Effect of Dental Composite Increment Thickness on Hardening of Bulk-fil Resin Composite Restorative
Mohamed Omoush, Omar El-Mowafy*, Dave Kojic
Faculty of Dentistry, University of Toronto, Canada
Received Date: 15/09/2021; Published Date: 12/10/2021
*Corresponding author: Omar El-Mowafy, BDS, PhD, FADM, Professor, Faculty of Dentistry, University of Toronto, 124 Edward Street, Toronto, Ontario M5G 1G6
Abstract
The aim of this study was to determine Relative Hardness (RH) of a restorative bulk-fil composite when polymerized in increments with two LED lights. Methods: Two resin composites were used, Tetric-Evoceram Bulk-fill and Tetric -Evo Ceram nano-hybrid Universal (Ivoclar-Vivadent). Specimens were prepared from shade A2 in 4 thicknesses (1 – 4 mm). Two LED light polymerization units were used, Elipartm Deep-cure, 3M/ESPE and Blue phase Style, Ivoclar-Vivadent. Specimens were polymerized from upper surface only for 10 and 20 sec. Knoop microhardness measurements were then made on both upper and lower surfaces of each specimen. Ten Knoop hardness numbers (KHN) were obtained per specimen, five upper and five lowers. RH ratios were calculated by dividing a lower KHN by the corresponding upper value. Five RH ratios were obtained from each specimen (n = 5). Data were statistically-analyzed with multi-variate ANOVA. Results: ANOVA revealed significant differences among the groups (p<.0001). In general, 20 sec polymerization-cycle resulted in higher RH ratios than the 10 sec one. RH ratios decreased as specimen thickness increased. For Tetric-Evoceram Bulk-fil, RH ratio fell below the desired 80% level once increment thickness was greater than 2 mm irrespective of light unit used. For Tetric-Evoceram Nano-hybrid, RH ratio fell below the desired 80% level once increment thickness was greater than 1 mm irrespective of light unit used. No significant difference was found between the two light units in terms of mean RH ratios (P = .247). Conclusions: While RH ratios were generally higher for Tetric Evo Ceram Bulk-fil, indicating a better monomer conversion, however, when specimen thickness was greater than 2 mm, RH ratios fell significantly below the desired 80% level. This finding is alarming as it directly relates to the risk of incomplete hardening that can be encountered in the Class 2 restorations. Thinner increments should be always used irrespective of the type of the composite restorative along with longer polymerization cycle of at least 20 seconds to ensure optimum hardening.
Introduction
Globally, the use of bonded composite restorations continues to increase on the expense of traditional amalgam restorations. [1] In the last few years, the widespread use of light sources has given rise to manufacturers producing several varieties of light units with variable intensities. Several factors can affect the intensity of a light unit such as line voltage [2], condition of the bulb and filters [3], resin adherence to the curing tip end, fracture of optic fiber bundles inside the light guide [4] and, more importantly, the type of the light unit (LED, Plasma-arc, Halogen and laser). LED light units have become the most popular and are used widely by dentists in North America
A polymerization light with proper wavelength range must reach all areas of a light-activated restoration to ensure adequate polymerization and long-term clinical success. The depth of polymerization of composite restorations is affected by several factors, one of which is light energy [5,6]. Manufacturers have recently produced a number of radiometers useful for measuring the light intensity of the unit in the amount of energy on a given surface area (mW/cm2), in a limited wavelength range (400 to 520 nm). This is a way that clinicians can rely on to verify periodically the effectiveness of their dental polymerization lights [7,8].
Methods for evaluating the depth of polymerization of light-activated composites include optical microscopy to detect changes in the translucency of the polymerized section [9], scraping a specimen to remove unpolymerized portion and determine the depth of polymerization [10], infrared spectroscopy [11] and determining the relative hardness (RH) of the lower and upper surfaces of polymerized specimens [12,13].
Factors that may contribute to the quality of polymerization of composite restorations include light intensity [14-17] exposure time [14,16,18-21], light wavelength [22], thickness of the composite increment [20], distance between the tip of the light guide and the surface of the composite [23], shade of the composite [24] and composition of the composite material [12,21,23,25,26].
