Comparison of Classification for Headache Disorders Between Western Medicine and Traditional Chinese Medicine
Saroj K. Pradhan, Yiming Li, Yiliang Zhang, Andreas R. Gantenbein
TCM-Klinik Ming Dao Bad Zurzach / ZURZACH Care, Research Department Rehaklinik Bad Zurzach, Switzerland
Swiss TCM Academy, Research Department Bad Zurzach, Switzerland in Collaboration with Department of Research, Nanjing University of Chinese Medicine, Nanjing, China
ZURZACH Care, Neurology & Neurorehabilitation Department Rehaklinik Bad Zurzach, Switzerland
Received Date: 14/10/2021; Published Date: 11/11/2021
*Corresponding author: Saroj K. Pradhan, TCM-Klinik Ming Dao, ZURZACH Care, Research Department Rehaklinik Bad Zurzach, Switzerland, Quellenstrasse 31, CH-5330 Bad Zurzach, Switzerland.
Email: s.pradhan@tcmmingdao.ch
Abstract
Headache disorders (HD) are the most common neurological disorder and affect all ages, gender, and ethnicity. HD implicates huge economic costs worldwide, and has a significant impact on the quality of life for all the individuals concerned. The currently valid international headache classification is «The International Classification of Headache Disorders, 3rd edition» (ICHD-3) and has precise diagnostic criteria for each HD. To date similarly to the systematic classification of ICHD-3 is still lacking in Traditional Chinese Medicine (TCM).
A comprehensive online database search using PubMed, Cochrane Library, CNKI, Google Scholar, literature research regarding HD and its classification was performed to identify relevant references, investigating the classification of HD in Western medicine (WM) and TCM. The results were analyzed, classified and evaluated.
This paper highlights the comparison of classification for HD between WM and TCM and provides a basis for the understanding of the two systems of health care in the classification of HD.
Keywords: Headache disorders, Western medicine, Chinese medicine, classification of headache disorders
Introduction
Headache Disorders (HD) are one of the oldest maladies since the existence of humankind [1]. Studies of trephined prehistoric skulls provided findings of trepanation of Neolithic skulls indicating numerous techniques in the surgical treatment for health issues, shows the importance of HD for over 7000 years ago [2].
Around 4000 BC to 3000 BC, an unknown Sumerian author described in a poem that headache occurs in connection with visual disturbances [3].
Hippocrates (460-370 BC) mentioned seizure-like headaches, which are initiated by visual symptoms and ended by vomiting. However, he was not able to recognize migraine as an independent disease entity and to distinguish it from headaches of another genesis [4].
The earliest mention of headache in China was found on oracle bones during the Shang Dynasty around 1600 BC-1046 BC. It was described as Ji Shou, 疾首, headache caused by anger [5]. In AD 1529 the term migraine was documented for the first time in China and HD was classified into two types. Namely according to the invasion of exogenous pathogenic factors and the internal deficiency [6].
Approximately about 1500 BC Egyptian medical documents reported records of migraine-like headaches and suggested treatment for this ailment [7]. The Egyptians thought the cause of headache is related to the work of an evil spirit. The heated head was cooled by the application of moistened mortar to the head. Another therapy derived from Egyptian mythology is a combination of coriander, wormwood, juniper, honey, and opium. The use of willow leaves is cited in treatment for an inflammatory condition: Salicylic acid is derived from willow bark, and its use led to the discovery of aspirin [8].
In «The Inner Canon of the Yellow Emperor, Ling Shu, Chapter 42, Discourse on Wind» during the Han-Dynastie around 200 BC-AD 200 headache is described as 首风, Shou Feng, Wind in the head or Nao Feng, 脑风 [9].
Headaches have been narrated and investigated since the history of humanity. It has been analyzed and tried to be classified since antiquity and further
categorization followed over the centuries. We aimed to provide a comprehensive understanding of the difference between the two systems of health care in the comparison of classification for HD in this study.
Western Medicine Classification
Gaius Plinius Secundus, also known as Pliny the Elder, (AD 23-79) recommended the first headache categorization indicating distinct pain localization i.e., headache
involving the entire head, temporal or occipital [10], and besides he even suggested the application of medicinal herbs for the alleviation of headache [11].
The Greek doctor Aretaeus of Cappadocia, approximately 1st part of 2nd
centennial, made a basal distinction between three types of major headaches and contributed very early to HD classification [12]:
- Heterocrania: half-sided extremely painful headache, wavering in different head areas and periodically followed by nausea, bilious vomiting, and fainting. Aretaeus then interpreted migraine as heterocrania [13]. Due to the lack of medicine for HD at that period the treatment was limited to bloodletting and laxative [14,15].
- Cephalea: chronic, intense headache and often difficult to treat [1].
