Utilization of Soft Tissue and Bone Surface Scanning Algorithm, in Streamlining Diagnosis and Treatment Planning of Facial Asymmetry. Toward Advancing Protocol
Dastan Tahir Abdulla*, Suha Nafea Aloosi, Zaniar Mustafa Amin
KBMS Student in Oral and Maxillofacial Surgery, Lecturer University of Sulaimaniyah- College of Dentistry, Iraq
Received Date: 04/07/2021; Published Date: 30/07/2021
*Corresponding author: Dastan Tahir Abdulla, KBMS Student in Oral and Maxillofacial Surgery, Lecturer University of Sulaimaniyah- College of Dentistry, Iraq
Abstract
Introduction: Symmetry has always been a feature of facial attractiveness. Treating facial asymmetry and deformity are commonly encountered by maxillofacial surgeons. However, diagnosing and treatment planning is not an easy task and require experience and meticulous skills. Knowing the exact relationship between facial hard and soft tissue is mandatory for proper management and allows for developing a treatment plan that aims squarely at the patient complaint and avoid unnecessary procedures. In this study we aim to purpose a landmark independent algorithm for measuring facial asymmetries and clarify the relationship between facial hard and overlaying soft tissue in six different anatomical regions.
Material and Method: CT scan of fifty patients with primary facial asymmetrical feature were selected. And by using Radiant software, bone and soft tissue segmentations were performed on the scans. Exported Stereolithography (STL) files were cleaned and mirrored around the sagittal section using Meshmixer software applied by the author. The mirrored parts were overlayed on each other and aligned using ControlX software utilizing an automated landmark free algorithm to avoid human error and inter examiner disagreement. Finally using 3-matic software, the root mean square deviation (RMSD) value for each of the six anatomical facial units were recorded for hard and soft tissue parts. SPSS software was used to perform the statistical analysis.
Results: Statistically significant difference (p<0.05) between five of the six anatomical subunits were found. For the exception of the nasal area, all other regions showed marked difference between the degree of bony deformity and the amount of soft tissue deformity in the same area. Ranking from most to least difference were the mandibular ramus and periauricular region, mandibular body, Maxillary area, Chin, Zygomatic region and nasal area.
Conclusion: This research presents a reliable, reproducible and operator independent method for measuring facial Skelton and soft tissue deformities from patients CT scan as well as calculating the exact relationship between them. The effects of the underlying bony deformity on the overlying soft tissue and skin appearance are not consonant and change significantly based on the anatomical region. The thinner the soft tissue structure the more apparent are the effects of the hard tissue asymmetry. The results of this study will greatly aid maxillofacial surgeons in diagnosis and treatment plan formulations for cases with facial asymmetries and deformities. If the result is well understood and interoperated, can act as a guide for designing facial implants and determining their exact thickness to better estimate their soft tissue and final results.
Keywords: Asymmetry, RMSD, facial implants, orthognathic surgery.
Introduction
Facial asymmetry refers to the relationship of facial components around the sagittal axis [1]. Symmetry of the face has always been a fundamental feature for attractiveness and an essential goal for facial and esthetic plastic surgery. No face has an obsolete symmetry and a normal degree of asymmetry is always present but not commonly noticeable by casual observers. However, passing this normal limit the facial dysmorphism will become apparent [2].
Facial asymmetry may be apparent; however, precise diagnosis might not be a straightforward task. Unfortunately, it is commonly encountered that people with dento-facial asymmetry try to mask the deformity with postural changes that can deter even the most expert surgeon from the diagnosis [3,4]. For this reason and many others, facial asymmetry should be examined carefully and cautiously through multiple interviews and using the best diagnostic aid available [5].
Learning about the etiology behind developing asymmetry is crucial in developing a proper treatment planning, and ensuring acceptable long-term outcome. Asymmetry of the face can be classified based on etiology, time of onset and structural involvement, and according to Lundstrom the etiology behind the problem might be either genetic, non-genetic or combination of both [6]. Pirttiniemi however classifies facial asymmetry based on time of onset. The onset can be prenatal, embryonic and fetal, or can be post-natal [7]. Another classification based on the structures involved divides the facial asymmetry into dental, skeletal, muscular, functional or combination in origin [8].
A more used classifications for facial asymmetry are the morphological structural classifications. Obwegeser and Makek divide the problem into Hemi mandibular elongation and hemi mandibular hyperplasia type [9]. While, Kim et al., assessed the deviation of Menton point with the transverse asymmetry, canting of maxilla and lip [10]. Finally, Hwang et. al., analyzed skeletal asymmetry based on the chin and bilateral rami length difference [11].
The initial patient interview will act as a platform for hearing about the chief complaint and the patient’s expectation of the outcome of the treatment as well as establishing the causative factor for the asymmetry [12]. Clinical examination is to be performed in all directions and it is the fundamental diagnostic tool available to the surgeon. The face from frontal, lateral and vertical dimensions should be examined for assessing the complaint of the patient [13].
Treatment of facial asymmetry is challenging because of the complexity of the facial construct. The bony structure, soft tissue and dentition are all geometrically interconnected. For example, a simple asymmetry in the mandible usually associated with occlusal canting and maxillary overgrowth. This makes one jaw correction alone not useful for most deformities. Most of the time, treatment is complicated by the lack of comprehensive and accurate assessment and planning [14].
Asymmetry may involve a single jaw or a single bone, however due to the intricate relationship of the facial skeleton, the antagonist or related bone are usually affected as well and during growth and function, the related skeleton is influenced and decompensated. Bearing this in mind, the mandible is the most affected and maxillary bone is usually secondarily involved. All parts of the mandibular bone can be affected, the condyles, ramus, body and chin in asymmetry and the change can be in size, shape or location. Hence, correct diagnosis of the affected parts and the causative parts are of high importance [15].
Adopting conventional orthognathic surgeries in correcting facial asymmetry and more specifically medio-lateral deformity is unsatisfactory. The exact deficiency is going back to the restriction of lateral movement of the jaws in bi-maxillary surgery and the associated butterfly effect that has on the facial tissues as a whole that makes it to some extent unpredictable in some cases [16]. Facial implants and camouflage surgery provide an easier alternative and more predictable results in some cases, however, designing and choosing the correct implant thickness is the Achilles heel of the procedure as under and overestimation of the implant size are common [17]. In this paper we aim to rectify some of those shortcomings and provide an idea on the relationship between soft and hard tissue defects in different facial regions and their response to different implant sizes.