Depth of polymerization and microhardness testing have been widely used to assess the relative hardness of resins and, thus, the efficiency of light sources [27,28]. Surface microhardness is related to the degree of monomer conversion and resin composites showed a gradual decrease of microhardness from the top surface toward the bottom of specimens polymerized from the top surface only [29]. Since microhardness measurement has been deemed a useful method to indirectly probe degree of conversion of the polymer matrix [30], the gradual decrease in microhardness along the specimen’s thickness suggests a decrease in the degree of monomer conversion with decreasing light penetration and increasing distance from the irradiated surface [30].
Four types of polymerization sources have been developed: quartz tungsten halogen (QTH) lamps, light emitting diodes (LED) units, plasma-arc lamps and argon-ion lasers [31,32].
Halogen light emits light intensities ranging from 400–800 mW/cm2 [33], however, despite its low cost, halogen lights have some limitations, such as gradual reduction in energy output over time, limited depth of cure and relatively longer exposure time [33,34]. It is expected that, if the light intensity is increased, the degree of polymerization improves, the polymerization depth increases and a shorter irradiation time is possible [35,36].
The use of light-emitting diodes [LED] units have certain advantages over conventional light units: Many of them are wireless, and the LEDs have an estimated lifetime of about 10,000 hours, in contrast, QTH bulbs have a lifetime of 50 to 100 hours.[28,37,39]
If a resin composite restoration does not receive sufficient light exposure at the correct wavelength, the degree of polymerization may be less than ideal [14,40,41]. Previous studies have reported that QTH lights should deliver a minimum irradiance [power density] of 300 to 400 mW/cm2 to adequately cure a 1.5- to 2.0-mm increment of resin composite [14,15,42]. Although many lights can produce much more than 400 mW/cm2, the spectral emission from some of these lights may not match the absorption characteristics of the photosensitizers used in the resin composites, which then fail to polymerize adequately despite receiving sufficient total light energy [28,39,43-50].
More than 37% of composite restorations are clinically insufficiently polymerized, and most of the time it is due to inefficient light units with intensities of less than 300 mW/cm2, which are described in the literature as inadequate, unusable, or unsuitable [28]..Three international studies conducted to measure the intensity of light units used for polymerization of resin composites in private dental offices reported that 33% to 48% of the lights had intensities of less than 300 mW/cm2 [51-53]..
The aim of this study was to determine relative hardness of a bulk-fil composite restorative when polymerized in increments of 1 mm thick with two polymerization cycles. A conventional micro-hybrid composite restorative served as a control. In addition, two high-intensity light polymerization units were compared in terms of their effect on hardening of the two composite restoratives.
Material and Method
Details of two light polymerization units used in this study are presented in table [1]. Two resin composite restoratives were used [Tetric evoceram nano-hybrid Universal Composite Restorative Resin [Figure 1] and Tetric Evoceram Bulk Fill, [Figure 2], Ivoclar Vivadent, Germany] with a shade of A2 for both materials. The manufacturers and detailed composition of the restorative resin composite materials are presented in Table 1, 2.
Thirty-two-disc specimens of the two composite resins were obtained. Prefabricated cylindrical metallic molds with a 3 mm internal diameter and thicknesses of 1 mm, 2 mm, 3 mm and 4 mm were used to make the specimens. Specimens were prepared by placing a mold on a glass slide lined with a Mylar strip, then the mold was filled up flush with the composite material before another glass section lined with a Mylar strip was placed on top of it. The glass sections were secured together with a clamp. Composite resin [shade A2, Tetric evoceram Universal the LED light was applied from the top surface only for either 10 or 20 seconds. Both Light unit intensities were measured before every light activation using the CheckMARC® System provided by BlueLight Analytics. The resultant polymerized composite specimen thickness was verified with a micrometer to ensure accuracy. Specimens were individually placed in black vials in water and were stored in the dark for 48 hours at 37±1°C.
After storage, each specimen was submitted to a micro-hardness test [Tukon 300; Acco Industries Inc., Wilson Instrument Division, Bridgeport, Conn.]. A Knoop indenter was used for making the indentations. Micro-hardness measurements were made on the light-exposed surface [top surface] and on the bottom surface for all specimens. Five indentations were made on each specimen surface [top and bottom] under a static load of 50 g for 30 s [Figure 3]. Relative Hardness [RH] was calculated as a ratio between Knoop hardness number of the lower surface over that of the upper. Five RH ratios were obtained per specimen [n = 5]. Data were analyzed by four-way univariate ANOVA with 95% confidence level. Data analyses were performed using SPSS version [22].