- Cephalalgia: a mild, short duration of headache. Dangerous if correlated with fever, coldness, or decreased muscle tone [13,16]. His findings contributed basally to the international classifications of the International Headache Society regarding
the categorization of migraine from tension-type headache [17].
The famous Greek physician Galen of Pergamum, who lived around AD 129–199, also categorized headache into three various types: [18].
- Cephalgia: a mild, short duration of headache
- Cephalea: chronic, constant pain, with photophobia as a concomitant feature [1].
- Heterocrania: pounding headache with sudden attacks [1].
He was the first physician to use the term heterocrania, which was later known
as ʻhemicraniaʼ. He assumed that excessive heat or cold could be a triggering aspect for headaches. Galen of Pergamum presumed an individual’s health relied on a personal balance or disharmony of four fluids, namely black bile, blood, humors, and phlegm [19]. His entrenched pattern carried on until the 17th century.
Caelius Aurelianus (5th century) described cephalgia as an acute headache
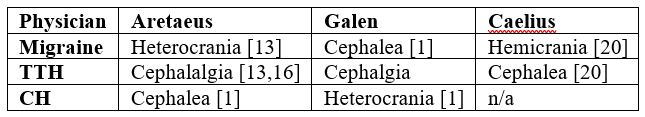
followed by fever. Hemicrania was characterized by pulsating pain with dizziness, nausea, or emesis and cephalea was a chronic, sequential headache without fever [20]. Table 1 presents the historical definition/naming of the most prevalent primary and secondary headaches.
The neuroanatomist Thomas Willis (AD 1621-1671) from England was a pioneer of contemporary clinical neurology. Continuous headache, intermittent headache, and intermittent headache with vague and uncertain attacks [21] were the three common forms of headache he had distinguished at his time.
Samuel Auguste Tissot (AD 1728-1797), a renowned physician from Switzerland provided clinical insight on migraine in his work «Treatise on the nerves and nervous disorders» [22]. He differentiated between migraine, cephalalgia, cephalaea, and parietal or occipital headache and narrated precisely the recurrence and the pattern of migraine outbreaks [23]. Tissot discovered the involvement of the nervous system in migraine. As a result, he described hemianopia (half-sided blindness), hemiplegia (unilateral or hemiplegic paralysis), and aura [22].
An assistant of the famous physician Herman Boerhaave in Leiden (AD 1668- 1738) named Gerhard van Swieten (AD 1700-1772) composed in AD 1745 several volumes of influential medical textbooks discussing on the scripts of Herman Boerhaave. The content included a fundamental explanation known to date of episodic cluster headache (ECH), which conforms to the benchmark of the International Headache Society of AD 1988 for ECH [24].
An English physician named Edward Liveing (AD 1832-1919) presented new theories on migraine pathogenesis in his book «On Megrim» [25] which was published in AD 1873. His work, a collection of clinical elements, can be regarded as an essential text for neurological comprehension of migraine. He characterized migraine as an appearance of ʻnerve-storm’ and interpreted it as riddance of exuberance nerve-force through the body and brain [26].
Emil du Bois-Reymond (AD 1818-1896) interpreted migraine in AD 1860 as tetany of the vascular muscles and conjectured the pain was induced by the elevated blood pressure against the vessel walls. He also assumed migraine was an ailment of the centrum ciliospinale in the Medulla spinalis [27].
The British neurologist William Richard Gowers (AD 1845-1915) was a pioneer in modern neurology [28]. He was one of the first leading person segregating migraine treatments into abortive or preventive [29]. His, at that time a modern
textbook in neurology, «Manual of Diseases of the Nervous System (AD 1886– 1888)» categorizes every facet of neurological disorder formulated in a pattern according to their section. The book distinguishes epilepsy and headache and contains information about performing the appropriate neurological diagnosis [30].
The first «International Classification of Headache Disorders» (ICHD) was published in AD 1988 and updated in AD 2004 [31]. The currently valid ICHD-3 was published in AD 2018. It distinguishes more than 250 types of headaches, which are divided into primary, secondary, neuropathies & facial pains, and other headaches [32].
The three most common types of primary headaches are Tension-Type Headache (TTH), migraine, and Cluster Headache (CH), whereas migraines and CH are the most important primary headaches in a clinical context, with Medication-Overuse Headache (MOH) being the most important secondary type [33]. The cause of primary headaches to date is still not very clear.
Table 1: Historical definition of most prevalent HD.
Traditional Chinese Medicine Classification
Differentiation of syndromes in Traditional Chinese Medicine (TCM) is carried out by fact-finding and classifying of the indication achieved from the four TCM diagnostic techniques (inspection, listening-smelling, inquiry, and pulse-taking/palpation).
These steps must be followed to evaluate the persons' health status and determine the syndrome [34]. The resulting diagnosis for HD relies on multiple factors comprising knowledge of the area of pain to correlate with the respective meridian and to deduce a connection to the affected internal organ. Understanding the quality of pain, exogenous, endogenous noxae and internal disorders [35] is advantageous to distinguish more about the pathogenesis. Each and all of these aspects must be examined to receive a concluding TCM diagnosis [36].