Conventional 2D analysis and conventional cephalometric studies are limited in diagnosing and planning because of their inherent limits when a 3D structure is projected onto a two-dimensional plane [18]. Conventional manual model surgery played an important part of preoperative preparation which comprise of multiple labor-intensive laboratory steps with every step carrying risk of errors and miscalculations. It is essential that when performing the model surgery, the patient data is transferred accurately. Failure in doing that will result in inaccurate wafers and guides that will lead to catastrophic outcomes even when a competent surgeon is involved [19].
Three-dimensional image gathering techniques including Cone Beam Computed Tomography (CBCT) and CT scans greatly improved that accuracy of recording the patient data as they are truly representative of the actual three-dimensional anatomy. The three-dimensional (3D) images can be manipulated and viewed from virtually any angle. Precise measurements can be taken and can greatly aid in understanding and diagnosing the etiology [20].
Another issue currently present is the estimation of the size of facial implants in relation of the soft tissue deficiency, as for now, predicting the exact size of implant needed for a specific deformity has been based only on the clinical judgment of the surgeon and mostly subjective [21]. Over and underestimation of implant sizes that leads to over and under correction is quite common with facial implants as currently used today. Through this study, we hope to provide an objective point of view for determining the correct implant site suitable for the facial anatomical region.
Through this study, we plan to develop a precise and landmark independent algorithm that can be used in diagnosis and treatment planning in cases with facial asymmetry. The proposed algorithm can be used on with soft tissue as well as hard tissue asymmetries and can distinguish the deformity in specific regions of the face, aiding in providing an objective tool in estimating facial implants size in relation to a specific region of the face and designing the final implant. Furthermore, we aim to propose our results to the established algorithms currently available.
Material and Method
Fifty patients had attended the Sulaymaniyah Surgical Teaching Hospital-Maxillofacial Surgery unit from January 2020 to March 2021 seeking facial correction surgeries. Patients were complaining of ranges of facial deformities and asymmetries. Adequate clinical examinations were done to ensure that the patients fit the inclusion criteria of the research which were as follow:
1- Patients with facial asymmetry.
2- Patients with facial deformity.
1- Deformities due to trauma.
2- Deformity due to pathological excision.
4- Patients orthodontically treated
1- Whole facial skeleton is included.
2- Acceptable quality without major artifacts from metal objects/dental restorations.
3- Jaws are centric occlusion while scanning.
From the 50 patients, 19 were male and 31 females. Their age was ranging from 18 to 42 years old.
CT Scans were taken with exposure conditions matched as closely as possible at 140kV and 120mA with 1mm slice thickness.
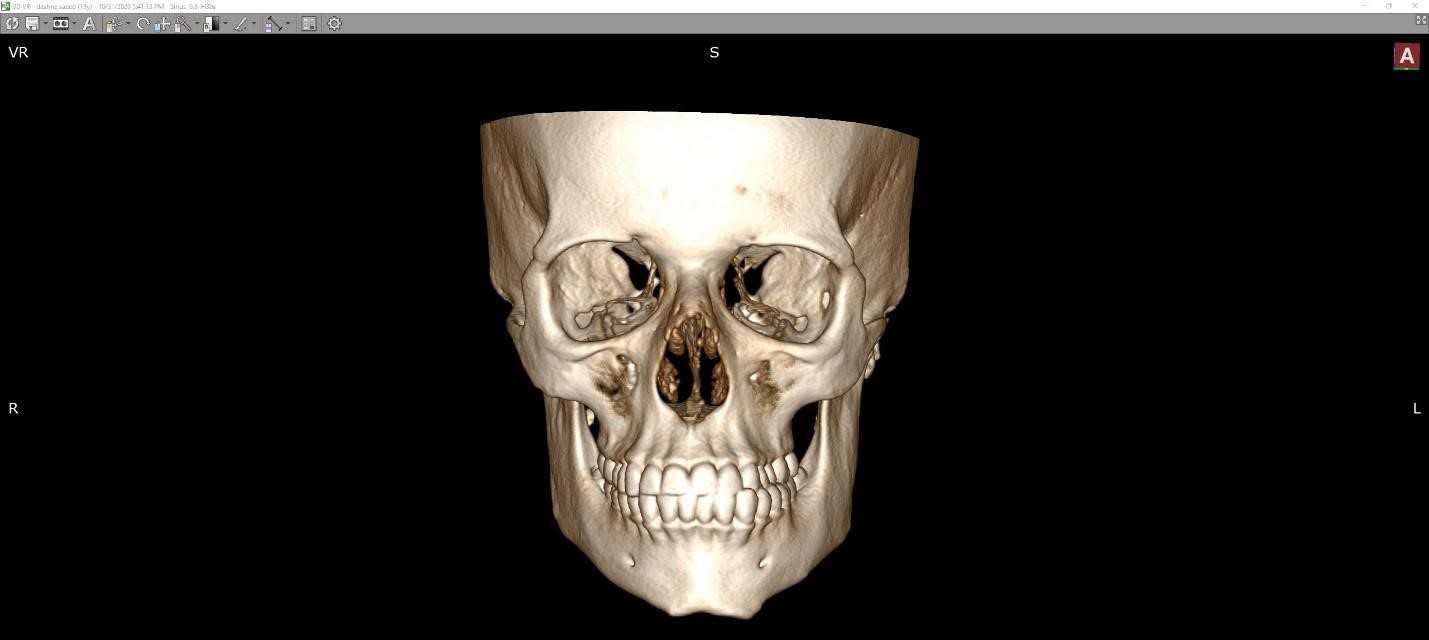
The scans were burned on a DVD disk in DICOM format, then the scan data were analyzed and 3D reconstructed using RadiAnt DICOM Viewer v. 2020.2.3 (Medixant, Poland) Figure 1.
For each patient, the scan data was segmented two times, once for obtaining the bone reconstruction and once to reconstruct the soft tissue surface Figure 2
This is a sample text. You can click on it to edit it inline or open the element options to access additional options for this element.
