Evaluation of A Light-Cured Calcium Silicate (Theracal Lc) in Primary Molars Pulpotomy after 12 Months; A Randomized Controlled Trial
Abdullah H, Wassel M, Abd-Elaziz, A Farid M
Pediatric Dentistry and Dental Public Health Department, Ain Shams University, Egypt.
Oral Radiology Department, Ain Shams University, Egypt.
Received Date: 15/12/2020; Published Date: 22/12/2020
*Corresponding author: Mariem Osama Wassel, Associate Professor, Pediatric Dentistry and Dental Public Health Department, Faculty of Dentistry, Ain Shams University, Cairo, Egypt. Organization of African Union Street, Abbasia, Cairo. Post NO.: 11566. Email: mariem.wassel@dent.asu.edu.eg, Tel: 202/ 22639088, Cell phone: +2 01064871416, Fax: 202/22603983, ORCID ID: 0000-0002-2561-2519
Abstract
Background: To compare clinically and radiographically TheraCal LC and form cresol pulpotomies in primary molars.
Methods: Sixty mandibular second primary molars were randomly assigned to TheraCal LC or 1:5 concentration formocresol in four to seven years-old healthy children. Clinical and radiographic assessments were performed at three, six, nine, and 12 months. Fisher’s Exact test was used for analysis at p≤0.05.
Results: No clinical failures were evident in both groups over the 12 months. At nine months, internal resorption was evident in two (6.7%) and three (10%) molars in TheraCal LC and formocresol, respectively. Inter-radicular bone resorption was evident in one (3.3%) and two (6.7%) molars in TheraCal LC and formocresol, respectively.
No new radiographic failures were evident at 12 months. No significant difference was found between both groups regarding radiographic failure (p=0.706).
Radiographic success at 12 months was 90% for TheraCal LC and 83.3% for formocresol.
Conclusions: TheraCal LC can be an effective medicament for vital pulpotomy in primary molars.
Keywords: Calcium silicate; light cured; TheraCal LC; Primary molars; Pulpotomy
Introduction
One of the major challenges in pediatric dentistry is maintaining primary teeth with pulp involvement in a healthy state until normal exfoliation. Pulpotomy is the complete removal of the coronal portion of dental pulp followed by placement of a medicament that will either preserve pulp vitality or devitalize radicular pulp.
It is a universally accepted treatment for pulpally involved primary teeth [1].
Although different materials and techniques were introduced for pulpotomy in primary teeth, formocresol remained the first-choice pulpal medicament for almost 100 years. Formocresol proved to be the most efficient, reliable, and successful material regardless the controversy related to its carcinogenicity and toxicity [2].
In 1993 Mineral Trioxide Aggregate (MTA), a tricalcium silicate material, was introduced as a new pulp medicament and turned to be one of the most versatile materials of this century in the field of dentistry. Studies proved that MTA has a good sealing ability, excellent long-term prognosis, good biocompatibility and also favors tissue regeneration [3-5].
MTA showed success rates very close to those of formocresol and was recommended by the American Academy of Pediatric dentistry as the best alternative to formocresol when a more biocompatible material is preferred and costs are not a concern [6].
However, the limitations of MTA are high cost, long setting time, and unease of handling, the last two limitations are especially important when it comes to pediatric dentistry where reducing chair time is always a goal.
In 2012, TheraCal LC (Bisco, Inc. Schaumburg IL, USA), a light-cured resin-modified calcium silicate material, was introduced into the markets.
It is indicated for direct and indirect pulp capping and as a protective base/liner under restorative materials including composite, amalgam and cements.
It has an alkaline pH and consists of tricalcium silicate particles in a hydrophilic monomer that stimulates hydroxyapatite and secondary dentin bridge formation through calcium release [7].
It basically combines the advantages of MTA along with ease of application, as it is syringe dispensed requiring no mixing, and command set. TheraCal LC was evaluated in few studies in primary molars as a medicament for direct and indirect pulp capping for 12 months, and revealed insignificant success rates compared to MTA [8,9].