TCM categorizes HD evoked by exogenous factors or by internal disorders.
Headache and different ailments on the head are subject of repletion in the superior and depletion of the inferior part of the body according to «The Inner Canon of the Yellow Emperor, Ling Shu, Chapter 10, The Function of the Five Viscera to the Human Body and Their Mutual Relations» [37]. Nine types of headaches due to the pathological upward movement of qi and their treatment are also mentioned in the same textbook in chapter 24. But the description of the arise of symptoms and their pathophysiology is not provided [38].
Classification according to the acupuncture meridian system
In a modern scientific point of view of the meridians, also described by Unschooled as conduit pathways [9], are similar to the conception of a sophisticated structure of neurovascular bundles and their minor extensions in the sense of Western Medicine (WM). This complicated meridian network system links the muscles, extremities, bones, joints, and including all organ systems. By implication connected the entire body structures as one unit. Nevertheless, it still differs from the neurovascular system and physiology as defined by the WM [39,40].
Although the pathophysiology of migraine is not completely understood, it is well accepted that migraine pain can be triggered by the activation of trigeminal ganglia neurons and their nerve fibers, which innervate cranial meninges [41]. In TCM, this nociceptive trigeminal activation belongs to the Yang category. Yang is heat, light, motion, excitation, ascending, and dispersing nature, whereas Yin is cold, darkness, tranquility, inhibitory, descending, and astringing [42]. In the Textbook «Treatise of Cold Damage Disorder» passages No.13, 28, 35, 38, 56, 92, 142, 265, 378 Zhang Zhong Jing classified HD according to the six-stages pattern for the first time [43].
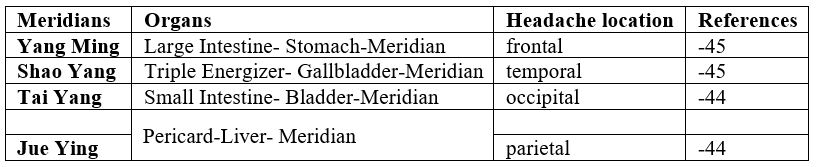
Table 2 provides the classification according to the acupuncture meridian system the following meridians are affected in HD:
- Yang Ming [Large Intestine-Stomach-Meridian]: Affected patients often suffer from digestive disorders [44]. The pain is located in the frontal area, comparable to tension headaches [45].
- Shao Yang [Triple Energizer-Gallbladder-Meridian]: As a result of fire stasis in the Shao Yang meridian and ascending gallbladder-fire, headache with vertigo, difficulty to sleep, uneasiness in the thoraco-abdominal area arise [46]. The pain occurs temporal and resembles a migraine [45]. These patients tend to be
emotionally unstable [44].
- Tai Yang [Small Intestine-Bladder-Meridian]: mostly connected with spinal Patients usually have complaints regarding pain in the occipital area, similar to occipital neuralgia [44].
- Jue Ying [Pericard-Liver-Meridian]: The pain is Patients feel exhausted with no energy [44].
Table 2: Classification according to the acupuncture meridian system.
Classification of headache according to TCM organ system
TCM has evolved the theory of functional systems and describes physiology referring to different functional organ systems. Even though these functional organ systems are called the same as the anatomical organs of biomedicine, their functions are
different and not similar to the modern anatomical morphology [47]. The theory of the
Zang-Fu organ in TCM illustrates all organ systems and the external indications of
their functional and pathological condition. Zang organs consist of liver, heart, spleen, lung, kidney, and Fu organs contain gallbladder, small intestine, stomach, large intestine, bladder, and triple burner [48]. Every Zang organ is linked to a Fu organ
through a meridian system. The Zang organs produce, transform and cumulate the essence whereas the Fu organs have a digesting, transporting, and discharging
function. Brain, marrow, vessels, gallbladder, bones, and the uterus belong to
extraordinary organs [49]. The fundamental elements for developing and preserving the physiological mechanism of the Zang-Fu organs are Yin, Yang, Qi, and blood.
Every pathological alteration is an outcome of insufficiency or misbalance of these components [50].
Table 3: TCM Classification according to the pathogenesis.

Disharmony pattern in the Zang-Fu organ system
- Hyperactivity of Liver Yang: According to the Zang-Fu organ theory, the physiological aspect of the liver is to store yin-blood. It also regulates the unimpeded movement of the qi and smooth circulation of blood and Within this context,this means the liver conducts the activity of qi, balances mental activity i.e., anger and mood, management of the upward movement of spleen qi, and distribution action of stomach qi [51]. Prolonged emotional disbalance, especially anger and resentment, which is governed by the liver, leads to liver qi stagnation. Deficiency of Yin blood, results in an excess of liver Yang qi, causing liver Yang qi with blood to ascend towards the head, evoking HD. This outcome is because the dredging and soothing function of the liver becomes pathological [52].