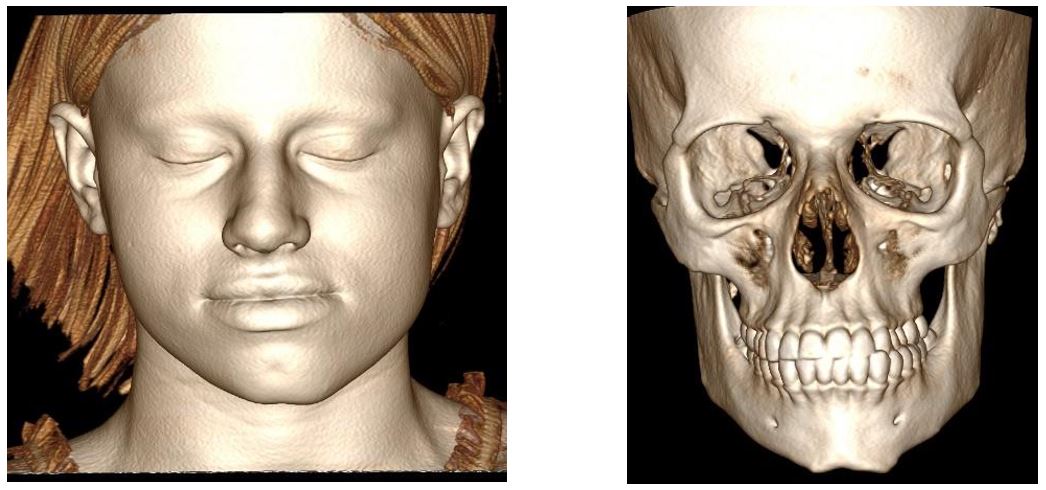
Figure 2: RadiAnt DICOM Viewer v. 2020.2.3 (Medixant, Poland) showing facial bones and soft tissue of a case in figure 1
The three-dimensional converted data was exported with the same software and saved as STL (Standard Triangle Language) files using the Hi-Res option. The stereolithographic files then were refined using Meshmixer v3.5 (Autodesk, Inc., USA). The refinements were encompassed fixing mesh holes, spikes and foreign body artifacts when present [22].
Using plane cut tool, a plane drawn parallel to the coronal plane 2mm behind the external auditory meatus and areas posterior to it were removed. The vertebral bones if present were also removed using the lasso select and delete tool. The remaining parts, facial bone and facial soft tissue parts were then mirrored parallel to the sagittal plane [23]. (Figure 3)
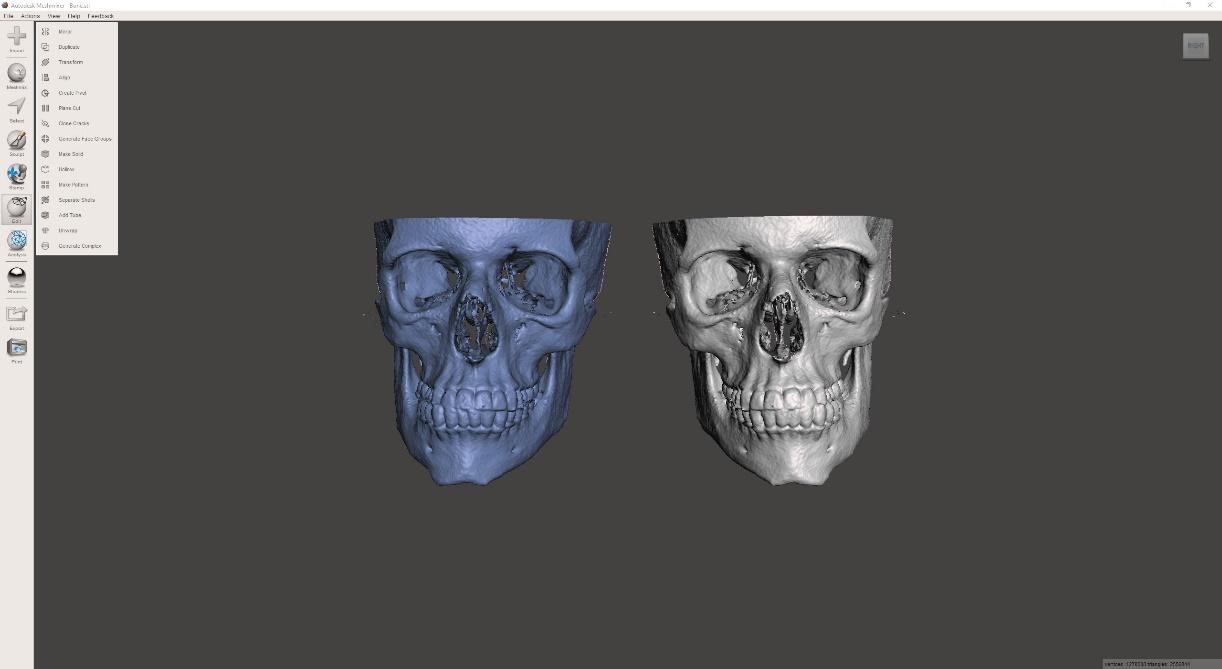
Figure 3: Meshmixer v3.5 (Autodesk, Inc., USA) mirroring of the facial skeleton of the patient in figure 1 and 2.
The newly created part and the original part then aligned using best fit alignment via Geomagic Control X v2018 1.1 (3D Systems Inc., USA). Landmark free alignment was performed ensuring operator-error free alignment that is a very serious limitation of conventional alignments techniques affecting reliability of the comparison results. Figure 4
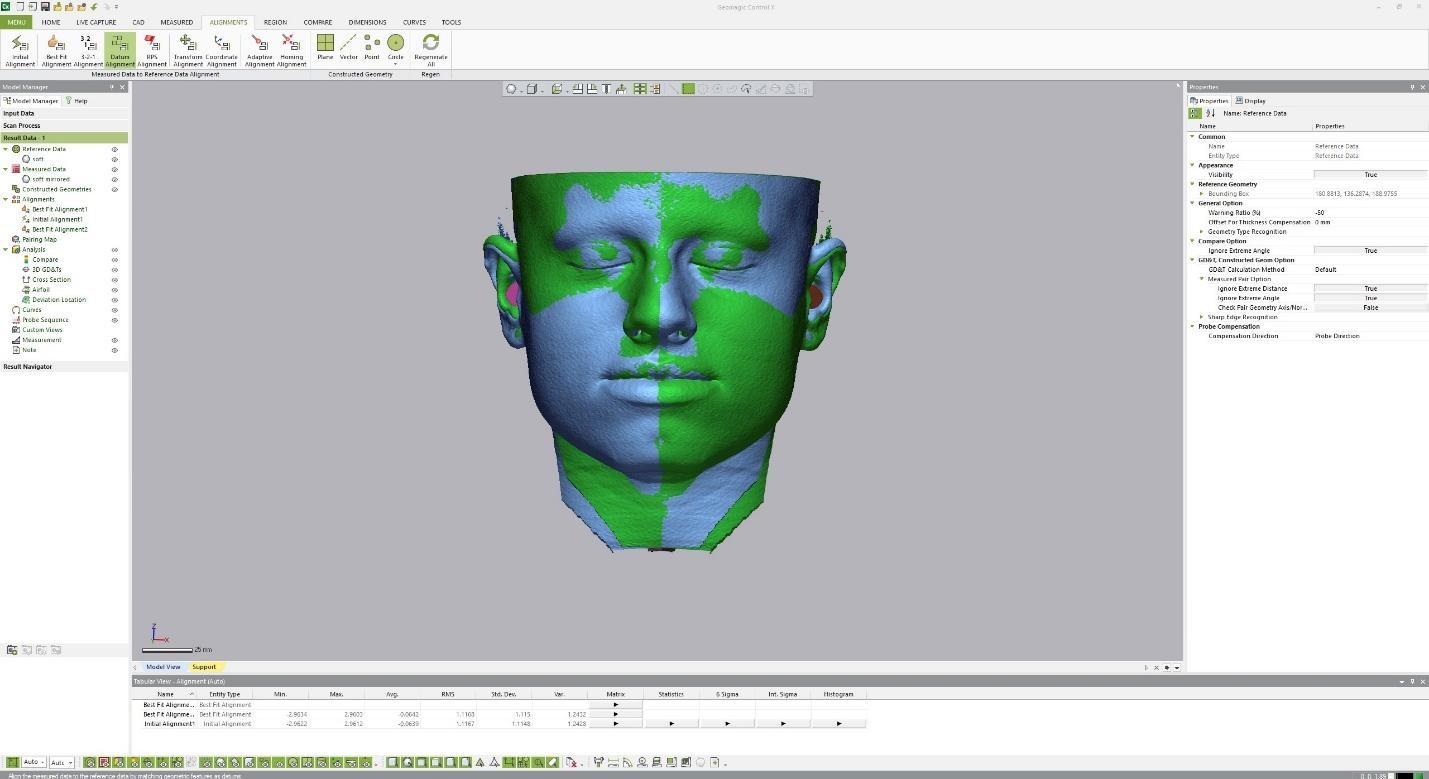
Figure 4: Geomagic Control X v2018 1.1 (3D Systems Inc., USA) Fully automated scan alignment. Showing the original and mirrored soft tissue aligned using best fit alignment tool.