TheraCal LC was also evaluated in primary molars pulpotomy but only for 6 months and was found comparable to formocresol both clinically and radiographically [10].
Therefore, the current study was designed to clinically and radiographically evaluate TheraCal LC as a bioactive material for vital pulpotomy in primary molars compared to conventional formocresol pulpotomy after 12 months. The PICOT question was: In mandibular second primary molars with carious exposure (P), would TheraCal LC pulpotomy (I) compared to formocresol pulpotomy (C), has comparable clinical and radiographic success rates (O), over 12 months follow up (T).
The null hypothesis is that there is no difference between groups.
Materials and Methods
The study was a single center randomized controlled trial, with an equal allocation ratio between both study arms; TheraCAL LC (Bisco, Inc. Schaumburg IL, USA) and Formocresol (Formacresol, PREVEST DenPro, Digiana, Jammu, India).
The study was designed and reported according to CONSORT statement 2010 and in accordance with the Declaration of Helsinki (1964).
Ethical approval was granted from the Faculty of Dentistry Ain Shams University, Research Ethics Committee institutional under the number of (FDASU-REC D 101612). The study was registered in clinical trial.gov with (NCT04397094) as registration number. Before operative procedures, a signed consent was obtained from parents, and a simplified verbal and illustrated explanation was also given to children to have their assent.
A total sample size of 54 molars was estimated to detect effect size of f=0.59, a power of 95%, and a significant level of 5%11. An additional 10% was added to compensate for possible dropouts, thus a total of 60 primary molars were included. A total of sixty children participated in the study where 60 mandibular second primary molars were randomly divided into TheraCal LC (test group) or formocresol (control group) pulpotomy. The eligibility criteria were [12].
- Four to seven years-old children with at least one restorable mandibular second primary molar having deep caries that displays large carious pulp exposure upon caries removal.
- Asymptomatic, with no pathologic tooth mobility, tenderness to percussion, gingival abscess or fistula.
- No radiographic evidence of pathologic internal or external root resorption, interradicular or priapical bone resorption, or widening of periodontal membrane space.
- At least 2/3 of root length remaining.
- Achievement of radicular pulp hemostasis after five minutes application of cotton pellets moistened with saline.
Using computer generated randomization (www.randome.org), eligible primary molars were randomly allocated to both groups with 1:1 allocation ratio. Each generated number, with its allocated group, was written in a sheet of paper and kept inside a closed opaque envelope.
A department’s nurse opened each envelope at the time of intervention. Only participants and assessors were blinded to the type of treatment.
Intervention
One hundred children were screened over a period of four months (December 2017 till March 2018) until the required number of eligible mandibular 2nd primary molars was achieved, Figure1. The trial ended March 2019.
Infiltration anesthesia with 40mg/ml articaine HCL and 0.005 mg/ml adrenaline (Artinibsa, Inibsa Dental, Barcelona, Spain) was administered.
Under rubber dam isolation, caries removal and access cavity preparation were made using sterile high speed large round bur and coolant.
Coronal pulp tissue was removed by a sterile sharp excavator, and then radicular pulpal hemostasis was attained by gentle application of sterile cotton pellets moistened with saline for five minutes [13].
Teeth were allocated to a treatment group after control of bleeding. If bleeding continued afterwards, pulpectomy was performed and the case was excluded.
TheraCal LC was applied directly to the radicular pulp in 1mm thickness by disposal syringe tip that was also used to manipulate the cement to ensure smooth surface free from air bubbles then light cured for 20 seconds as per the manufacturer protocol.
A cotton pellet moistened with one fifth concentration Buckley’s formocresol (prepared by mixing three parts of glycerin with one part of distilled water then adding four parts of this diluent to one part of formocresol), was placed over the pulp stumps for five minutes [13]. The fixed pulp stumps were capped with zinc oxide eugenol (PrevesTDenPRO, Digiana, Jammu, India). In both groups, pulp chambers were filled with Ketacfil Plus Aplicap(3M ESPE, St Paul, USA ) and stainless steel crowns (3M ESPE, St Paul, USA) were fitted at the same visit and cemented with Ketac-cem (3M ESPE, St Paul, USA) and an immediate postoperative radiograph was obtained.
