Evaluating the Utility of Fast in Acute Blunt Abdominal Trauma in the Emergency Department: 20 Years On
Hee JS and Lateef F*
1Final Year Medical Student, Yong Loo Lin School of medicine, National University of Singapore, Singapore
2Senior Consultant/ Director of Training and Education, Department of Emergency Medicine, Singapore General Hospital; Professor, Dukes-NUS Graduate Medical School and Yong Loo Lin School of Medicine, National University of Singapore; Director, Sing health Duke NUS Institute of Medical Simulation, Singapore
Received Date: 10/09/2020; Published Date: 20/11/2020
*Corresponding author: Fatimah Lateef, Senior Consultant/ Director of Training and Education, Department of Emergency Medicine, Singapore General Hospital; Professor, Dukes-NUS Graduate Medical School and Yong Loo Lin School of Medicine, National University of Singapore; Director, Singhealth Duke NUS Institute of Medical Simulation, Singapore. E-mail: fatimah.abd.lateef@sgh.com.sg
Abstract
Introduction: Blunt abdominal trauma (BAT) is a common presentation in the Emergency Department (ED) and associated with high mortality and morbidity. Given the time-sensitive nature, it is necessary to evaluate if FAST possesses adequate sensitivity and specificity to confidently rule out life-threatening injuries and guide the course of management. A positive FAST result would indicate intra-abdominal injury and prompt urgent surgical intervention, particularly in hypotensive patients. This review aims to examine relevant literature to evaluate the diagnostic utility and outcomes of FAST, and important external factors to be considered.
Methodology: Keyword search of PubMed and the Cochrane Library yielded 514 articles, from which 61 studies were chosen based on the inclusion and exclusion criteria.
Results: FAST demonstrates low to moderate sensitivity and Negative Predictive Value (NPV) and high specificity and Positive Predictive Value (PPV) in detection of hemoperitoneum and associated intra-abdominal injuries. Sensitivity for detecting peritoneal fluid is the highest. While superior to DPL, it has yet to surpass the diagnostic utility and accuracy of CT.
Conclusion: FAST is essential and should remain the primary preliminary radiological assessment of acute BAT. A positive FAST is highly predictive of intra-abdominal injury but a negative FAST cannot accurately rule out intra-abdominal injury. Negative FAST results should be succeeded by continued clinical observation, and serial FAST examinations or CT-scan should clinical signs not correlate. Current literature offers no evidence that FAST should replace CT as the diagnostic standard for BAT or a definitive ability to determine the necessity of immediate surgical management.
Keywords: Focused Assessment for Sonography; FAST; E-FAST; Ultrasonography; Point Of Care Ultrasound; Pocus; Blunt Abdominal Trauma; Laparotomy and CT
Introduction
Abdominal trauma is a common presentation in the ED and also one of the leading causes of death in young adults, under 45 years. It can be broadly classified into high or low energy injuries, and blunt or penetrating abdominal trauma. Blunt abdominal trauma (BAT), may be the result of road traffic accidents, physical assault or falls from height. Penetrating injuries are generally caused by firearms and stabbings. The focus of this review will be blunt abdominal trauma, as it is by far the more common presentation. A study was conducted by The Western Trauma Association Multi-Centre Trials of 392,315 blunt trauma patients at 12 major trauma centres. Majority of the injuries were caused by motor vehicle collisions (60%). 47% of the patients had documented hypotension and solid organ, small bowel, and large bowel injuries occurred in 38%, 35%, and 28% respectively. The most commonly associated injuries were spine fractures (44%) and pneumothorax/haemothorax (42%) [1].
Up to 50% of patients with severe abdominal trauma and/or multiple distracting injuries are reported to either have a normal initial abdominal exam, or are obtund and unable to provide a reliable index of suspicion. This affects both the physical and imaging examinations [2]. Diagnostic errors are responsible for approximately 10%–15% of preventable deaths in trauma centre audits. The sole reliance on clinical assessment as the main indication for surgery has led to negative laparotomy rates of as high as 40% [3]. A retrospective analysis found the incidence of short‐term complications caused by negative laparotomy to be 43% [4].
A quick, effective and efficient imaging approach is necessary to exclude life-threatening injuries. This modality would preferably need to have high sensitivity and specificity [5]. Prior to FAST, Diagnostic Peritoneal Lavage (DPL) was the standard initial diagnostic investigation. Although an invasive test, it could be done rapidly and was relatively safe with high sensitivity but had a significant false‐positive rate, which potentially exposed patients to the risks of an unnecessary laparotomy [6]. All patients who sustain blunt trauma to below the nipple line, are assumed to have intra-abdominal injuries until proven otherwise. Prompt reliable diagnosis and characterization of the abdominal injuries is essential to reduce risk of mortality and morbidity. Hemodynamic instability is a high-risk clinical sign and as such, both the diagnostic and interventional thresholds for these patients should be lowered. The three main types of blunt abdominal trauma injuries are solid organ injury, hollow viscos/mesenteric injury and vascular injury. The most commonly injured intra-abdominal organ is the spleen, followed by the liver and the genitourinary tract [7].