Aligned data, both the original and the mirror parts, then exported to 3-Matics Medical v 13.0 (Materialize, USA). Figure 5
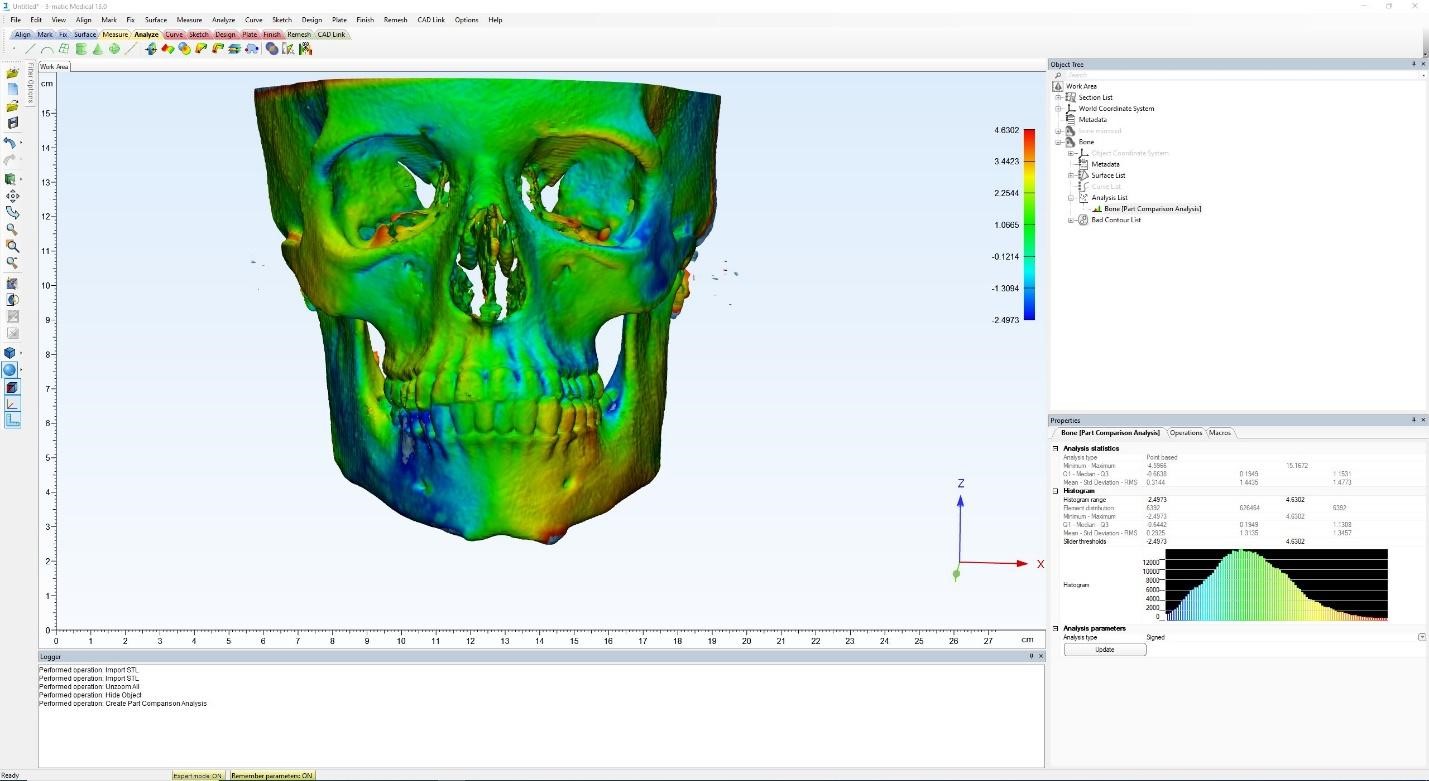
Figure 5: To 3-Matics Medical v 13.0 (Materialize, USA). Showing the heat-map of the amount of facial deformity comparing left to right side of the face. From blue to red according to the amount of deficiency to excess compared to the other side.
Different parts of the bony surface anatomy selected and compared separately based on the research points of interest as follows:
1- Zygomatic Bone.
2- Maxillary bone.
3- Nasal Bone.
3- Chin area between the two mental foramina.
4- Mandibular body, from mental foramen to the angle of mandible.
5- Mandibular ramus, from the mandibular angle to the sigmoid notch.
6- Mandibular condyle.
The Root Mean Square Deviation (RMSD) was calculated for each of the above areas. RMSD is a common numerical calculation to compare two solid structures by aligning them in a way that there is a minimal distance between each of their corresponding surface points. Advantage of this method is that it is algorithmically driven and lack human interference and therefore it is free of operator errors during alignment [24].