Table 1: Characteristics of LED light polymerization units used.

Table 2: Composition of composite material used.
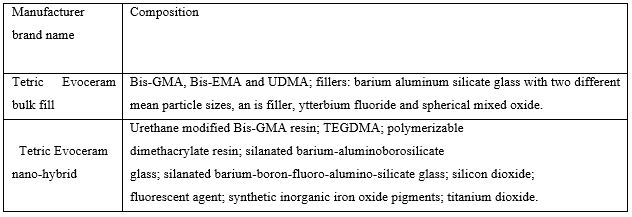

Figure 1: Syringe containing Tetric Evoceram resin composite restorative.

Figure 2: Syringe containing Tetric Evoceram Bulk Fill resin composite restorative.
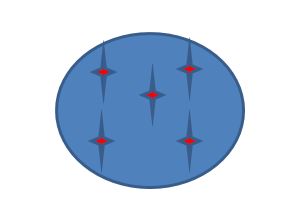
Figure 3: Diagrammatic representation of a composite specimen surface with locations of 5 indentations made with the Knoop indenter, one at the center and one at each corner.
Results
Mean RH ratios decreased with increasing thickness of the material increment regardless of the light unit used, polymerization cycle or type of composite. In general, RH ratio was higher for the Tetric Bulk-Fill compared to the Tetric Evo Ceram. Mean [SD] RH ratios for all groups are given in [Table 3].
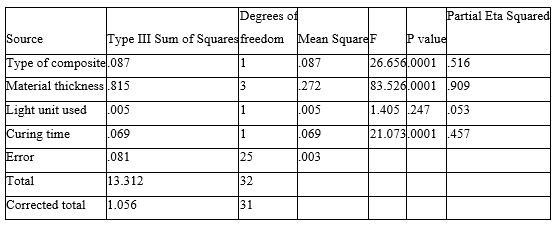
Four-way univariate ANOVA showed that all variables, with the exception of the type of light unit, to have a statistically significant effect on RH ratios [p<.0001]. RH ratio increased with increasing polymerization cycle and decreased with increasing increment thickness. Changing the type of light unit did not have any statistically significant effect on RH ratio [P = .247] [Table 4].
Table 3: Mean relative hardness ratios and standard deviation values for both composite restoratives with the two light units at the two polymerization cycles and the four specimen thicknesses.

Table 4: Statistical analyses ANOVA results for all variables.
Discussion
Relative hardness measurements are simple, reproducible and reliable information that provide a good indication of the quality of monomer conversion within a resin composite restorative increment. An 80% relative hardness ratio was established as an arbitrary ratio that is universally accepted as a cut off point for optimum polymerization of resin composite. A relative hardness ratio greater than 80% for a 2 mm resin composite increment indicates adequate monomer conversion with subsequent optimum polymerization. In contrast, a relative hardness ratio less than 80% for a 2 mm thick increment of composite resin indicates less than ideal monomer conversion. As seen in Table 3, in general, the reported relative hardness ratios ranged from 37% to 93% which is a fairly wide range. Perhaps there is need to create an arbitrary buffer zone where relative hardness ratios that are less than 80% but greater than 60% are considered acceptable, however, not optimum. While relative hardness ratios less than 60% would be considered clinically unacceptable.
Statistical analyses of the results of the present study showed that for the two composite materials, the relative hardness ratios were not significantly different between the 1mm and 2mm increment thickness with either LED lights used. For the two materials, when the 1 mm composite increment thickness was tested, the relative hardness ratios ranged from 74% to 94% indicating acceptable monomer conversion. However, when the composite increment thickness increased to 2 mm, the relative hardness ratios ranged from 58% to 80%. While these ratios fell below the optimum level, they were well within the “acceptable range”.