- Kidney deficiency: In TCM the physiological function of the kidney is to store essence, controls growth, development, and reproduction. It is also responsible to govern water and bones, generate marrow, transform blood, deal with the reception of qi, sustain and warm the Zang-Fu organs [53]. The decrease of kidney Yang, its deficiency in fostering the body, decay of kidney Yin as an outcome of overextension and chronic disease and depletion of kidney essence provokes kidney deficiency, leading to
- Spleen deficiency: The spleen is the source of qi, blood, and fluid. As a physiological function, the spleen controls the transformation and transport, supplying nutrients for muscle and energy Its hemopoietic function manages blood and is responsible for proper circulation in the vessels [54]. Improper diet, continuous overthinking, exhaustion debilitate the spleen, leading to spleen qi deficiency and decline in the function of transformation and transport [55]. The spleen qi is incapable to arise adequately to the head and symptoms like vertigo, fatigue, and headache occur [56].
Classification according to TCM pathogenesis
Wind, cold, heat, and dampness are associated with the six elements also known as six qi [wind, cold, heat, dryness, dampness, and summer heat] of the natural environment in TCM [57]. Unusual and sudden changes of these elements are regarded as six pathogenic exogenous factors (six excess) syndromes [58].
According to TCM pathogenic mechanism theory, the manifestation of diseases can be determined by the influence of six pathogenic exogenous factors, retention of phlegm, blood stasis, improper diet, and life habit. If the immune system becomes weak, the adaptability of the human body is overstrained, and due to the inability of the body to adjust to the alteration of these mentioned factors diseases breakout [59]. In TCM theory of six qi, the wind is Yang in nature and always in movement.
Cold is the Yin category. Pathological cold coagulates Yang-qi, blood, and fluid, which leads to abnormal tightening of muscles, tendons, and vessels [60]. The classification according to TCM pathogenesis is presented in Table 3.
Wind-Cold headache: Wind belongs to the pathogenic factor of Yang. According to the theory of «Huang Di Nei Jing—Su Wen», the head is the highest segment of the body and is the confluence of all yang-meridians [61]. The head can be easily and quickly invaded by the pathogenic exogenous Through the
attack of the pathogenic exogenous wind in the head, Yang qi is inhibited. Qi and blood in the meridians and network vessels tend to coagulate, leading to pain due to obstruction of the Tai Yang conduit pathway. Occipital, - neck-, and back pain are mostly the symptoms occurring in an intermittent intermission [62].
Wind-Heat headache: Heat as a Yang category ascends. Unresolved wind- cold converted into pathogenic heat or wind linked with pathogenic heat affecting the Yang meridians gives rise to inflated pain induced by pathogenic wind-heat [63].
Wind-Dampness headache: Pathogenic exogenous wind associated with dampness penetrates the head and blocks the orifices. The manifestation is a head feeling tightly compressed, burdensome extremities, less desire for food, abdominal fullness, tiredness, chest tightness, and voiding dysfunction. This pathogenesis is attributable to the malfunction of the spleen because dampness amasses in the middle burner preventing the spleen to control its transformation and transportation mechanism [62].
Qi and blood insufficiency headache: Qi belongs to Yang and blood to Yin The affiliation between them is a relationship between Yin and Yang. Qi controls the flow of blood whereas blood is the origin for qi alteration. Qi and blood insufficiency consequently result in a diminished function and nutrition deficiency of the Zang-Fu organs related to the meridian network system. Pale complexion,
fatigue, dizziness, sleeplessness, chronic headache, thin, and weak pulse are the outcome of qi and blood insufficiency [64].
Phlegm retention headache: Phlegm is classified as Yin. Misbalance and assemble of fluid in the body is induced by six excesses, overstrain, laze, incorrect or irregular Enduring emotion disturbances initiate the malfunction of qi
transformation and generate phlegm. The organs, lung, liver, spleen, kidney, and the triple burner get then negatively affected in their physiology. This impaired mechanism obstructs the meridians and blocks the circulation of qi and blood.
Dizziness, headache, chest distress, breathlessness, nausea, and emesis are the attribute of phlegm retention headache [65].
Blood stasis headache: The pathological blood flow in the meridians, network vessels and Zang-Fu organs causing confinement of the blood leads to blood stasis. The cold of the six excess is likely to contract the blood vessels and obstruct them, letting blood stasis occurs. Blood stasis also arises, because the overabundance of pathogenic heat makes the blood pour out of the vessels. Injuries, qi insufficiency, qi stagnation, hemorrhage all influence the development of blood stasis. Blood stasis headache is marked by dull and stabbing pain, fixed location, and aggravating at night [66,67] and the pain is persistent and hard to be relieved [68].
