Failed Back Surgery Syndrome (Post-Laminectomy Syndrome): The Prevalence, Accompanying Signs, Possible Causes, Management and Outcomes; One-Year Trial at the Teaching Hospitals in Sana’a City, Yemen
Majed Ali Amer Ali, Monya Abdullah Yahya El-Zine, Hassan Abdulwahab Al-Shamahy
Department of Neurosurgery, Faculty of Medicine and Health Sciences, Sana’a University, Republic of Yemen
Departement of Histopathology, Faculty of Medicine and Health Sciences, Sana’a University, Republic of Yemen
Department of Basic Sciences, Faculty of Dentistry, Sana’a University, Republic of Yemen
Received Date: 02/07/2021; Published Date: 26/07/2021
*Corresponding author: Hassan A Al-Shamahy, Faculty of Dentistry, Sana’a University. P.O. Box 775 Sana’a, Yemen. Tel: +967-1-239551, Mobile: +967-770299847, E-mail: shmahe@yemen.net.ye, https://orcid.org/0000-0001- 6958-7012
Abstract
Background: FBSS is a term that groups the conditions with recurring low back pain after spine surgery with or without a radicular component.
Aims: The study aimed to investigate the prevalence of FBSS and describe the age, gender, accompanying signs, possible causes of FBSS, methods of diagnosis, management, and outcomes after treatment for patients admitted to Al-Kuwait University Hospital, Sana'a. Yemen for spine surgery.
Materials and methods: A one-year follow-up study was conducted on patients after spine surgery at Kuwait University Hospital - Sana'a, for one year from October 1, 2018 until October 31, 2019. The variables of the study were qualitative (gender, signs, symptoms, type managements, the outcome) and quantitative (age).
Results: A total of 283 spinal surgeries were performed during the study period, of which 31 patients developed FBSS. The prevalence of FBSS was 11%, of whom 12 were female and 19 were male, with a ratio of 1.0:1.6 and the most common age group was 40–49 years with a mean age of 50.3 years. The first symptoms that occurred after laminectomy were back and leg pain (77.5%), delayed onset (48.3%), and herniated disc was the common diagnostic cause associated with FBSS (58.1%) followed by instability (32.2%), while the canal stenosis was rare (9.7%). On the subject of the type of first operation performed for FBSS patients, laminectomy and discectomy were the popular surgical procedure (64.5%), followed by laminectomy (16.1%), and the fusion procedure (13%) and only 3.2% by foraminotomy. Diagnostic causes of FBSS were wrong level (21.1%), recurrent disc at the same level (29%), canal stenosis (3.2%), root injury (9.7%), instability (19.4%), fibrosis (9.7%), and adhesive arachnoiditis (6.5%). Regarding the second types of management applied in FBSS patients, surgical intervention was performed in 61.3% of FBSS patients and conservative treatment performed for 38.7%.
Conclusion: In short, FBSS is a complex and challenging disease with multiple known causes and largely unknown etiologies. In this study, the prevalence of FBSS was low, it was more common in males and herniated disc was the common diagnostic cause associated with FBSS followed by instability.
Keywords: Causes; Diagnosis; FBSS; Management; Prevalence; Spine surgery; Symptoms; Yemen.
Introduction
Failed Back Surgery Syndrome (FBSS) is an expression that joins cases with recurring low back pain subsequent to spine surgery with or without a root component. It was initial articulated by North et al. [1] in 1991, and this may in fact be a misnomer since the clinical appearance could be produced by a disparity between patient and surgeon's preoperative expectations [2]. Since FBSS is a recurrent low back pain, it is difficult to distinguish spine surgery as the main cause because low back pain is a common presentation among adults, ranging between 60% and 85% [3]. Back pain has the highest indirect cost among chronic and orthopedic conditions, estimated at $19.8 billion [4]. Alternatively, the occurrence of spinal surgery in common and spinal fusion, particularly amongst adults, has increased considerably in current years [5,6]. The rate of FBSS varies between 10% and 40% subsequent to lumbar laminectomy with or without fusion [2] but this pain may be due to failed lumbar laminectomy as controlled trials have shown a high incidence of failed surgery as high as 19% [7] Other studies have confirmed that the success rate of decompression surgery appears to be between 65% and 75% only [8,9].