Different parts of the Soft tissue surface anatomy were selected and compared separately based on the research points of interest as follows
1- Malar Eminence
2- Nose
3- Chin
4- Buccal region of the mandible
5- Preauricular region (parotid area)
The Root Mean Square Deviation (RMSD) was calculated for each of the above areas, then RMSD for Soft tissue landmarks and bony landmarks were compared in the same anatomical subregion. Additionally, soft and hard tissue mean difference were also compared to further analyze the exact relationship between hard and soft tissue in each anatomic subunit using paired sampled T-Test.
Statistical Analysis
All statistical analyses were performed using the SPSS software package for Windows (version 25.0; SPSS, Chicago, Ill). Paired sample T-Test was performed as well as the standard descriptive statistics (mean and standard deviation). The statistical significance level was set at P <0.05.
Results
In this study, fifty patients were selected based on the predetermined criteria. RMSD values Extracted from soft tissue and bone scan for twelve different variables were measured as mentioned before. Six pairs of data were then selected for comparison based on the anatomical area. Each pair contained one soft tissue and one bony landmark for the same region.
The pairs created were named as follow:
1- Zygomatic Bone and Malar Soft.
2- Maxillary Bone and Upperlip Submalar area.
3- Nasal Bone and Nose Soft.
4- Mand Ramus Bone and Periauricular Soft
5- Chin Bone and Chin Soft.
6- Mand Body Bone and Man body Soft.
The mean RMSD value and Standard deviation are mentioned in table 1
Table 1: The mean RMSD, Std. Deviation and Std. Error.
Mean: The mean amount of deformity present measure by RMSD value.
N: Number of participants
St. Deviation: Deviation from mean value for each group.
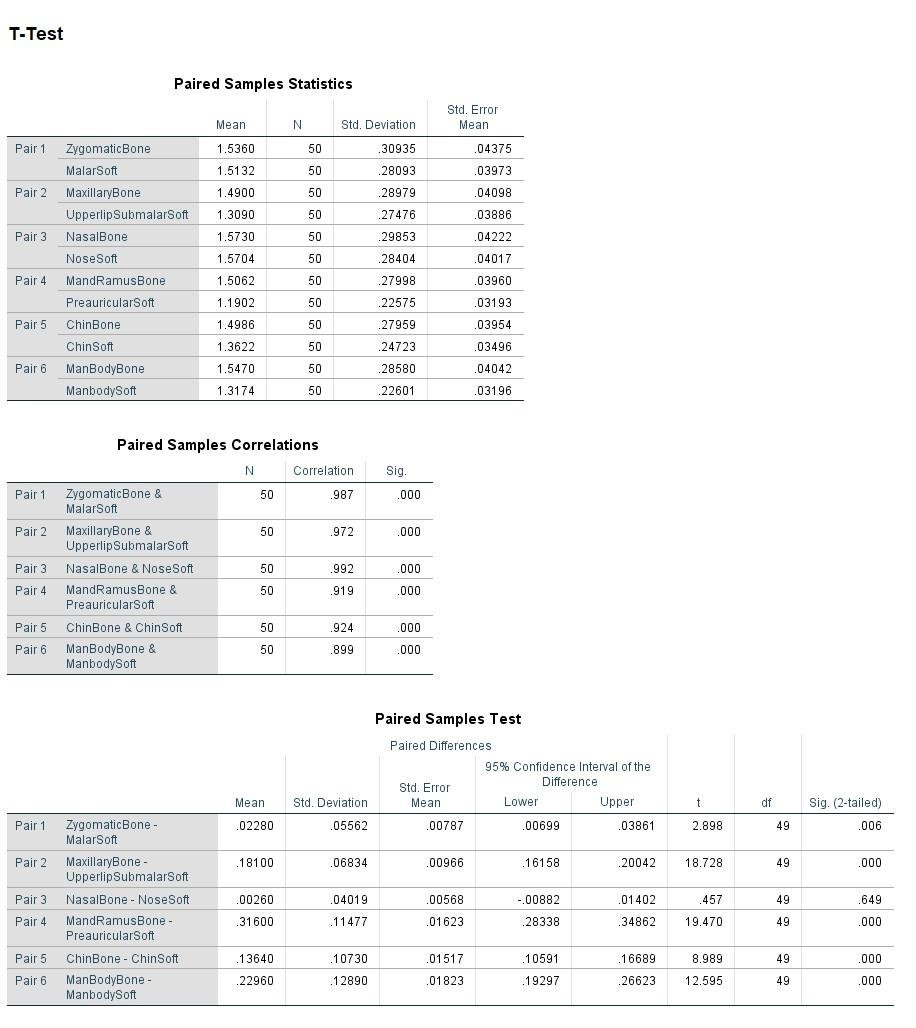
As it is shown in the Table 1, the mean RMSD values lies between 1.19 at the minimum to 1.57 at the maximum, which in accordance to the asymmetry ruler Figure 6 refers to significant asymmetry found in the participants.
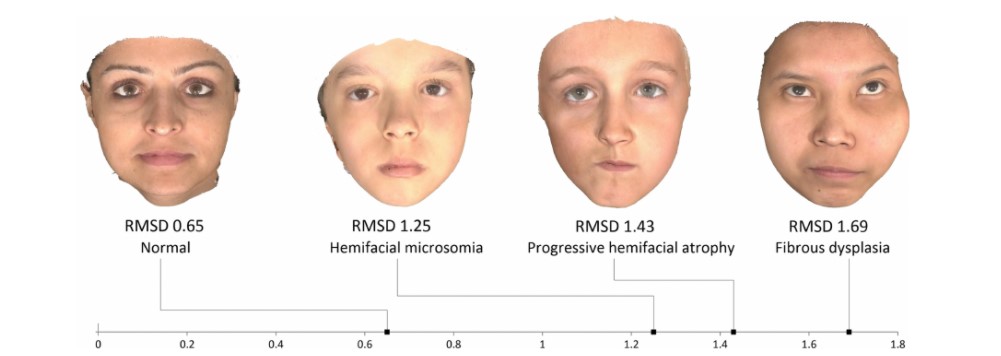
Figure 6 : RMSD ruler, measuring the asymmetry value from normal to deformed. Taylor et.al., 2014 [25]. A value of 0.65 deemed normal as exact symmetrical faces are not common.
Mandibular body bone, zygomatic bone and soft tissue, chin, the nasal bone and soft tissue. This is in line with the assumption that most of the facial deformities involve the mandible and the zygomatic area. Table 2
When comparing each pair, hard and soft tissue, there were a significant difference between the degree of the hard and soft tissue deformity in the same region except for the nasal area (Pair3).