Discussion
The World Health Organization (WHO) survey showed that in the past few years, people suffering from HD have reached 50% of the global population. Among these people, 30% or more proclaimed suffering a migraine. Nearly half of adults have had at least once in their life headache. According to the WHO, 1.7- 4% of adults worldwide endure headache attacks 15 or more days monthly [69].
The Global Burden of Diseases, Injuries, and Risk Factors (GBD) studies came to the finding that around three billion people suffered from migraine or TTH in AD 2016. TTH was the third common and migraine the sixth in AD 2016 of all GBD causes of disease [70]. This condition reveals that headache is a major global burden affecting the patient’s work, quality of life, and having a massive impact on the rising of health insurance costs and straining the national economy [71].
Besides migraine, TTH, MOH, trigeminus neuralgia, and CH are among the most important headache types [33]. TTH, episodic and chronic [72] are the most typical types of primary headache [73].
Around one million people in Switzerland are affected by migraine with an estimated migraine prevalence of 10–15% [74]. HD in China surged from around 112.4 million individuals in AD 1990 to 482.7 million individuals in AD 2017. In the years lived with disability, people with migraines [5.5 million) were superior to TTH persons in China [1.1 million) [75]. All over the world, HD is very common symptoms in primary health care [76]. Moreover, it is often difficult and challenging for an unexperienced physician in HD to precisely classify different types of HD to make the exact diagnosis due to different pathophysiology [77,78]. Particularly in primary headache, the classification is not based on laboratory medical tests but only on anamnesis criteria, therefore it is predestined for classification.
As a disease, HD is often underestimated, misdiagnosed or not treated properly [79]. Consequently, HD must be taken seriously including accurate assessment and diagnosis.
TCM is considered as an ancient holistic medicine originating through evidence by tradition, whereas modern WM is rather more resulting from evidence-based medicine. Although, the TCM classification is a historical categorization based on empirical and phenotypic experience, there are some similarities respectively to the ICHD-1 classification, which mainly includes phenotypic viewpoints of experts over a period of 30 years [32]. By adapting to scientific evidence, pathophysiology, and clinical findings, the ICHD-1 has been aligned over the past decade and all adaptations in the latest version of ICHD-3 are based on such findings.
Conclusion
In conclusion, the TCM classification in HD is predominately orientated on TCM pathogenesis, disharmony patterns in the Zang-Fu organ system, and meridian systems. Its differentiation derived from ancient times and has not been greatly modified to date. Considering the historical development of the ICHD, the current
ICHD-3 is now designed based on scientific evidence and research. However, to date similarly to the systematic classification of ICHD-3 is still lacking in TCM.
Physicians compile a diagnosis derived from their diagnostic methods to design the therapy concept for the affected person. Therefore, an adequate therapy and the precise diagnosis should be of importance for the HD patient.
This study can be used by physicians and therapists involved in TCM in understanding the comparison of the two systems of health care in the comparison of classification for HD.
The combination of TCM and WM in clinical trials have shown evidence that the collaboration of these two medical treatment paradigms is more efficient than monotherapy [80–83].
References
- Guerrero-Peral ÁL, de Frutos González V, Pedraza-Hueso MI. Galeata: chronic migraine independently considered in a medieval headache classification. J Headache Pain, 2014; 15[1): 16.
- Petrone P, Niola M, Di Lorenzo P, Paternoster M, Graziano V, Quaremba G, et al. Early Medical Skull Surgery for Treatment of Post-Traumatic Osteomyelitis 5,000 Years Ago. Rosenberg K, editor. PLOS ONE, 2015; 10[5): e0124790.
- Schalke HP. Zur Klinik und Klassifikation der Migräne. Der Schmerz. Springer Verl. 1989; 171-179.
- Critchley M. Background to migraine. Migraine Cappadocia Queen Sq. 1967; 1: 28-38.
- Schwartz AC. The Oracle Bone Inscriptions from Huayuanzhuang East Translated with an Introduction and Commentary. In Boston: Walter de Gruyter Inc; 2019; p. 291.
- Xiao N. Shang Han Za Bing Lun. Study of diagnosis and treatments of Treatise on Febrile Diseases. Hubei Univ Chin Med, 2007; 35.
- Assina R, Sarris CE, Mammis A. The history of craniotomy for headache treatment. Neurosurg Focus. 2014; 36[4).
- Diamond S, Franklin MA. Introduction–The History of Headache. In: Headache and Migraine Biology and Management. Elsevier, 2015; p. 1–12.
- Unschuld PU, Tessenow H, Zheng J. Prolegomena. In: An Annotated Translation of Huang Di’s Inner Classic – Basic Questions. Berkeley Los Angeles: Oxford University Press, 2011; p. 15.