Many factors can add to the appearance or progress of FBSS, contain residual or recurrent intervertebral disc herniation, persistent post-operative pressure on the spinal nerve, altered joint mobility, persistent post-operative pressure on the spinal nerve, joint hypermobility with instability, depression, scar tissue (fibrosis), and insomnia, anxiety, spinal decompensation and even skin infection [3]. A person might have a propensity to developing FBSS as a result of general disorders for instance autoimmune disease, diabetes, and peripheral vascular disease [5].
However, in Yemen as in the majority of Arab countries, there are no specialized epidemiological records dedicated to FBSS, which is why it is important to encourage, update, build and continue to provide studies on FBSS with the purpose of achieving greater extent and impact on public health, with effective diagnosis and appropriate treatment with the aim of promoting to reduce the suffering of patients and minimizing the potential consequences. This follow up study is aimed to determine the prevalence of FBSS and describe FBSS cases age, gender, symptoms, accompanying signs and possible causes of FBSS, methods of diagnosis, managements, and outcomes after treatment for patients admitted to Kuwait University Hospital, Sana'a. Yemen for spine surgery.
Materials and Methods
A follow up study for one year was performed on patients after spine surgery at Al-kwait university Hospital - Sana'a, for a period of 1 year from October 1, 2018 to October 31, 2019. The variables of the study were qualitative (gender, signs, symptoms, type managements, the outcome) and quantitative (age). Diagnosis of FBSS were created in sequence with the North et al. 1991, definition.
Table 1: Age distribution of patients with failed back syndrome or post-laminectomy syndrome among patients admitted to Al-Kuwait University hospital.
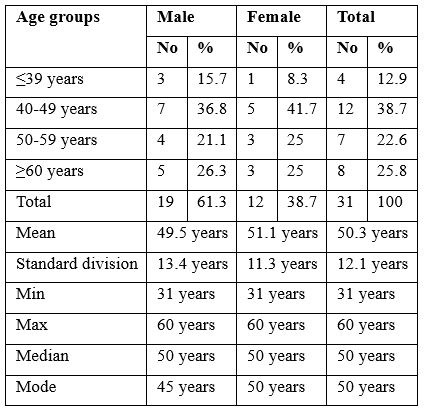
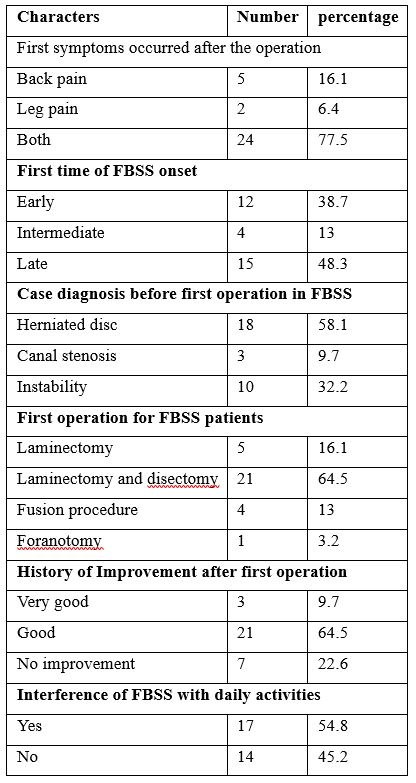
Table 2: Clinical information of patients with failed back syndrome or post-laminectomy syndrome among patients admitted to Al-Kuwait University hospital.
Ethical Approval
The ethical approval was obtained from the Medical Research and Ethics Committee at the Faculty of Medicine and Health Sciences at Sana'a University with a reference number (213) dated 1-01-2018. Also, all data, including patient identification, have been kept confidential.
Table 3: The potential diagnostic causes of failed back syndrome among patients admitted to Al-Kuwait University hospital.
