soluble fibrin gel. Finally, with the help of coagulation factor ⅩⅢ and calcium, it is further cross-linked to form a stable fibrin clot. The physical properties of the blood clot (rate, hardness, and stability) will determine whether the patient has normal coagulation function or whether there will be bleeding or thrombosis [11,12]. TEG is an indicator that reflects the dynamic changes in blood coagulation, including the formation speed of fibrin, the dissolution state, the firmness and elasticity of coagulation. Therefore, it is widely used in the screening of various coagulation abnormalities pre- and post-operatively, to guide blood transfusion and medication [13]. It has also been widely used for the screening in CD diseases. It is of great value in the diagnosis, differential diagnosis, and evaluation of the coagulation status of CD patients, and provides more accurate information for the therapy of CD patients [14,15]. TEG can also be used to assess the risk of obstetric complications in women with dysfibrinogenemia (or hypodysfibrinogenemia) in the non-pregnant state [8]. Therefore, choosing a suitable vacutainer tube for TEG measurement and obtaining accurate and reliable experimental results are necessary for assessing the risk of bleeding or thrombosis in CD patients.
In this study, we used both Ruiqi and BD sodium citrate anticoagulation tubes to collect venous whole blood from CD patients and healthy controls for TEG measurement. The main monitoring indicators included R, K, angle, minimum amplitude (MA), LY30, and CI. When the Ruiqi vacutainer tube was used, significant differences were found in R, LY30, and CI between CD patients and healthy controls. When the BD vacutainer tube was used, differences occurred in R and CI between CD patients and healthy controls. The results showed that when the same sodium citrate vacuum blood collection tube was used, the R, measured by TEG in CD patients was shorter than that of healthy controls, whereas their CI was higher than that of healthy controls. R value refers to the time from the beginning of the detection to the amplitude of up to 20mm. This mainly reflects the comprehensive effect of all coagulation factors participating in the coagulation process, and can be used to reflect the activity of the coagulation factors. CI is the coagulation comprehensive index, which is used to describe the overall coagulation status of the patient. CI≤3 is considered as a hypocoagulable state, and CI≥3 is considered as the hypercoagulable state. CI is calculated based on R, K, angle, and MA. When the R time is shortened, CI is increased, indicating that the coagulation factor activity is strong and that the body is in a hypercoagulable state.
In CD patients, significant differences occurred in R, angle, and CI between Ruiqi and BD vacutainer tubes. In healthy controls, the differences in R, K, angle, LY30, and CI were statistically significant between Ruiqi and BD vacutainer tubes (P<0.05). This study showed that these two brands of blood collection tubes have a certain impact on TEG measurements in both CD patients and healthy controls; this is consistent with the results reported by Chinese scholars [16]. The sodium citrate vacuum blood collection tube produced by China Ruiqi Company, and used in this study, is made of single-layer glass, with a sodium citrate concentration of 0.109 M (3.2%) and a blood collection volume of 1.8 mL. When the blood specimen was collected, there was a 3 mL “dead space”. BD vacutainer tube is a small volume thick-walled double siliconized inner wall vacuum blood collection tube with a sodium citrate concentration of 0.109 M (3.2%), the blood volume of 2.7 mL, and almost no "dead space" after blood sampling. Studies have shown that the "dead space" of the sodium citrate vacuum blood collection tube can lead to partially activated and aggregated platelets, reduced coagulation factor Ⅹa activity, shortened activated partial thromboplastin time, and ultimately, reduced R value [17]. Studies have also shown that the high concentration of magnesium ions in the rubber stopper of the vacuum blood collection tube can activate certain coagulation factors, resulting in shortened prothrombin time and international normalized ratio measurements [18,19]. Since the quality of the blood collection tubes varies from manufacturer to manufacturer, this can lead to different magnesium ion concentrations in the rubber stoppers, and to inaccurate TEG results. Some scholars