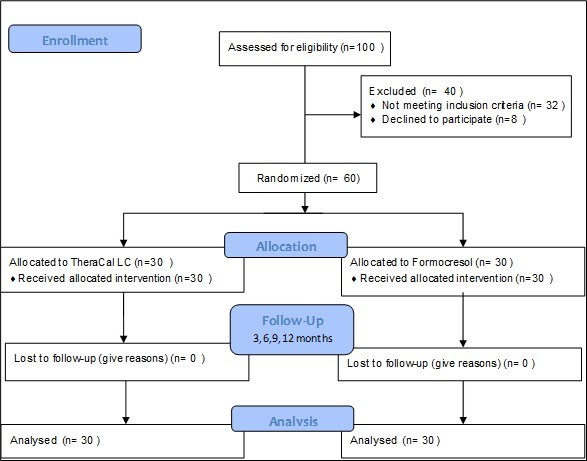
Figure 1: Study Design.
Outcome Assessments
Clinical and radiographic examinations were performed at three, six, nine and 12 months by a single examiner for each assessment type.
The following criteria were considered as clinical failure; restoration loss, spontaneous pain, mobility, gingival swelling, or fistula related to the treated teeth. Internal/external root resorption, inter-radicular or periapical bone resorption, or widening of the periodontal ligament space were considered radiographic failures [13].
All radiographic examinations were taken using a positioning XCP film holder device (Super Bite, Hawe Neos DentalSA, Switzerland), indicated for paralleling technique and an exposure time of 0.25 seconds, using an x-ray machine (X genus DC, de Gotzen, Roma, Italy) at 70 Kvp and 8m, a while wearing a lead apron with thyroid collar. A phosphor plate scanner (Fona-Scaneo, Phosphor Plate Scanner,Germany), and phosphostimulable phosphor plates (Fona- Phosphor Plate size 0, Germany) were used.
The Kappa value for intra-examiner reliability for radiographic evaluation was 0.88.
Data were presented as frequency and percentage values.
Fisher’s Exact test was used at p ≤ 0.05. Statistical analysis was performed with IBM® SPSS® Statistics Version 23 for Windows (SPSS Inc., IBM Corporation, NY, USA).
Results
All participants were available for recall. The mean age in years for TheraCal LC was 5.71 (± 0.59), and 5.56 (± 0.71) for Formocresol. The male to female ratio was 17:13 for TheraCal LC and 15:15 for Formocresol.
No clinical failures were evident in both groups all over the 12 months. Radiographic failures started to appear at nine months where internal resorption was evident in two (6.7%) and three (10%) molars in TheraCal LC and formocresol, respectively and inter-radicular bone resorption was evident in one (3.3%) and two (6.7%) molars in TheraCal LC and formocresol, respectively, table (1) figures (2,3). No new radiographic failures were evident at 12 months.
Table 1: Radiographic Failure at 9 Months.
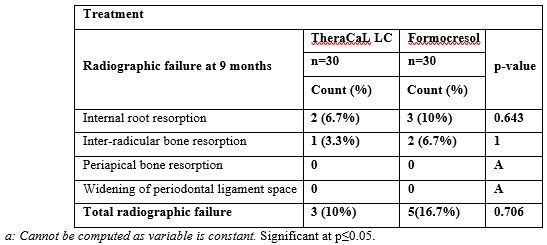
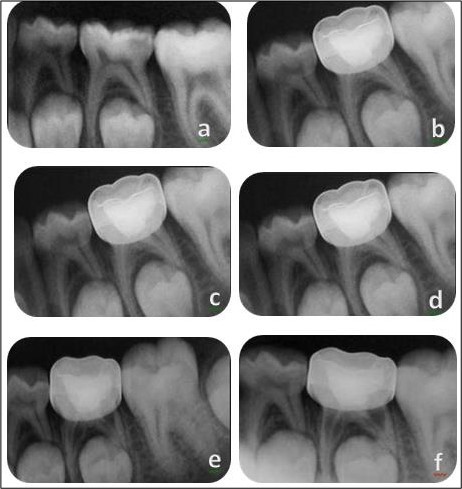
Figure 2: TheraCal pulpotomy; (a): pre-operative, (b): post-operative, (c): 3 months, (d): 6 months, (e): 9 months (note internal root resorption), (f): 12 months.