Immediate laparotomy should be done for patients with signs of peritoneal irritation, fresh blood on rectal exam, fresh blood aspirated from nasogastric tube, stab wounds with implement in-situ, gunshot wounds traversing the abdominal cavity, suspected intra-abdominal injury with hemodynamic instability, ultrasound evidence of active haemorrhage, and X-ray evidence of pneumoperitoneum or diaphragmatic rupture. In a retrospective cohort study of consecutive normotensive blunt trauma patients at 2 trauma centres, there was a strong association between a positive FAST and the need for therapeutic laparotomy. (Adjusted OR 44.6, 95% CI 1.77–1124). Thirty-seven percent of patients with a positive FAST required therapeutic laparotomy vs. 0.5% with a negative FAST [8]. Another study quoted lower figures, where only 25% of patients with intra-abdominal fluid required laparotomy [9].
Imaging modalities most often used to evaluate abdominal trauma in the ED are the Focused Assessment for Sonography for Trauma (FAST) and the Computed Tomography scan (CT-scan) which is the current reference diagnostic gold standard. The purpose of this study is to present a systematic review on the utility of the primary first line imaging modality FAST, in the acute assessment of blunt abdominal trauma.
Methodology
A systematic review of the literature was achieved using the electronic database PubMed and the Cochrane Library. Various query terms were tested to obtain enough data and to avoid unspecific information. Duration of search was from 1stMarch 2020 to 1stApril 2020. There was no limit on geography, age, type of study or date of article. Only original studies published in English were considered for this review. Keyword search yielded 514 articles, from which 61 studies were chosen based on the inclusion and exclusion criteria.
The keywords used in the search include: Focused Assessment for Sonography, FAST, E-FAST, Ultrasonography, Point of Care Ultrasound, PoCUS, Blunt abdominal trauma, Laparotomy and Computed tomography, CT
For studies to be included in this study, the inclusion criteria are as follows:
- Acute presentation of blunt abdominal trauma at the ED
- PoCUS/FAST or E-FAST examination done performed by radiologists, non‐radiologist clinicians, or ultrasound technicians
- Definitive diagnosis verified by CT-scan or operative diagnosis.
- Sufficient information on diagnostic test accuracy (i.e. sensitivity, specificity)
The studies were excluded if:
- Insufficient information on diagnostic test accuracy
- Case reports, case series
- Unclear index or reference tests
- Diagnostic case-control studies that compared patients with known case status to healthy controls. (This creates artificial populations and tends to overestimate sensitivity of the index test)
- Patients with penetrating abdominal injuries
Results
Focused Assessment for Sonography for Trauma (FAST)
Ultrasound based trauma algorithms were only introduced formally into trauma literature in 1996.FAST is a limited abdominal ultrasound modality used in acute trauma as part of Advanced Trauma Life Support (ATLS)protocol to identify intra-abdominal fluid collections using a 3.5Hz sector transducer. FAST was established in 1999 after the FAST consensus conference and a subsequent study done at Massachusetts General Hospital in Boston, USA, showed the number of FAST scans increased from 15 % to approximately 34 % in the period 2002–2011, while the number of abdominal CT scans decreased from 35 % to 14 % in the same period [10]. In a prospective study on influence of FAST on trauma management, 194 patients underwent FAST. It was shown that FAST prevented an unnecessary laparotomy in 1 patient, CT in 23 patients, and DPL in 15 patients. There was an overall reduction in CT requests (from 47% to 34%) and DPL requests (from 9% to 1%) (p < 0.0001) [11].The goal of FAST is to detect hemoperitoneum in the right and left sub phrenic space, peri-splenic fossa, hepatorenal recess, suprapubic window (Pouch of Douglas or rectovesical pouch) and hemopericardium in the subxiphoid space. A positive FAST result would mean that there is free fluid in either of these abdominal compartments, which is a surrogate for active haemorrhage and in one study, has demonstrated a 65% sensitivity in detection of abdominal injuries requiring surgery [12].
E-FAST and Ex-FAST
E-FAST was established in 2004 and is now the diagnostic standard of ATLS, virtually replacing DPL. The E component refers to bilateral anterior thoracic sonography which searches for free air in the pleural cavity as evidence of an acute traumatic pneumothorax. It has been shown to have greater sensitivity and specificity than traditional chest radiography [13]. There is also some reference to Extended FAST or Ex-FAST. It is a combination of both physical examination and FAST. An abnormal examination constitutes signs of hemodynamic instability, abdominal bruising, tenderness, absence of bowl sounds, peritonism, seatbelt sign, lacerations etc. [14]. In a retrospective study of 354 children in the ED of which 14% (n=50) had intrabdominal injury (IAI), the use of Ex-FAST showed greater sensitivity (sensitivity of 88% (95% CI: 76‐96%) and Negative Predictive Value (NPV) 97.3% (95% CI: 94.5‐98.7%)) over either physical examination [OR, 15.2; 95% CI: 7.7 ‐ 31.7] or FAST [OR, 14.8; 95% CI: 7.5 ‐ 30.8] alone [15].