suggested that the magnesium ion concentration in the vacutainer tube should be less than 1 mmol/L [20]. In addition to the magnesium contamination, changes in the sodium citrate concentrations are other sources of pre-analysis errors. The anticoagulant concentration recommended by the National Committee for Clinical Laboratory Standardization (NCCLS) is 3.2% or 3.8% (equivalent to 0.109 mol/L or 0.129 mol/L), and the ratio of the anticoagulant to blood is 1:9. The sodium citrate vacuum blood collection tube maintains a stable vacuum to ensure that the ratio of blood to anticoagulant in the tube cannot be affected. The sodium citrate in the anticoagulant acts mainly as an anticoagulant by chelating with calcium ions in the blood sample. When the ratio of the anticoagulant is too low, it will increase the absolute concentration of calcium ions and shorten the clotting time. The K value reflects the coefficient of fibrin and platelets at the beginning of the clot formation, that is, it reflects the rate of clot formation. The K value is mainly affected by the level of fibrinogen, accounting for about 80%, and it is also affected by the function of the platelets, accounting for about 20%. The angle value is the result of the coefficient of fibrin and platelets at the beginning of the clot formation. It is closely related to the K value and reflects the rate of blood coagulation. In this study, the angle value measured by the Ruiqi vacutainer tube was larger than that of the BD vacutainer tube in both CD patients and healthy controls. The "dead space" of the vacutainer tube can cause the platelet to be partially activated and aggregate, which leads to an increase in the angle.
In this article, Ruiqi and BD sodium citrate vacuum blood collection tubes were used to measure TEG in CD patients and healthy controls, and then their parameters were compared. It was found that the R value of Ruiqi vacuum vascular collection was lower, the angle was larger, and its CI was lower than that of BD vacuum blood collection tubes in both CD patients and healthy controls. The plug of the BD vacuum blood collection tube was treated with low magnesium to prevent the activation of coagulation factors, and the double-layer tube wall helped to maintain its vacuum, and to effectively maintain the ratio of the anticoagulant to the blood. The clinical manifestations of CD patients are diverse, the TEG measurement helps to assess the blood coagulation level accurately, to assess the risk of bleeding or thrombosis, and provide guidance for the patient's replacement therapy. Therefore, it is necessary to choose a suitable vacutainer tube for TEG measurement and establish the TEG reference range for the laboratory, so as to provide accurate experimental data for the clinic.
Acknowledgments:
We would like to thank the Department of Hematology and Clinical Laboratory of the First Affiliated Hospital of Guangxi Medical University, China. We are grateful to all participants in this study.
Research funding:
This research was funded by the National Natural Science Foundation of China (grant number:81800130)
Author contributions:
Xiang Liqun analyzed the study data and wrote the initial draft of the paper; Luo Meiling designed the study; Wu Yangyang statistical experiment data; Yan Jie and Lin Faquan revised the article. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
Competing interests: The authors have no conflicts of interest to disclose.
Informed consent: Informed consent was obtained from all individuals included in this study.
Ethical approval:
This study was approved by the Medical Ethics Committee of No.6, Shuangyoyng Road, Qingxiu District, Nanning City, Guangxi, China.
References
- Yan J, Luo M, Cheng P, Liao L, Deng X, Deng D, et al. A novel mutation in the fibrinogen Aalpha chain (Gly13Arg, fibrinogen Nanning) causes congenital dysfibrinogenemia associated with defective peptide A release. International journal of hematology. 2017; 105: 506-514.
- Bolton-Maggs PH, Perry DJ, Chalmers EA, Parapia LA, Wilde JT, Williams MD, et al. The rare coagulation disorders--review with guidelines for management from the United Kingdom Haemophilia Centre Doctors' Organisation. Haemophilia : the official journal of the World Federation of Hemophilia. 2004; 10: 593-628.
- Casini A, Neerman-Arbez M, Ariens RA, de Moerloose P. Dysfibrinogenemia: from molecular anomalies to clinical manifestations and management. Journal of thrombosis and haemostasis: JTH. 2015; 13: 909-919.