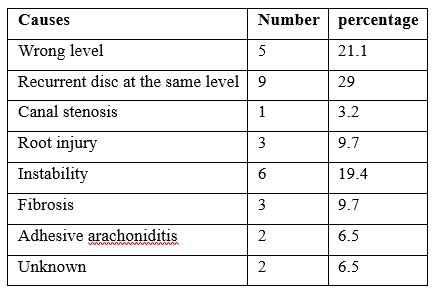
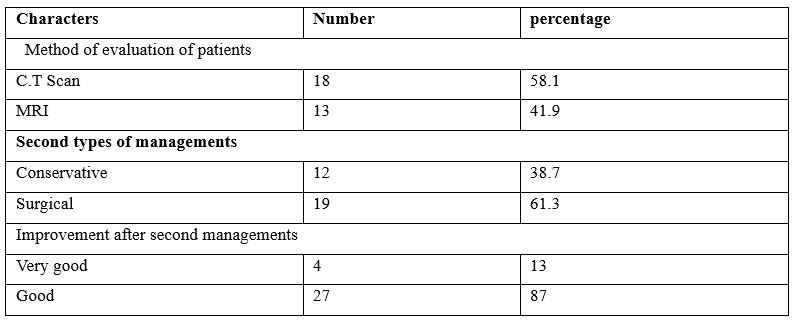
Table 4: The methods of diagnosis and managements used on the failed back syndrome patients admitted to Al-Kuwait University hospital.
Results
There was a total of 283 spine surgeries done during the study period, out of them 31 patients were developed FBSS. The prevalence rate of FBSS was 11%, Of these, 12 were females and 19 were males, with a ratio of 1.0: 1.6 and most common age group was 40-49 years with mean age of 50.3 years. Table 1 shows age distribution of patients with failed back syndrome Most of the FBSS patients were in the 40-50 year age group (38.7%) followed by the ≥ 60-year age group with 25.8%. The patients' ages ranged from 31-60 years with a mean total age of 50.3 years, while for males it was 49.5 years and for females 51.1 years. Table 2 shows the clinical information of patients with failed back syndrome. Regarding the first symptoms that occurred after a laminectomy, the incidence of back pain only was 16.1% and leg pain only was 6.4%, while most patients had back and leg pain (77.5%). Concerning the first-onset of FBSS: Early onset occurred in 38.7% of FBSS patients, whereas mean time onset occurred in 13% of FBSS patients, while late onset occurred more frequently as 48.3% showed late onset of FBSS. With regard to FBSS by diagnosis, herniated disc was the common diagnostic cause associated with FBSS patients accounting for 58.1% of cases, followed by instability accounting for 32.2%, while canal stenosis accounted for only 9.7%. On the subject of the type of first operation done for FBSS patients, laminectomy and discectomy were the popular surgical procedures among FBSS patients numbering 64.5%, while the number of laminectomies was 16.1%, the fusion procedure done for 13% of the patients and foraminotomy was done for only 3.2%. A history of improvement occurred after the first operation in the patients between good improvement in 64.5% of FBSS patients and very good improvement occurred in 9.7% while there was no improvement in 22.6% of FBSS cases. Regarding FBSS interference with daily activities of FBSS patients, 54.8% of FBSS patients answered yes while the rest said no. Table 3 shows the possible diagnostic causes of failed back syndrome among the studied patients. Wrong level was diagnosed in 21.1%, recurrent disc at the same level was diagnosed in 29%, canal stenosis was diagnosed in only 3.2%, root injury was diagnosed in 9.7%, instability in 19.4%, fibrosis in 9.7%, and adhesive arachnoiditis in 6.5 %. While 6.5% of FBSS patients had no causes diagnosed.
Table 4 shows the diagnostic and management methods used, and results of treatments on failed back syndrome patients admitted to Al-Kuwait University Hospital. Regarding the assessment and prognostic methods used in the diagnosis and follow-up of patients, CT was used in 58.1% of FBSS patients and MRI was used in 41.9% of patients. Regarding the second types of management applied in FBSS patients, surgical intervention was performed in FBSS patients in 61.3% and conservative treatment in 38.7%. Improvement after second administrations was very good in 13% of patients and was good in 87% of patients.