Table 2 : Paired T-Test Comparison of bone and soft tissue landmarks. It should be a table not a figure !!
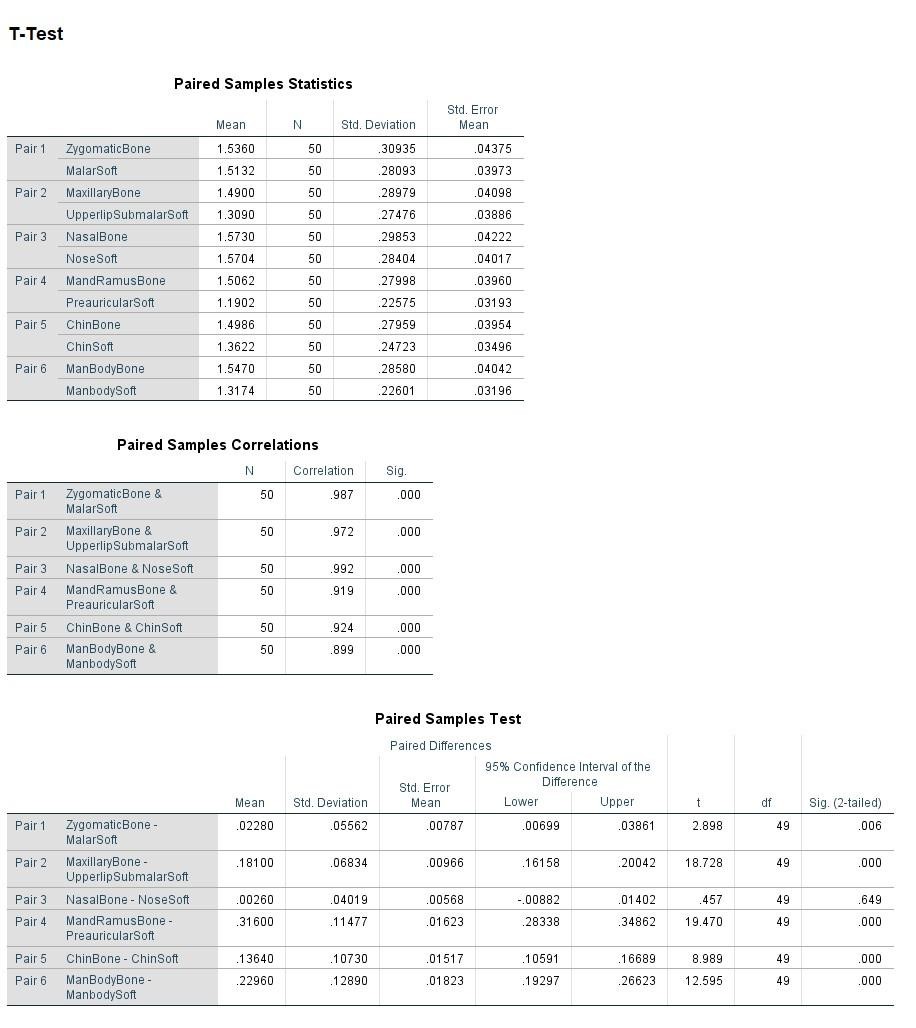
The results signify that in the selected region for this study except in pair 3, which resulted in p value of insignificant 0.649, there are considerable difference between the soft and hard tissue deformity. To further analyze the amount of discrepancy, the mean difference value was measured in each specific pair.
Asymmetry over the mandibular ramus and the periauricular region showed the highest mean difference between soft and hard tissue of 0.316 followed by the mandibular body 0.229 and the maxillary bone at 0.181. The chin and zygomatic area showed moderate difference at 0.136 and 0.022 respectively. While the nasal area showed the least difference at just 0.002.
Discussion
1-Facial asymmetry has become a common complaint of patients seeking the maxillofacial surgery clinic. Diagnosis and treatment planning has always been the most challenging part of the treatment [26]. Clinical examination and patient interview were and still is a crucial part of the diagnosis and planning step. However, due to complexity of the facial anatomy, most facial asymmetries may not present an easy diagnosis. For that reason, adjunct investigations are usually ordered to aid in the diagnosis [27].
2-Radiological examination of the facial skeleton and soft tissue is one of the most valuable tests that the clinician will require. Interpretation of CT scan and reliable measurement usually need a trained eye and experience [29]. Even with that available, controversies exist and inter-examiner reliability of accurate identification of facial structures cannot be guaranteed. For this reason, a computer aided algorithm was used to identify the facial regions and accurately and reproducibly measure the amount of asymmetry present based on root mean square deviation RMSD values [30]. Patel et. al., also describes the same methodology and found that the interoperative agreement on defining the midsagittal plane in patients with facial asymmetries are difficult and it resulted in a statistically significant margin (P=0.8) of error when five surgeons determined the facial landmarks defining the position of the facial midline [31].
3-Other types of radiological investigation such as OPG and Lateral and PA Cephalograms are commonly used to get an idea about the amount of soft and hard tissue deformities. However, being two-dimensional representation of a three-dimensional object inherently makes them inaccurate in diagnosing and comprehending the complete extend of the defects [32]. According to a research by Hajeer et. al., analyzing facial proportions for orthognathic corrections, they found that there were 18% more chances of miscalculation of the facial proportions using two-dimensional media, like 2D photographs and lateral cephalometrics, when compared to 3D data from facial laser scans and CBCT imaging. Additionally, there were a significant difference (P=0.01) when multiple anatomical measurements compared between 3D and 2D data sets signaling the importance for change to three-dimensional imaging as a routine necessity and not as a luxury [33]. And this corresponds to the finding in this paper as well.
4-Incidents of facial deformity and asymmetry varies by the region. In a study by Anu et. al., (2015) they found that most of the defects were in the chin where the mandibular bone was the causative factor followed by the cheek and the malar area. Whereas the lips and the nose were less likely affected [28]. These correspond with the results of this research, where most the deformities were noted in those areas. As the largest amount of asymmetry was noted in the mandibular body bone, zygomatic bone and soft tissue, chin, the nasal bone and soft tissue.
5-Asymmetry in the mandibular ramus and the condyle translated poorly to the overlaying periauricular region soft tissue. In most of the cases with bony asymmetry, there were insignificant soft tissue deformity. Suggesting that correction of the bony deformity in that area with implants or any other camouflaging technique yields less visible soft tissue correction and overcorrection of the hard tissue defect should be done to make tangible appearance on the skin. A paper by Tatch W. (2020) demonstrated this effect and why overcorrection of the bone is necessary to give a symmetrical soft tissue. However, the article did not specify an objective way for measuring the amount of overcorrection needed [34].