- Zanchin G. Chapter 25 Headache. An historical outline. In: Handbook of Clinical Neurology. Elsevier B.V., 2009; 25: p. 375–86.
- Stannard J. History and Philosophy of the Life Sciences on JSTOR, 1982; 4[1): p. 13–23.
- Koehler PJ, Van de Wiel TWM. Aretaeus on migraine and headache. Journal of the History of the Neurosciences, 2001; 10: p. 253-261.
- Magiorkinis E, Diamantis A, Mitsikostas DD, Androutsos G. Headaches in antiquity and during the early scientific era. Journal of Neurology. Springer, 2009; 256: p. 1215-1220.
- Pearce JMS. Historical aspects of migraine. Journal of Neurology, Neurosurgery and Psychiatry. BMJ Publishing Group, 1986; 49: p. 1097–1103.
- Pearce JMS. The Neurology of Aretaeus: Radix Pedis Neurologia. Eur Neurol, 2013; 70[1–2): 106-112.
- Isler H. Kopfwehgeschichten. In: Agosti R, Diener HS, Limmroth V, editors. Migräne und Kopfschmerzen Ein Fachbuch für Hausärzte, Fachärzte, Therapeuten und Betroffene. Basel: Karger; 2015; p. 349.
- Isler H, Koehler PJ. General Aspects of the Headaches ◗ History of the Headache ANCIENT MESOPOTAMIA, EGYPT, CLASSICAL GREECE, AND ROME: HEADACHES AS A MAJOR PROBLEM, 2005.
- Pearce JMS. A headache history. Brain, 2012; 135[8): 2569-252.
- Evans EC. Galen the Physician as Physiognomist. Trans Proc Am Philol Assoc, 1945; 76: 287.
- Eadie MJ. Headache and its classification. In: Headache: Through the Centuries. New York: Oxford University Press, 2012; p. 5.
- Isler H. Thomas Willis’, Two Chapters on Headache of 1672: A First Attempt to Apply the “New Science” to this Topic. Headache J Head Face Pain, 1986; 26[2): 95–98.
- Pearce JMS. Samuel-Auguste Tissot [1728–1797) and Migraine. Cephalalgia, 2000; 20[7): 668-670.
- Karbowski K. Samuel Auguste Tissot [1728-1797) His research on migraine, J Neurol, 1986; 233[2): 123–125.
- Pearce JMS. Gerardi van Swieten: Descriptions of episodic cluster headache. Journal of Neurology, Neurosurgery and Psychiatry. BMJ Publishing Group, 2007; 78: p. 1248-1249.
- On Megrim, Sick-headache, and same allied disorders, a contribution to the pathology of Nerve-Storms. The Indian Medical Gazette. Pandeya Publications, 1873; 8.
- Barnett R Migraine. The Lancet, 2019; 394[10212): 1897.
- Koehler PJ. Brown-Séquard’s Comment on Du Bois-Reymond’s “Hemikrania Sympathicotonica.” Cephalalgia. 1995; 15[5): 370–372.
- Lochte BC, Beletsky A, Samuel NK, Grant I. The Use of Cannabis for Headache Disorders. Cannabis Cannabinoid Res, 2017; 2[1): 61–71.
- Simona Liliana Sava, Schoenen J, Martens de Noordhout A. Interrelations between the cerebral cortex and the trigeminal system: studies in healthy subjects and in migraine patients; therapeutic perspectives, 2016.
- Swash M. Sir William Gowers: a life in neurology. Brain, 2012; 135[10): 3189-3191.
- Olesen J. The international classification of headache disorders. 2nd edition [ICHD-II). In: Revue Neurologique. Elsevier Masson SAS, 2005; p. 689-691.
- IHS. Headache Classification Committee of the International Headache Society [IHS) The International Classification of Headache Disorders, 3rd edition. Vol. 38, Cephalalgia. SAGE Publications Ltd, 2018; p. 1–211.
- Schipper S, Gantenbein AR. Starke Kopfschmerzen. Abklärung und Therapie in der Hausarztpraxis. ARS MEDICI, 2013; [4): 17–23.
- Wang S-J, Yue W, Rahman K, Xin H-L, Zhang Q-Y, Qin L-P, et al. Mechanism of Treatment of Kidney Deficiency and Osteoporosis is Similar by Traditional Chinese Medicine. Curr Pharm Des. 2015; 22[3): 312-320.
- Zhang BY, Dong JH, Zhou ZY. Tou Teng. In: Zhong Yi Nei Ke. Shanghai: Shanghai Ke Xue Zhi Shu Chu Ban She; 1985; p. 198–203.
- Böwing G, Zhou J, Endres HG, Coeytaux RR, Diener HC, Molsberger AF. Differences in Chinese diagnoses for migraine and tension-type headache: An analysis of the German acupuncture trials [GERAC) for headache. Cephalalgia. 2010; 30[2): 224-232.