Discussion
In the present study, the prevalence of FBSS was 11%, and this rate is in the range reported elsewhere as the incidence of FBSS is recognized to be between 10% and 40% after lumbar laminectomy with or without fusion [2]. In the current study, the female to male ratio was 1.0:1.6, and this result differs from that reported by Fritsch et al. [10], and Parker et al. [11] where the rate is approximately equal in both sexes. In the present study, the most frequent age group was 40-49 years with a mean age of 50.3 years. These results differ from those reported from Georgetown University where the mean age of BFSS patients was 67 years, and 80% of them were over 60 years old [12,13]. The incidence of FBSS in younger age groups compared to older ages in other countries around the world may reflect that the lifespan of people in Yemen is lower than that in other countries for example for Iran it is 77 years old, Saudi Arabia is 75 years old and the USA is 85 years old The United Kingdom is 85 years old, while in Yemen 66 years [14].
Regarding the first symptoms that occurred after laminectomy in the current study, the incidence of back pain was only 16.1% or leg pain only 6.4%, while most patients had back and leg pain (77.5%). Symptoms of FBSS should ideally begin with a detailed evaluation of the history and clinical examination. The evaluation should compare preoperative symptoms with recent symptoms. If the pain is in its first onset or is the similar such as the pain before surgery, the cause may be intraoperative or postoperative complications [15]. Central is defined as pain move on the way to or from the lumbar spine as a result of repetitive motions, and is suggestive of disc pain. Radicular pain may be due to insufficient decompression, foraminal stenosis, recurrent disc herniation or epidural fibrosis [15]. In most cases [15], it includes back and foot pain, as it is with the patients of the current study.
In the current study, regarding first onset of FBSS: early onset occurred in 38.7% of FBSS patients, while median time onset occurred in 13% of FBSS patients, while late onset occurred more frequently as 48.3% showed late onset. This result is similar to that reported by Waguespack et al. [16] and Waddell et al. [17] as late onset of FBSS occurred in more than 50% of their patients. If the pain is in its early beginning or is the similar such as the pain before surgery, it may be attributable to intraoperative or postoperative complications [15]. Regarding FBSS by postoperative diagnosis (postoperative causes), herniated disc was the most common diagnostic cause associated with FBSS patients accounting for 58.1% of cases, followed by instability accounting for 32.2%. Postoperative causes can be separated into surgery-related factors and disease progression. Recurrent herniated discs are known to occur in approximately 6%–23% of patients who underwent microdiscectomy at the same site or adjacent level [11, 18] less than reported in our study.
Adjacent segment disease, a known complication of lumbar fusion with radiological and clinical subcategories, is a significant risk factor for re-operation post primary micro endoscopic discectomy [18]. On the other hand, the incidence of clinical instability (adjacent segment disease) is thought to be approximately 27% [19] close to our rate (32.2%); Sagittal balance plays an important role because unbalanced and compensated balanced spines predispose to adjacent disc degeneration [20]. Therefore, radicular pain might be due to foramen stenosis, as nerve root entrapment in epidural fibrosis is believed to be a causative or contributing factor to postoperative pain in 20% - 36% of FBSS cases [2,15], while canal stenosis accounted for 9.7%. in the current study. A history of improvement occurred after the first operation in the patients between good improvement in 64.5% of FBSS patients and very good improvement occurred in 9.7% while there was no improvement in 22.6% of FBSS cases. Regarding FBSS interference with daily activities of FBSS patients, 54.8% of FBSS patients answered yes while the rest said no.