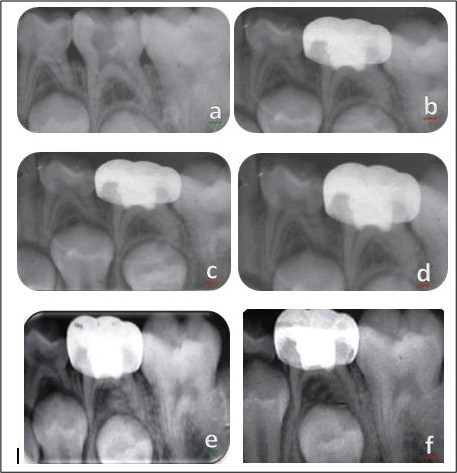
Figure 3: TheraCal pulpotomy; (a): pre-operative, (b): post-operative, (c): 3 months, (d): 6 months, (e): 9 months (note inter-radicular bone resorption), (f): 12 months.
Discussion
The current study was designed to evaluate the efficacy of TheraCal LC in complete pulpotomy of cariously exposed primary molars. TheraCal LC is considered a light-cured MTA like material, but additionally, easy handling and setting on demand are two more advantages compared to MTA [14]. Formocresol application for five minutes is still considered the gold standard for pulpotomy in primary teeth. The diluted concentration was used as a control for it was proved to be equally effective as the full strength but with less toxicity15. Radiographic examination was performed every three months as the only investigation of TheraCal LC pulpotomy at the time of conducting the study reported radiographic failure as early as 3 months following treatment [10].
No clinical failures were evident in both groups at all follow up periods, while radiographic failures started to appear at nine months in both groups. Internal root resorption and inter- radicular bone resorption were the only radiographic failures seen in both groups. These were also the most common radiographic failures reported in the literature [13,15-18]. No significant differences were evident regarding radiographic failures between both groups, so the null hypothesis is accepted.
Radiographic evaluation of both groups revealed insignificant differences. At nine months, formocresol group showed three cases (10%) with internal root resorption and two cases (6.7%) with inter-radicular bone resorption. While two cases (6.7%) in the TheraCal LC group had internal root resorption and one case (3.3%) showed inter-radicular bone resorption. No new radiographic failures were evident at 12 months.
Therefore, radiographic success rates at 12 months were 83.3% and 90% for formocresol and TheraCal LC, respectively.
The clinical and radiographic success rates of the present study falls within previously reported rates for other pulp medicaments after one year which ranged between 73% and 96% [6,10,13,19,20].
A previous investigation of TheraCal LC pulpotomy reported a 100 % clinical and 96.6% radiographic success rates for both TheraCal LC and formocresol at six months. The investigators detected radiographic failures in both groups at three months, with one molar (3.3%) in TheraCal LC demonstrated internal root resorption [10].
Internal root resorption in TheraCal LC could be a result of possible transformation of mesenchymal cells into odontoclastic cells in response to inflammation induced by calcium and hydroxyl release21. Moreover, inter-radicular bone resorption could be attributed to residual monomers that can have a cytotoxic effect on mesenchymal cells22,23. The manufacturer has recommended curing depth of about 1 mm, but complete curing of the material in pulpotomy may be difficult to be achieved. It is worth to mention that a new dual cure product “TheraCal PT “has been recently introduced to the market to overcome such possible side effect. Nevertheless, a histological study of TheraCal LC in human primary teeth revealed pulpal response that was described to be in the direction of pulpal repair. Chronic inflammatory cells with variable degrees, with deposition of multiple osteodentin, dentinoid tissue and calcific foci were seen with absence polymorphonuclear leukocytes indicating absence of acute inflammation. Stimulation of undifferentiated mesenchymal cells to form osteodentin along dentinal walls was noted, though there were areas of disruption in odontoblastic cell layer.