For the 3 mm thick composite increment, relative hardness ratios ranged from 35% to 61% for both composites and with both LED lights. While for the 4 mm thick composite increment, the range dropped to 34% to 57%. This means that for both increment thicknesses, relative hardness ratios fell below the acceptable level and, indeed, were far from the optimum level. Based on this, for both materials tested, dentists must ensure that the maximum thickness used in a composite restoration must not exceed 2 mm. This is in order to ensure acceptable monomer conversion with subsequent adequate hardness.
The bulk fill resin composite had better overall higher relative hardness ratios particularly at the deeper levels [3 and 4 mm]. This might be due to compositional differences in the inorganic fillers incorporated, their loading and distribution. Bulk-fil composites have a lower inorganic filler loading which may contribute to less light scatter and deeper penetration of the LED light within the composite increment. This speculation is based on the premise that more inorganic fillers will impede light penetration with limited amounts of light energy reaching the deeper levels of the composite increment.
Both LED units used in this study provided the minimum energy output required for adequate polymerization of resin composites and both performed well. However, only two representative composite materials were tested in the present study which is a limitation. More studies are needed where a larger number of bulkfil composites is included.
The results of the present study indicated that increasing the composite increment thickness beyond 2 mm adversely affected the degree of polymerization due to limited light penetration with subsequent less than ideal relative hardness ratios. This is in agreement with findings reported in a study by Price et al who found that with increasing specimens’ thickness, there was exponential decrease in light energy transmitted for seven different resin composites tested using 2 different light intensities [26]. However, Flury et al found that increasing the thickness of resin composite materials will lead to a decrease in the microhardness of conventional resin composites but not the bulk fill resin composites [27]. There could be some material specific variables that led to their contrasting findings.
Conclusions
Based on the findings of this work, it is concluded that:
[1] The resin composite type, increment thickness and polymerization cycle were all factors that influence the relative hardness ratios.
[2] Two different light polymerization units performed equally with respect to relative hardness ratios of the two composites tested.
[3] Increasing light exposure time from 10s to 20s resulted in statistically higher relative hardness ratios regardless of the composite increment thickness.
[4] Clinician should consider increasing polymerization cycle to 20 seconds and using thin composite increments regardless of the type of material used in order to optimize hardening.
[5] Relative hardness ratios of the bulkfil material tested fell below the accepted range once the material increment thickness increased to 3 and 4 mm.
References
- Eklund SA. Trends in dental treatment, 1992 to 2007. Journal of the American Dental Association (1939). 2010; 141(4): 391-399.
- Fan PL, Wozniak WT, Reyes WD, Stanford JW. Irradiance of visible light-curing units and voltage variation effects. Journal of the American Dental Association (1939). 1987; 115(3): 442-445.
- Watts DC, Amer O, Combe EC. Characteristics of visible-light-activated composite systems. British dental journal. 1984; 156(6): 209-215.
- Pollack BF, Lewis AL. Visible light resin-curing generators: a comparison. General dentistry. 1981; 29(6): 488-493.
- Visible light-cured composites and activating units. The Journal of the American Dental Association.110(1):100-103.
- Pires JA, Cvitko E, Denehy GE, Swift EJ Jr. Effects of curing tip distance on light intensity and composite resin microhardness. Quintessence international (Berlin, Germany: 1985). 1993; 24(7): 517-521.
- Fowler CS, Swartz ML, Moore BK. Efficacy testing of visible-light-curing units. Operative dentistry. 1994; 19(2): 47-52.
- Lee SY, Chiu CH, Boghosian A, Greener EH. Radiometric and spectroradiometric comparison of power outputs of five visible light-curing units. Journal of dentistry. 1993; 21(6): 373-377.
- Newman SM, Murray GA, Yates JL. Visible lights and visible light-activated composite resins. The Journal of prosthetic dentistry. 1983; 50(1): 31-35.
- Cook WD. Factors affecting the depth of cure of UV-polymerized composites. Journal of dental research. 1980;59(5):800-808.
- DeWald JP, Ferracane JL. A comparison of four modes of evaluating depth of cure of light-activated composites. Journal of dental research. 1987; 66(3): 727-730.
- Johnston WM, Leung RL, Fan PL. A mathematical model for post-irradiation hardening of photoactivated composite resins. Dental materials: official publication of the Academy of Dental Materials. 1985;1(5):191-4.
- Tirtha R, Fan PL, Dennison JB, Powers JM. In vitro depth of cure of photo-activated composites. Journal of dental research. 1982; 61(10): 1184-1187.