- Wu NL, Wu AQ. The Function of the Five Viscera to the Human Body and Their Mutual Relations. In: Yellow Empero’s Canon Internal medicine. beijing: Zhong Guo Ke Xue Zhi Shu Chu Ban She; 1997; p. 64-68.
- ItsHaky B. Huang Di Nei Jing Ling Shu; The Ancient Classic on Needle Therapy; The Complete Chinese Text with an Annotated English Translation. Altern Complement Integr Med. 2017; 3[1): 1–11.
- Wang GJ, Ayati MH, Zhang WB. Meridian Studies in China: A Systematic Review. JAMS Journal of Acupuncture and Meridian Studies. Korean Pharmacopuncture Institute, 2010; 3: p. 1–9.
- Chang S. The meridian system and mechanism of acupuncture-A comparative review. Part 1: The meridian system. Taiwanese Journal of Obstetrics and Gynecology. Elsevier; 2012; 51: p. 506-514.
- Edvinsson JCA, Viganò A, Alekseeva A, Alieva E, Arruda R, De Luca C, et al. The fifth cranial nerve in headaches. Vol. 21, Journal of Headache and Pain. BioMed Central; 2020; p. 1–17.
- Zhu Y, Zhang H, Liu L, Liu Y, Zhang F, Bai J, et al. Yin-Coldor Yang-HeatSyndrome Type of Traditional Chinese Medicine Was Associated with the Epidermal Growth Factor Receptor Gene Status in Non-Small Cell Lung Cancer Patients: Confirmation of a TCM Concept. Evid Based Complement Alternat Med. 2017; 2017: 1–7.
- Zhongjing Z. Treatise on Febrile Diseases. 1st ed. Beijing: People’s Health Publishing House; 2019; p. 26–99.
- Pradhan SK. Komplementärmedizinische Behandlung von Kopfschmerz am Beispiel der Akupunktur. Psychiatr Neurol Rosenfluh, 2020; 3: 42–43.
- Schiapparelli P, Allais G, Rolando S, Airola G, Borgogno P, Terzi MG, et al. Acupuncture in primary headache treatment. In: Neurological Sciences. Neurol Sci; 2011.
- Zhang HL. Treatment of depression based on differentiation of the shaoyang channels. J Tradit Chin Med. 2010; 30[2): 83–92.
- Liao W, Dang C, Pan W. The Brief Theory of Viscus and Its Manifestations in Traditional Chinese Medicine. Integr Med Int. 2017; 4[1–2): 13–18.
- Zhang L, Zhang QM, Wang YG, Yu DL, Zhang W. The TCM pattern of the six-zang and six-fu organs can be simplified into the pattern of five-zang and one-fu organs. J Tradit Chin Med, 2011; 31[2): 147-151.
- O’Brien KA. Alternative perspectives: How chinese medicine understands hypercholesterolemia. Cholesterol, 2010; 2010.
- Wang W, Liu X, Liao X, Tan Q, Li M, Liu J, et al. Conceptual framework of modern Zangxiang concept: a qualitative content analysis. J Tradit Chin Med Sci, 2018; 5[1): 43– 52.
- Zhao L, Wang T, Dong J, Chen A, Li G. Liver-stomach disharmony pattern: theoretical basis, identification and treatment. J Tradit Chin Med Sci, 2018; 5[1): 53–57.
- Payant M-J. A Single Case Study: treating Migraine Headache with Acupuncture, Chinese Herbs, and diet. Glob Adv Health Med, 2014; 3[1): 71-74.
- Wang XQ, Zou XR, Zhang YC. From “kidneys Govern Bones” to Chronic Kidney Disease, Diabetes Mellitus, and Metabolic Bone Disorder: A Crosstalk between Traditional Chinese Medicine and Modern Science. Evidence-based Complementary and Alternative Medicine. Hindawi Limited, 2016; 2016.
- Wu X-N. Current concept of Spleen-Stomach theory and Spleen deficiency syndrome in TCM. World J Gastroenterol, 1998; 4[1): 2.
- Szmelskyj I, Aquilina L, Szmelskyj AO. Investigations from a TCM perspective. In: Acupuncture for IVF and Assisted Reproduction. Elsevier, 2015; p. 97-142.
- Yang YF, Ross J. Syndrome of disharmony and formula composition. In: Chinese Herbal Formulas. Churchill Livingstone, 2010; p. 361-381.
- Dashtdar M, Dashtdar MR, Dashtdar B, Kardi K, Shirazi MK. The concept of wind in traditional chinese medicine. J Pharmacopuncture, 2016; 19[4): 293-302.
- Sun GR, Tong Y, Chen WK. Liu Yin. In: Zhong Yi Ji Chu Lun. Beijing: Zhong Guo Zhong Yi Yao Chu Ban She, 2002; p. 218-223.