However, in this study, TheraCal LC was placed over radicular pulp stumps for only four months [10].
The inter-radicular bone resorption in formocresol group could be a result of the small molecular size of formaldehydes, which may have leached into the furcation area via accessory canals. Also, in the current study, diluted concentration of formocresol was used.
This concentration may not produce complete mummification of the pulp tissue. This in turn may lead to half-dead, half-vital, and/or chronically inflamed pulp tissue. The resulting pulp can be susceptible to abscess formation [24].
It is worth to mention that failure in pulp therapy may be related to several factors, namely the capping material, technique inconsistency, improper coronal seal or case selection [25,26].
The sole operative selection criterion that decides whether the pulp is inflamed is the time at which hemostasis is controlled. Un-inflamed pulp usually needs no more than five minutes to achieve hemostasis.
However, Mutluay, et al.2018 [ 27] found that the levels of inflammatory cytokines at exposure sites that achieved hemostasis at five minutes or in sites that achieved hemostasis at more than five minutes did not differ significantly, indicating that control of bleeding at carious exposure sites is not a completely reliable criterion to reflect pulp status. Accordingly, insignificant failures seen in vital pulp therapies may be largely a result of misdiagnosis of pulp inflammatory status rather than being related to capping materials, provided that an adequate coronal seal and a standardized technique are employed.
Conclusions
Based on the current results, TheraCal LC can be regarded as a biocompatible alternative to formocresol when a cheaper and an easier technique than MTA is preferred.
However, longer term evaluations may be needed to assess possible late effects of monomers in TheraCal LC on treatment outcomes.
The authors deny any conflicts of interest related to this study.
References
- Fuks AB, Guelmann M. Pulp therapy for the primary dentition. In Dean JA, Jones J, Walker Vinson LQA eds. Dentistry for the child and adolescent, 10th edition, Elsevier Saunders; 2015; pp333-51.
- Lewis B. The obsolescence of formocresol. J Calif Dent Assoc. 2010; 38(2): 102-107.
- Parirokh M, Torabinejad M, Dummer PMH. Mineral trioxide aggregate and other bioactive endodontic cements: an updated overview - part I: vital pulp therapy. Int Endod J. 2018; 51(2): 177‐205.
- Ansari G, Ranjpour M. Mineral trioxide aggregate and formocresol pulpotomy of primary teeth: A 2-year follow-up. Int Endod J 2010; 43(6): 413-418.
- Oliveira TM, Moretti BS, Sakai VT. Clinical, radiographic and histologic analysis of the effects of pulp capping materials used in pulpotomies of human primary teeth. Eur Arch Paediatr Dent 2013; 14(2): 65-71.
- American Academy of Pediatric Dentistry. Use of vital pulp therapies in primary teeth with deep caries lesions. Clinical practice guidelines. 2017; 179-192. http: www.aapd.org/policies. Accessed April 12, 2020.
- Gandolfi M, Siboni F, Prati C. Chemical-physical properties of TheraCal, a novel light-curable MTA-like material for pulp capping. Int End J. 2012; 45(6): 571-579.
- Gurcan AT, Seymen F. Clinical and radiographic evaluation of indirect pulp capping with three different materials: a 2-year follow-up study. Eur J Paediatr Dent .2019; 20(2): 105‐110.
- Erfanparast L, Iranparvar P, Vafaei A. Direct pulp capping in primary molars using a resin-modified Portland cement-based material (TheraCal) compared to MTA with 12-month follow-up: a randomised clinical trial. Eur Arch Paediatr Dent. 2018; 19(3): 197‐203.