- Rueggeberg FA, Caughman WF, Curtis JW Jr. Effect of light intensity and exposure duration on cure of resin composite. Operative dentistry. 1994; 19(1): 26-32.
- Fan PL, Schumacher RM, Azzolin K, Geary R, Eichmiller FC. Curing-light intensity and depth of cure of resin-based composites tested according to international standards. Journal of the American Dental Association (1939). 2002; 133(4): 429-434; quiz 91-93.
- Santos GC Jr, El-Mowafy O, Rubo JH, Santos MJ. Hardening of dual-cure resin cements and a resin composite restorative cured with QTH and LED curing units. Journal (Canadian Dental Association). 2004; 70(5): 323-328.
- Miyazaki M, Hattori T, Ichiishi Y, Kondo M, Onose H, Moore BK. Evaluation of curing units used in private dental offices. Operative dentistry. 1998; 23(2): 50-54.
- Dietschi D, Marret N, Krejci I. Comparative efficiency of plasma and halogen light sources on composite micro-hardness in different curing conditions. Dental materials: official publication of the Academy of Dental Materials. 2003; 19(6): 493-500.
- Baharav H, Abraham D, Cardash HS, Helft M. Effect of exposure time on the depth of polymerization of a visible light-cured composite resin. Journal of oral rehabilitation. 1988; 15(2): 167-172.
- Yap AU. Effectiveness of polymerization in composite restoratives claiming bulk placement: impact of cavity depth and exposure time. Operative dentistry. 2000; 25(2): 113-120.
- Ruyter IE, Oysaed H. Conversion in different depths of ultraviolet and visible light activated composite materials. Acta odontologica Scandinavica. 1982; 40(3): 179-192.
- Price RB, Derand T, Sedarous M, Andreou P, Loney RW. Effect of distance on the power density from two light guides. Journal of esthetic dentistry. 2000; 12(6): 320-327.
- Ferracane JL, Aday P, Matsumoto H, Marker VA. Relationship between shade and depth of cure for light-activated dental composite resins. Dental materials: official publication of the Academy of Dental Materials. 1986; 2(2): 80-84.
- Taira M, Urabe H, Hirose T, Wakasa K, Yamaki M. Analysis of photo-initiators in visible-light-cured dental composite resins. Journal of dental research. 1988; 67(1): 24-28.
- Ferracane JL, Greener EH. The effect of resin formulation on the degree of conversion and mechanical properties of dental restorative resins. Journal of biomedical materials research. 1986; 20(1): 121-131.
- Pashley DH. Mechanisms of dentin sensitivity. Dental clinics of North America. 1990; 34(3): 449-473.
- Kurachi C, Tuboy AM, Magalhaes DV, Bagnato VS. Hardness evaluation of a dental composite polymerized with experimental LED-based devices. Dental materials: official publication of the Academy of Dental Materials. 2001; 17(4): 309-315.
- Dunn WJ, Bush AC. A comparison of polymerization by light-emitting diode and halogen-based light-curing units. Journal of the American Dental Association (1939). 2002; 133(3): 335-341.
- Flury S, Hayoz S, Peutzfeldt A, Husler J, Lussi A. Depth of cure of resin composites: is the ISO 4049 method suitable for bulk fill materials? Dental materials: official publication of the Academy of Dental Materials. 2012; 28(5): 521-528.
- Flury S, Peutzfeldt A, Lussi A. Influence of increment thickness on microhardness and dentin bond strength of bulk fill resin composites. Dental materials: official publication of the Academy of Dental Materials. 2014; 30(10): 1104-1112.
- Hervas-Garcia A, Martinez-Lozano MA, Cabanes-Vila J, Barjau-Escribano A, Fos-Galve P. Composite resins. A review of the materials and clinical indications. Medicina oral, patologia oral y cirugia bucal. 2006; 11(2): E215-E220.
- Vandewalle KS, Roberts HW, Tiba A, Charlton DG. Thermal emission and curing efficiency of LED and halogen curing lights. Operative dentistry. 2005; 30(2): 257-264.
- Rahiotis C, Kakaboura A, Loukidis M, Vougiouklakis G. Curing efficiency of various types of light-curing units. European journal of oral sciences. 2004; 112(1): 89-94.