6- This current result, showed that, on the end of the scale, hard and soft deformity of the nose were very closely related to each other and had an insignificant difference (P=0.649) in the amount of asymmetry present between them. These results make it clear that even a simple deformity of the nasal bone has direct effect visible on the overlaying skin. Care should be taken in correcting deformity in that area, meticulous technique and precise one to one bony implant should be used. Chen et. al., (2008) discussed this issue by using porous polyethylene implants in thirty-two patients presented with nasal deformity after trauma where bone substitution was necessary.
Other regions studied in this research were in the middle ground between those two areas above. Ranking from most significant difference to the least were Mandibular body area, Maxillary area, chin area and the zygomatic region. Mandibularbody area presented with the mean difference of 0.229 and p<0.000 , Maxillary area with the mean value of 0.181 and P<0.000 and the Chin area’s mean difference was 0.136 with p<0.000.
The results of this study make it clear why clinical examination is an important pillar of the treatment protocol. As it is clear, judging by only radiological scan can mislead the clinician for correcting or overcorrecting deformities that have little to no clinical significance to the patient. A systematic review published Akhil et. al., pointed out that many patients with calculatable facial asymmetry or deformity on radiographs do not need any corrective treatment as some asymmetry is natural and unperceivable [35].
The exact relationship between the bony deformity and soft tissue deformity per anatomic region were as follow:
1- Zygomatic Bone to soft tissue: 1:1.015
2- Maxillary Bone to soft tissue: 1:1.13
3- Nasal Bone to soft tissue: 1:1.001
4- Mandibular ramus to soft tissue: 1:1.265
5- Mandibular symphyseal bone to soft tissue: 1:1.099
6- Mandibular Body to soft tissue: 1:1.174
Those ratios can be simply explained to mean that when a 1mm soft tissue movement is desired the corresponding amount of bony movement needs to be corrected to give the required results. An example of this would be that correcting a nasal bone defect with a 2mm facial implant will have almost 2mm change visible on the skin, however, a depressed periauricular region of a 2mm deficiency may need around (2x1.265) 2.53mm thick implant to get the same tissue effect. In the five of the six anatomical facial regions taken in this study, results were significant and considerable for the amount of the difference present. Influence of the facial skeleton on the appearance of the skin varies from region to region.
Wide-field CBCT scan almost provide the same accuracy and 3D representation of the facial anatomy for the fraction of the radiation dose, it is even cheaper and more readily available. However, participants in our study were already had CT scan taken for the planning of their orthognathic surgeries and cutting guides preparation in which CT scans represent a more accurate and highly superior bone surface mesh for preparation of 3D printed parts used in the surgeries [36]. A paper published by Van Dessel et. al., on the accuracy and reliability of CBCT scan and CT scans showed an overestimation of porosity of the alveolar bone when the CBCT scans were compared to gold standard CT scans. As CBCT machines use less radiation dose and expose in a fan fashion covering large area with single exposure comparing to CT scan when each slice gets to be exposed at the expense or more radiation dose. This simply demands the CBCT machines to produce images with more calculations rather than actual data and this in turn will introduce more inaccuracies in the reconstructed image [37].
The RMSD value proofed to be a reliable way of measuring the amount of asymmetry present.31 However, correction plans should not be based on the amount of bony deformity alone as there are a significant difference between the amount of bony asymmetry and soft tissue deformity in the same anatomical region.
These results are logical and goes with the current clinical practice of facial aesthetic surgeons. This study provides a quantitative and objective measurement and confirmation of the current guidelines. Furthermore, this research adds more detail regarding specific anatomical regions and the exact relationship of soft and hard tissue per site.
Conclusion
This research presents a reliable, reproducible and operator independent method for measuring facial Skelton and soft tissue deformities from patients CT scan as well as calculating the exact relationship between them. The effects of the underlying bony deformity on the overlying soft tissue and skin appearance are not consonant and change significantly based on the anatomical region. The thinner the skin structure the more apparent are the effects of the hard tissue asymmetry.
These exact ratios can be used in calculating the thickness of the implants or the bony movement needs to be performed. In the malar region 1:1.015, Maxillary and upper lip region 1:1.13, the nose 1:1.001, Mandibular ramus and preauricular region: 1:1.265, the Chin area 1:1.099 and finally in the Mandibular body region 1:1.174.
The ratios can be translated to millimeters or any appropriate units of measurements. The latter number corresponds to the amount of bony movement necessary to get 1mm of soft tissue movement in its related region.
The results of this study will greatly aid maxillofacial surgeons in diagnosis and treatment plan formulations for cases with facial asymmetries and deformities. It will act as a guide for designing facial implants and determining their exact thickness to better estimate their soft tissue and final results.
Additionally, using results from this paper, a facial implant designer might reverse-engineer the procedure and start form virtually correcting the soft tissue defect and then calculating the mount of bone needed. As of now, most caregivers used one-to-one ratio, meaning the implant design was the same size of the defect. However, as shown in this article, the ratio of bone to soft tissue effect varies considerably based on the facial anatomical region.
These methods currently laid in this paper may act as future refence for more studies going in depth and calculating more facial regions on much larger population sample which was not feasible here due to lack of facilities and time limitations.
References
- Choi KY. Analysis of Facial Asymmetry. Arch Craniofac Surg. 2015; 16(1): 1-10. doi:10.7181/acfs.2015.16.1.1
- Quantitative Facial Asymmetry, Mulliken JB. The molders of this plastic surgeon and his quest for symmetry. J Craniofac Surg 2004;15: 898-908.
- Nanda R, Margolis MJ. Treatment strategies for midline discrepancies. Semin Orthod. 1996; 2(2): 84-89.
- Burstone CJ. Diagnosis and treatment planning of patients with asymmetries. Semin Orthod. 1998; 4(3):153-164.
- 5- Lee MS, Chung DH, Lee JW, Cha KS. Assessing soft-tissue characteristics of facial asymmetry with photographs. Am J Orthod Dentofacial Orthop. 2010; 138(1): 23-31.
- Lundström A, some asymmetries of the dental arches, jaws, and skull, and their etiological significance, Am J Orthod 1961; 47(2): 81–106.
- Pirttiniemi PM, Associations of mandibular and facial asymmetries – a review, Am J Orthod Dentofac Orthop, 1994; 106: 191-200.
- Bishara SE, Burkey PS, Kharouf JG. Dental and facial asymmetries: a review. Angle Orthod. 1994; 64: 89–98.
- Obwegeser HL, Makek MS. Hemimandibular hyperplasia: hemimandibular elongation, J Maxillofac Surg, 1986; 14: 183–208.