In the current study, a wrong level was diagnosed in 21.1%, recurrent disc at the same level was diagnosed in 29%, canal stenosis was diagnosed in only 3.2%, root injury was diagnosed in 9.7%, instability in 19.4%, fibrosis in 9.7%, and adhesive arachnoiditis in 6.5 %. While 6.5% of FBSS patients had no causes diagnosed. Patients who have undergone one or more operations on the lumbar spine and continue to experience pain afterward can be divided into two groups. The first group consisted of those for whom surgery was not actually indicated or for whom the surgery was not likely to achieve the desired result, and those for whom surgery was indicated but technically did not achieve the desired result [7]. Patients whose complaints of pain are of a radicular nature have a better chance of achieving a good outcome than those whose pain is limited to back pain. The second group includes patients who underwent incomplete or inadequate surgeries. Lumbar spinal stenosis possibly will be unnoticed, particularly when correlated with disc protrusion or herniation. Disc removal, while not treating the primary presence of the stenosis, can lead to disappointing results [8]. Occasionally operating on the wrong level occurs, as does failure to recognize an extruded or sequestered disc fragment. Inadequate or inappropriate surgical exposure can lead to other problems if the underlying pathology is not reached. Hackelius reported a 3% incidence of serious nerve root damage [9]. Regarding assessment and prognostic methods used in diagnosis and follow-up of patients, CT was used in 58.1% of FBSS patients and MRI was used in 41.9% of patients. As it known Computed Tomography (CT), another excellent modality to assess spinal instrumentation-related complications, can help qualify and quantify a fusion mass in an instrumented spine when instrumentation removal is contemplated [21]. In patients with contraindications to MRI, Computed Tomography (CT) myelography can be employed which might show the compression of neural structures by bony or other elements [15]. The treatment of FBSS presents a major, similar dilemma to the patient and physician. It needs to be emphasized that FBSS treatment should be multidisciplinary. As a team, pain physicians, spine surgeons, physical therapists, and psychiatrists should target demystifying the pain for the patient. Further, the alternative definition of FBSS that “its consequences when the result of lumbar spine surgery does not convene the preoperative expectations of the patient and surgeon” [16], leads to patient education being considered paramount; patients should be an integral part of the treatment process. In the current study regarding the second types of management applied in our FBSS patients, surgical treatment was performed in FBSS patients in 61.3% and conservative intervention in 38.7%. Removal of a disc at one level can lead to disc herniation at a different level at a later time. Even the most complete surgical excision of the disc still leaves 30–40% of the disc, which cannot be safely removed. This retained disc can re-herniate sometime after surgery. Virtually every major structure in the abdomen and the posterior retroperitoneal space has been injured, at some point, by removing discs using posterior laminectomy/discectomy surgical procedures. Most notable is the rupture of the left internal iliac vein, which is located near the front of the disc [22,23]. In some studies, recurrent pain in the same radicular pattern or a different pattern can be as high as 50% after disc surgery [23,24]. In fact, Surgical management of FBSS should be reserved for patients with a documented anatomic or pathologic cause for their pain and/or with failed medical treatment [2]. As the fact, the success rate of the surgery decreases with every reoperation [26].
Conclusion
In short, FBSS is a complex and challenging disease with multiple known causes and largely unknown etiologies. Accurate diagnosis is of paramount importance, and its management must be multidisciplinary. In this study, the prevalence of FBSS was low, it was more common in males and herniated disc was the common diagnostic cause associated with FBSS followed by instability. Therefore, special attention should be paid to cases of recurrent herniated discs and imbalances after spinal surgery.
Author Contribution
This study was completed by Assistant Professor Mjged Ali Amer Ali the neurosurgeon at the Al-Kwait university Hospital - Sana'a City, and Assistant professor of neurosurgar in Sana’a university, Monya Abdullah Y El-Zine, Assistant Professor of Histopathology at Sana'a University and Prof. Dr. Hassan Abdulwahab Al-Shamahy, Faculty of Medicine, Sana'a University. All authors analyzed the data, wrote the manuscript, and reviewed it.
Acknowledgments
The authors would like to acknowledge the Al-Kwait university Hospital - Sana'a, Yemen which supported this work.
Conflict of Interest
"No conflict of interest associated with this work”.
References
- North RB, Campbell JN, James CS, et al. Failed back surgery syndrome: 5-year follow-up in 102 patients undergoing repeated operation. Neurosurgery 1991; 28: 685-690.
- Chan CW, Peng P. Failed back surgery syndrome. Pain Med 2011; 12: 577-606.
- Schmidt CO, Raspe H, Pfingsten M, et al. Back pain in the German adult population: prevalence, severity, and sociodemographic correlates in a multiregional survey. Spine (Phila Pa 1976) 2007; 32: 2005-2011.