- Mumford AD, Ackroyd S, Alikhan R, Bowles L, Chowdary P, Grainger J, et al. Guideline for the diagnosis and management of the rare coagulation disorders: a United Kingdom Haemophilia Centre Doctors' Organization guideline on behalf of the British Committee for Standards in Haematology. British journal of haematology. 2014; 167: 304-326.
- Polak F, Kolnikova I, Lips M, Parizek A, Blaha J, Stritesky M. New recommendations for thromboelastography reference ranges for pregnant women. Thrombosis research. 2011; 128: e14-17.
- Brazzel C.Thromboelastography-guided transfusion Therapy in the trauma patient. AANA journal. 2013; 81: 127-132.
- Olson JC. Thromboelastography-Guided Blood Product Use Before Invasive Procedures in Cirrhosis With Severe Coagulopathy: A Randomized Controlled Trial. Clinical liver disease. 2019;13:102-105.
- Zhou J, Xin Y, Ding Q, Jiang L, Chen Y, Dai J, et al. Thromboelastography predicts risks of obstetric complication occurrence in (hypo)dysfibrinogenemia patients under non-pregnant state. Clinical and experimental pharmacology & physiology. 2016; 43: 149-156.
- Galanakis DK, Neerman-Arbez M, Brennan S, Rafailovich M, Hyder L, Travlou O, et al. Thromboelastographic phenotypes of fibrinogen and its variants: clinical and non-clinical implications. Thrombosis research. 2014; 133: 1115-1123.
- Zhou J, Ding Q, Chen Y, Ouyang Q, Jiang L, Dai J, et al. Clinical features and molecular basis of 102 Chinese patients with congenital dysfibrinogenemia. Blood cells, molecules & diseases. 2015; 55: 308-315.
- Weisel JW, Litvinov RI. Mechanisms of fibrin polymerization and clinical implications. Blood. 2013; 121: 1712-1719.
- Lord ST.Molecular mechanisms affecting fibrin structure and stability. Arteriosclerosis, thrombosis, and vascular biology. 2011; 31: 494-499.
- Jody, Olson. Thromboelastography-Guided Blood Product Use Before Invasive Procedures in Cirrhosis With Severe Coagulopathy: A Randomized Controlled Trial.
- Neerman-Arbez M, de Moerloose P, Casini A. Laboratory and Genetic Investigation of Mutations Accounting for Congenital Fibrinogen Disorders. Seminars in thrombosis and hemostasis. 2016; 42: 356-365.
- Wei A, Liao L, Xiang L, Yan J, Yang W, Nai G, et al. Congenital dysfibrinogenaemia assessed by whole blood thromboelastography. Int J Lab Hematol. 2018; 40: 459-465.
- Liu Yan, Zhao Zhonghua. The influence and analysis of domestic blood coagulation tube and American BD blood coagulation tube on the parameters of thromboelastography, labeled immunoassay and clinical [J]. 2017; 24: 1313-1315+1320.
- Toulon P, Abecassis L, Smahi M, Ternisien C. Monitoring treatments with unfractionated heparin: CTAD must be used instead of citrate as the anticoagulant solution when using partial-draw collection tubes. Results of a multicenter evaluation. Thrombosis research. 2010; 126: 536-542.
- van den Besselaar AM, van Vlodrop IJ, Berendes PB, Cobbaert CM. A comparative study of conventional versus new, magnesium-poor Vacutainer(R) Sodium Citrate blood collection tubes for determination of prothrombin time and INR. Thrombosis research. 2014; 134: 187-191.
- van den Besselaar AM.Magnesium and manganese ions accelerate tissue factor-induced coagulation independently of factor IX. Blood coagulation & fibrinolysis : an international journal in haemostasis and thrombosis. 2002; 13: 19-23.
- van den Besselaar AM, van Zanten AP, Brantjes HM, Elisen MG, van der Meer FJ, Poland DC, et al. Comparative study of blood collection tubes and thromboplastin reagents for correction of INR discrepancies: a proposal for maximum allowable magnesium contamination in sodium citrate anticoagulant solutions. Am J Clin Pathol. 2012; 138: 248-254.