- Wassel M, Badran A, Hamdy D. Clinical, radiographic, and histological evaluation of TheraCal pulpotomy in human primary teeth. EDJ. 2017; 63: 365-375.
- Bharti K, Kumar R, Khanna R. Clinical and radiographical evaluation of mineral trioxide aggregate, biodentine and propolis as pulpotomy medicaments in primary teeth. Restor Dent Endod. 2015; 40(4): 276–285.
- Musale PK, Soni AS. Clinical pulpotomy trial of Copaifera Langsdorffii oil resin versus formocresol and white Mineral Trioxide Aggregate in primary teeth. Pediatr Dent .2016; 38(2): 5‐12.
- Ruby JD, Cox CF, Mitchell SC, Makhija S, Chompu-Inwai P, Jackson J A. randomized study of sodium hypochlorite versus formocresol pulpotomy in primary molar teeth. Int J Paediat Dent. 2013; 23(2): 145‐152.
- Arandi NZ, Rabi T. TheraCal LC: From biochemical and bioactive properties to clinical applications. Int J Dent. 2018; 1-6.
- Morawa A, Straffon L, Han S, Corpron R. Clinical evaluation of pulpotomies using dilute formocresol. J Dent Child. 1975; 42: 360–363.
- Vostatek SF, Kanellis MJ, Weber-Gasparoni K, Gregorsok RL. Sodium Hypochlorite pulpotomies in primary teeth: A retrospective assessment. Pediatr Dent. 2011; 33: 327-332.
- Akcay M. The effect of Sodium Hypochlorite application on the success of calcium hydroxide and Mineral Trioxide Aggregate pulpotomies in primary teeth. Pediatr Dent 2014; 36(4): 316-321.
- Casas MJ, Layug MA, Kenny DJ, Johnston DH, Judd PL. Two-year outcome of primary molar ferric sulfate pulpotomy and root canal therapy. Pediatr Dent 2003; 25: 97-102.
- Fuks AB. Vital pulp therapy with new materials for primary teeth: New directions and treatment perspectives. Pediatr Dent. 2008; 3: 211-219.
- Huth KC, Paschos E, Hajek-Al-Khatar N, Hollweck R, Crispin A, Hickel R et al. Effectiveness of 4 pulpotomy techniques--randomized controlled trial. J Dent Res. 2005; 84(12): 1144-1148.
- Ulusoy A, Bayrak S, Bodrumlu E. Clinical and radiological evaluation of calcium sulfate as direct pulp capping material in primary teeth. Eur J Paediatr Dent. 2014; 15(2): 127-131.
- Jeanneau C, Laurent P, Rombouts C, Giraud T, About I. Light-cured tricalcium silicate toxicity to the dental pulp JOE 2017; 43(12): 2074–2080.
- Collado-González M, García-Bernal D, Oñate-Sánchez RE, Ortolani-Seltenerich PS, Álvarez-Muro T, Lozano A, Forner L, et al. Cytotoxicity and bioactivity of various pulpotomy materials on stem cells from human exfoliated primary teeth. Int Endod J. 2017; 50: 19-30.
- Berger JE. Pulp tissue reaction to formocresol and zinc-oxide eugenol. ASDC J Dent Child 1965;32:13-28. Cited from Shashidhar C, Jyothi S. Formocresol, still a controversial material for pulpotomy: A critical literature review. Journal of Restorative Dentistry 2014; 2(3): 114-124.
- Ranly DM, Garcia and Godoy. Reviewing pulp treatment for primary teeth. JADA 1994;122(12):83-87.
- Lin P-Y, Chen H-S, Wang Y-H, Tu Y-K. Primary molar pulpotomy: A systematic review and network meta-analysis. J Dent 2014; 42(12): 1060–1077.
- Mutluay M, Arıkan V, Sarı S, Kısa Ü. Does achievement of hemostasis after pulp exposure provide an accurate assessment of pulp inflammation. Pediatr Dent 2018; 40(1): 37‐42.