- Nomoto R, Uchida K, Hirasawa T. Effect of light intensity on polymerization of light-cured composite resins. Dental materials journal. 1994; 13(2): 198-205.
- Powell GL, Blankenau RJ. Laser curing of dental materials. Dental clinics of North America. 2000; 44(4): 923-930.
- Kelsey WP, 3rd, Blankenau RJ, Powell GL, Barkmeier WW, Cavel WT, Whisenant BK. Enhancement of physical properties of resin restorative materials by laser polymerization. Lasers in surgery and medicine. 1989; 9(6): 623-627.
- Mills RW, Jandt KD, Ashworth SH. Dental composite depth of cure with halogen and blue light emitting diode technology. British dental journal. 1999; 186(8): 388-391.
- Craford MG, Jr NH, Jr FAK. In pursuit of the ultimate lamp. Scientific American. 2001; 284(2): 63-70.
- Uhl A, Mills RW, Vowles RW, Jandt KD. Knoop hardness depth profiles and compressive strength of selected dental composites polymerized with halogen and LED light curing technologies. Journal of biomedical materials research. 2002; 63(6): 729-738.
- Peutzfeldt A, Sahafi A, Asmussen E. Characterization of resin composites polymerized with plasma arc curing units. Dental materials: official publication of the Academy of Dental Materials. 2000;16(5):330-6.
- Nomoto R. Effect of light wavelength on polymerization of light-cured resins. Dental materials journal. 1997; 16(1): 60-73.
- Shortall AC, Harrington E. Effect of light intensity on polymerisation of three composite resins. The European journal of prosthodontics and restorative dentistry. 1996; 4(2): 71-76.
- Mills RW, Uhl A, Jandt KD. Optical power outputs, spectra and dental composite depths of cure, obtained with blue light emitting diode (LED) and halogen light curing units (LCUs). British dental journal. 2002; 193(8): 459-463; discussion 5.
- Uhl A, Mills RW, Jandt KD. Photoinitiator dependent composite depth of cure and Knoop hardness with halogen and LED light curing units. Biomaterials. 2003; 24(10): 1787-1795.
- Soh MS, Yap AU, Siow KS. Effectiveness of composite cure associated with different curing modes of LED lights. Operative dentistry. 2003; 28(4): 371-377.
- Price RB, Ehrnford L, Andreou P, Felix CA. Comparison of quartz-tungsten-halogen, light-emitting diode, and plasma arc curing lights. The journal of adhesive dentistry. 2003; 5(3): 193-207.
- Jandt KD, Mills RW, Blackwell GB, Ashworth SH. Depth of cure and compressive strength of dental composites cured with blue light emitting diodes (LEDs). Dental materials: official publication of the Academy of Dental Materials. 2000; 16(1): 41-47.
- Uhl A, Sigusch BW, Jandt KD. Second generation LEDs for the polymerization of oral biomaterials. Dental materials: official publication of the Academy of Dental Materials. 2004; 20(1): 80-87.
- Price RB, Felix CA, Andreou P. Evaluation of a second-generation LED curing light. Journal (Canadian Dental Association). 2003; 69(10): 666.
- Sharkey S, Ray N, Burke F, Ziada H, Hannigan A. Surface hardness of light-activated resin composites cured by two different visible-light sources: an in vitro study. Quintessence international (Berlin, Germany: 1985). 2001; 32(5): 401-405.
- El-Mowafy O, El-Badrawy W, Lewis DW, Shokati B, Kermalli J, Soliman O, et al. Intensity of quartz-tungsten-halogen light-curing units used in private practice in Toronto. Journal of the American Dental Association (1939). 2005; 136(6): 766-773; quiz 806-807.
- Santos GC Jr, Santos MJ, El-Mowafy O, El-Badrawy W. Intensity of quartz-tungsten-halogen light polymerization units used in dental offices in Brazil. The International journal of prosthodontics. 2005; 18(5): 434-435.
- El-Mowafy O, El-Badrawy W, Lewis DW, Shokati B, Soliman O, Kermalli J, et al. Efficacy of halogen photopolymerization units in private dental offices in Toronto. Journal (Canadian Dental Association). 2005; 71(8): 587.