- Wang Y, Huang Y, Xie JH. Classification and Characteristics of Internal Diseases in Traditional Chinese Medicine. In: Internal Medicine of Traditional Chinese Medicine. Shanghai: Publish House of Shanghai University of Traditional Chinese Medicine, 2002; p. 1–5.
- Fu CH, Zou YH. Theoretical analysis and clinical application of migraine from the treatment of liver wind and blood stasis. Tianjin Traditional Chinese Medicine, 2016; 33[11): 698–701.
- NJUTCM. Interpretation of The Inner Canon of the Yellow Emperor. 4th ed. Shanghai: Shanghai Scientific and Technical Publishers, 2009; p. 281
- Shen HQ. Clinical diagnosis and treatment of headache. Jiangxi Traditional Chinese Medicine, 1995; 2: 47-48.
- Riley D. Wind-Heat Headache. In: Treating pain with traditional Chinese medicine. Paradigm Publications, 2003; p. 23.
- Tan T, Wang JG, Sun Q, Shi YS. The Qi-regulating massotherapy for treatment of tonic headache in 150 cases. J Tradit Chin Med, 2009; 29[1): 13–18.
- Sun P. Head and Neck Pain. In: The Treatment of Pain with Chinese Herbs and Acupuncture E-Book. Elsevier Health Sciences, 2010. p. 79–102.
- Wu Y, Fisher W. Practical therapeutics of traditional Chinese medicine. In: Fratkin J, editor. Headache. Brookline, MA: Paradigm Publications, 1997; p. 162-194.
- Wang J, Xiong X. Control strategy on hypertension in Chinese medicine. Vol. 2012, Evidence-based Complementary and Alternative Medicine, 2012.
- Rong H, Li Z, Yanhong Z, Yang X. Professor Li Zhenhua’s experience in treating blood stasis and headache. Chin J Tradit Chin Med, 2006; 2006: 1212.
- Headache disorders, 2021.
- Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol, 2018; 17[11): 954-976.
- Stovner LJ, Hagen K. Prevalence, burden, and cost of headache disorders. Current Opinion in Neurology. Curr Opin Neurol; 2006; 19: p. 281-285.
- Fumal A, Schoenen J. Tension-type headache: current research and clinical management. The Lancet Neurology. Elsevier; 2008; 7: p. 70–83.
- Jensen RH. Tension-Type Headache – The Normal and Most Prevalent Headache. Headache. 2018; 58[2): 339-345.
- Radtke A, Neuhauser H. Prevalence and burden of headache and migraine in Germany. Headache, 2009; 49[1): 79-89.
- Yao C, Wang Y, Wang L, Liu Y, Liu J, Qi J, et al. Burden of headache disorders in China, 1990-2017: Findings from the Global Burden of Disease Study 2017. J Headache Pain, 2019; 20[1): 102.
- Rizzoli P, Mullally WJ. Headache. Vol. 131, American Journal of Medicine. Elsevier Inc, 2018; p. 17–24.
- Morgan M, Jenkins L, Ridsdale L. Patient pressure for referral for headache: A qualitative study of GP’s referral behaviour. Br J Gen Pract, 2007; 57[534): 29-35.
- Roesch A, Dahlem MA, Neeb L, Kurth T. Validation of an algorithm for automated classification of migraine and tension-type headache attacks in an electronic headache diary. J Headache Pain, 2020; 21[1): 75.
- Ziegeler C, Brauns G, Jürgens TP, May A. Shortcomings and missed potentials in the management of migraine patients - Experiences from a specialized tertiary care center. J Headache Pain, 2019; 20[1): 86.
- Li X, Li X, Liu Q, Sun N, Zhang B, Shi C, et al. Traditional Chinese medicine combined with western medicine for the treatment of secondary pulmonary tuberculosis. Medicine [Baltimore), 2020; 99[16): e19567.
- Ni L, Chen L, Huang X, Han C, Xu J, Zhang H, et al. Combating COVID-19 with integrated traditional Chinese and Western medicine in China [Internet]. Acta Pharmaceutica Sinica B. Chinese Academy of Medical Sciences, 2020; 10: p. 1149–1162.
- Schiller J, Karst M, Kellner T, Zheng W, Niederer D, Vogt L, et al. Combination of acupuncture and medical training therapy on tension type headache: Results of a randomised controlled pilot study. Cephalalgia. 2021; 41[8): 879-893.
- Wang Y, Shi Y, Zhang X, Zou J, Liang Y, Tai J, et al. A Chinese Prescription Chuanxiong Chatiao San for Migraine: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Vol. 2019, Evidence-based Complementary and Alternative Medicine. Hindawi Limited, 2019; 15-18.
- National Administration of Traditional Chinese Medicine professional Technical Qualification Examination Expert Committee. Internal Medicine of TCM. Beijing: China Press of Traditional Chinese Medicine; 2019; p. 861–863.