- Kim JY, Jung HD, Jung YS, Hwang CJ, Park HS. A simple classification of facial asymmetry by TML system, J Craniomaxillofac Surg 2014; 42: 313–320.
- Hwang HS, A new classification of facial asymmetry, in: J.A. McNamara (Ed.), Early Orthodontic Treatment: Is the Benefit Worth the Burden? [Craniofacial Growth Series], 44 University of Michigan Ann Arbor, 2007; pp. 269-294
- Legan HL. Surgical correction of patients with asymmetries. Semin Orthod. 1998; 4(3): 189-198.
- Facial asymmetry: etiology, evaluation, and management. Chang Gung Med J. 2011; 34(4): 341-351.
- Cohen Jr. MMJr. Perspectives of craniofacial asymmetry. Part IV. Hemiasymmetries. Int J Oral Maxillofac Surg. 1995; 24: 134–141.
- Vig PS, Hewitt AB. Asymmetry of the human facial skeleton. Angle Orthod. 1975; 45: 125–129.
- Hosseinzadeh Nik T, Gholamrezaei E, Keshvad MA. Facial asymmetry correction: From conventional orthognathic treatment to surgery-first approach. J Dent Res Dent Clin Dent Prospects. 2019; 13(4): 311-320. doi:10.15171/joddd.2019.047
- Binder WJ. Custom-designed facial implants. Facial Plast Surg Clin North Am. 2008; 16(1): 133-146, vii. doi: 10.1016/j.fsc.2007.09.001. PMID: 18063252.
- Lee JK, Jung PK, Moon CH. Three-dimensional cone beam computed tomographic image reorientation using soft tissues as reference for facial asymmetry diagnosis. Angle Orthod. 2014; 84(1): 38–47.
- Sailer HF, Haers PE, Zollikofer CP, Warnke T, Caris FR, Stucki P. The value of stereolithographic models for preoperative diagnosis of craniofacial deformities and planning of surgical corrections. Int J Oral Maxillofac Surg. 1998; 27: 327–333.
- Kornreich D, Mitchell AA, Webb BD, Cristian I, Jabs EW. Quantitative assessment of facial asymmetry using three-dimensional surface imaging in adults: validating the precision and repeatability of a global approach. Cleft Palate–Cr Aniofacial J. 2016; 53: 126–131.
- Fanous N, Yoskovitch A. Estimating implant size in chin augmentation: A simplified approach. Can J Plast Surg. 2003; 11(3): 161-165. doi:10.1177/229255030301100305
- Ho M, Goldfarb J, Moayer R, Nwagu U, Ganti R, Krein H, Heffelfinger R, Hutchinson ML. Design and Printing of a Low-Cost 3D-Printed Nasal Osteotomy Training Model: Development and Feasibility Study. JMIR Med Educ. 2020; 6(2): e19792. doi: 10.2196/19792. PMID: 33200998; PMCID: PMC7708083.
- Cheong YW, Lo LJ. Facial asymmetry: etiology, evaluation, and management. Chang Gung Med J. 2011; 34(4): 341-351. PMID: 21880188.
- Coutsias EA, Wester MJ. RMSD and Symmetry. J Comput Chem. 2019; 40(15): 1496-1508. doi: 10.1002/jcc.25802. Epub 2019 Mar 3. PMID: 30828834.
- Taylor HO, Morrison CS, Linden O, Phillips B, Chang J, Byrne ME, Sullivan SR, Forrest CR. Quantitative facial asymmetry: using three-dimensional photogrammetry to measure baseline facial surface symmetry. J Craniofac Surg. 2014; 25(1): 124-128. doi: 10.1097/SCS.0b013e3182a2e99d. PMID: 24406564.
- Bishara SE, Burkey PS, Kharouf JG. Dental and facial asymmetries: a review. Angle Orthod. 1994; 64(2): 89-98.
- Chia MS, Naini FB, Gill DS. The aetiology, diagnosis and management of mandibular asymmetry. Ortho Update. 2008; 1(1): 44-52.
- Anu E Kaipainen, Kevin R Sieber, Rania M Nada, Thomas J Maal, Christos Katsaros, Piotr S Fudalej, Regional facial asymmetries and attractiveness of the face, European Journal of Orthodontics, 2016; 38(6): 602–608.
- Padwa BL, Kaiser MO, Kaban LB. Occlusal cant in the frontal plane as a reflection of facial asymmetry. J Oral Maxillofac Surg. 1997; 55(8): 811-816; discussion 817.
- Vivien Lum, Mithran S Goonewardene, Ajmal Mian, Peter Eastwood. Three-dimensional assessment of facial asymmetry using dense correspondence, symmetry, and midline analysis. American Journal of Orthodontics and Dentofacial Orthopedics. 2020
- Patel A, Islam SM, Murray K, Goonewardene MS. Facial asymmetry assessment in adults using three-dimensional surface imaging. Prog Orthod. 2015; 16: 36. doi: 10.1186/s40510-015-0106-9. Epub 2015 Oct 21. PMID: 26490376; PMCID: PMC4614853.
- Gateno J, Xia JJ, Teichgraeber JF: A new three-dimensional cephalometric analysis for orthognathic surgery. J Oral Maxillofac Surg 2011; 69: 606–622.
- Hajeer MY, Millett DT, Ayoub AF, Siebert JP. Applications of 3D imaging in orthodontics: part I. J Orthod. 2004; 31(1): 62-70. doi: 10.1179/146531204225011346. PMID: 15071154.
- Tatch W. Correction of Facial Asymmetry with Combination of Osteotomy and Mandibular Implants: A Case Report and Review of the Literature. The American Journal of Cosmetic Surgery. 2020; 37(1): 31-36. doi:10.1177/0748806819849795
- Akhil G, Senthil Kumar KP, Raja S, Janardhanan K. Three-dimensional assessment of facial asymmetry: A systematic review. J Pharm Bioallied Sci. 2015;7(Suppl 2): S433-S437. doi:10.4103/0975-7406.163491
- Hwang HS, Hwang CH, Lee KH, Kang BC: Maxillofacial 3-dimensional image analysis for the diagnosis of facial asymmetry. Am J Orthod Dentofacial Orthop 2006; 130: 779-785.
- Van Dessel J, Nicolielo LF, Huang Y, Coudyzer W, Salmon B, Lambrichts I, Jacobs R. Accuracy and reliability of different cone beam computed tomography (CBCT) devices for structural analysis of alveolar bone in comparison with multislice CT and micro-CT. Eur J Oral Implantol. 2017; 10(1): 95-105. PMID: 28327698.