- Stewart WF, Ricci JA, Chee E, Morganstein D, Lipton R. Lost productive time and cost due to common pain conditions in the US workforce. JAMA 2003; 290: 2443-2454.
- Sebaaly A, Lahoud MJ, Rizkallah M et al. Etiology, Evaluation, and Treatment of Failed Back Surgery Syndrome. Asian Spine J 2018; 12(3): 574-585.
- Deyo RA, Gray DT, Kreuter W, Mirza S, Martin BI. United States trends in lumbar fusion surgery for degenerative conditions. Spine (Phila Pa 1976) 2005; 30:1441-1445.
- Peul WC, van den Hout WB, Brand R, Thomeer RT, Koes BW; Leiden-The Hague Spine Intervention Prognostic Study Group. Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two-year results of a randomised controlled trial. BMJ 2008; 336: 1355-1358.
- Pearson A, Lurie J, Tosteson T, Zhao W, Abdu W, Weinstein JN. Who should have surgery for spinal stenosis? treatment effect predictors in SPORT. Spine (Phila Pa 1976) 2012; 37: 1791-802.
- Fokter SK, Yerby SA. Patient-based outcomes for the operative treatment of degenerative lumbar spinal stenosis. Eur Spine J 2006; 15: 1661-1669.
- Fritsch EW, Heisel J, Rupp S. The failed back surgery syndrome: reasons, intraoperative findings, and long-term results: a report of 182 operative treatments. Spine (Phila Pa 1976) 1996; 21: 626-633.
- Parker SL, Mendenhall SK, Godil SS, et al. Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res 2015; 473:1988-1999.
- Herno A, et al., "Computed tomography findings 4 years after surgical management of lumbar spinal stenosis. No correlation with clinical outcome". Spine 1999; 24(21): 2234–2239.
- Caputy A. J.; Luessenhop A. J. "Long-term evaluation of decompressive surgery for degenerative lumbar stenosis". J. Neurosurg 1992; 77 (5): 669–76.
- UN Population Division. Period life expectancy at birth. UN. 2019.
- Guyer RD, Patterson M, Ohnmeiss DD. Failed back surgery syndrome: diagnostic evaluation. J Am Acad Orthop Surg 2006; 14: 534-543.
- Waguespack A, Schofferman J, Slosar P, Reynolds J. Etiology of long-term failures of lumbar spine surgery. Pain Med 2002; 3: 18-22.
- Waddell G, McCulloch JA, Kummel E, Venner RM. Nonorganic physical signs in low-back pain. Spine (Phila Pa 1976) 1980; 5: 117-125.
- Hong X, Liu L, Bao J, Shi R, Fan Y, Wu X. Characterization and risk factor analysis for reoperation after microendoscopic diskectomy. Orthopedics 2015; 38: e490-496.
- Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J 2001; 10: 314-319.
- Mazzie JP, Brooks MK, Gnerre J. Imaging and management of postoperative spine infection. Neuroimaging Clin N Am 2014; 24: 365-374.
- Manca A, Kumar K, Taylor RS, et al. Quality of life, resource consumption and costs of spinal cord stimulation versus conventional medical management in neuropathic pain patients with failed back surgery syndrome (PROCESS trial). Eur J Pain 2008; 12: 1047-1058.
- North R, Shipley J, Prager J, et al. Practice parameters for the use of spinal cord stimulation in the treatment of chronic neuropathic pain. Pain Med 2007;8 Suppl 4: S200-275.
- Rigoard P, Assaker R. Failed back surgery syndrome: from pathophysiology to recent therapeutic advances in neurostimulation: introduction. Neurochirurgie 2015; 61 Suppl 1: S5.
- Kogias E, Franco Jimenez P, Klingler JH, Hubbe U. Minimally invasive redo discectomy for recurrent lumbar disc herniations. J Clin Neurosci 2015; 22: 1382-1386.
- Nachemson AL. Evaluation of results in lumbar spine surgery. Acta Orthop Scand Suppl 1993; 251: 130-133.Harrop JS, Youssef JA, Maltenfort M, et al. Lumbar adjacent segment degeneration and disease after arthrodesis and total disc arthroplasty. Spine (Phila Pa 1976) 2008; 33: 1701-1707.