The execution time of E-FAST examination averaged 2.3 ± 2.9 min for chest US and ≤5 min for standard FAST [16]. FAST has been reported to be able to detect as little as 200ml of fluid in Morrison’s pouch and can completed in less than a minute in the hands of an experienced operator. This is many times faster than a CT-scan which on average takes approximately 30minutes and hence unsuitable for an unstable patient in an emergent setting. Moreover, it is easily repeatable, physicians can be easily trained, inexpensive, non-invasive and does not require contrast nor exposes the patient to ionizing radiation. Although these are insufficiently substantiated by sufficient evidence, other possible beneficial outcomes include shortening of the primary trauma assessment, more precise triaging, avoidance of unnecessary interventional procedures, and associated costs
The reliability and quality of images obtained from FAST is also greatly dependent on the training and experience of its operator. A comparison of the reproducibility of FAST results between Emergency Medicine Residents (EMRs) and Radiology Residents (RRs) showed sensitivities, specificities, PPV, NPV and accuracy of evaluating intra-peritoneal fluid to be very similar at 80%, 95%, 57%, 98% and 94% and 86%, 95%, 59%, 98% and 94%. This shows that EMRs are well-trained to use FAST and their results would be similar if not identical to an RR [17]. However, a comparism done in another study amongst US operators with low, moderate and extensive experience reported sensitivities of 45%, 87%, and 100% respectively in detecting <1L of peritoneal fluid [18].
A recent review article has quoted FAST sensitivities that range between 63 % and 99 % and specificities range from 90% to 100%. These results are similar for the detection of free intraperitoneal fluid, with sensitivities ranging from 69 % to 98 % and specificities of 94% to 100% [19]. Another study reviewing literature from various institutions around the world has reported lower thresholds of sensitivities ranging from 42.0%–91.7%, specificities 83%–100% and accuracies 9%–96% for the utility of E-FAST examinations. Its own prospective observational study examining the diagnostic accuracy of E-FAST done by emergency physicians compared to CT at the ED of a level 1 trauma centre found that out of 132 patients with blunt abdominal trauma, FAST sensitivities (only abdomen) was 42.9% (95% CI: 9.9%, 81.6%) and specificity was 98.4% (95% CI: 94.3%, 99.8%). The + LR of the FAST exam for abdominal free fluid as 26.8 (95% CI: 5.3, 135.2) and − LR was 0.58 (95% CI: 0.31, 1.1) [20]. This consistently high reported specificity of FAST was highlighted in a systemic review of 11 articles containing prospectively derived data with FAST results, patient disposition and final diagnoses. It showed that out of the 2,755 patients, 448 (16%) went to the OR. In total, there were 5 false-negatives derived from FAST; 3 involving inadequate scans and 2 of blunt trauma-induced small bowel perforations without hemoperitoneum [21]. The sensitivity of an examination is the “correct positive test rate” and measures the proportion of patients with an intraabdominal injury who have a positive test result. A high degree of sensitivity is not useful to rule in a diagnosis, but rather to rule out a particular condition. Similarly, high levels of specificity indicate that positive findings will detect the presence of a pathology. This suggests that when FAST is positive, there is high certainty of injury but when it is negative there’s a higher chance the injury was undetected. Hence, there is still large uncertainty in diagnostic confidence, with its wide sensitivity range and cannot confidently or safely exclude the presence of intra-abdominal injury.
FAST in Abdominal Trauma
In a meta-analysis [22] of emergency ultrasonography for BAT, a sensitivity range was observed as low as 28% and as high as 97%, specificities were close to 100%. A summary measure of 0.90 was calculated for the sensitivity-specificity pair closest to the desirable upper left corner of the ROC curve, which could be interpreted as 10% of abdominal injuries will be missed by FAST. Low sensitivities, coupled with low NPV, negative LRs and associated post-test probability, diminishes confidence in negative FAST findings. However, high specificities and LRs>10 would almost confirm intra-abdominal injury if positive and hence the need for surgical management.
In a retrospective study, 3181 blunt normotensive trauma patients presenting at a single level 1 trauma centre were evaluated with FAST and stratified into various groups of Injury Severity Scores (ISS). A one-time, four-view FAST examination in patients with ISS ≥ 25 had a lower sensitivity of 65 % than those with an ISS < 25 (80–86 %). More than 82 % of the FAST-missed injuries in patients with ≥ 25 ISS were solid organ injuries of the liver, spleen and kidneys [23]. An observational study of the diagnostic accuracy of FAST in 105 patients from King Fahad Military Medical Complex Dhahran, Saudi Arabia with blunt abdominal trauma demonstrated sensitivities of 76.1% (95% CI, 64.14- 85.69%), specificity 84.2% (95% CI, 68.75- 93.98%) and accuracy 79% (95% CI, 70.01- 86.38%. FAST could detect free fluid in 37 out of 39 patients with high grade sold intra-abdominal injuries. However, it could not detect small amount of fluid and nearly half of the negatives had low grade visceral injuries [24]. These studies highlight potential factors that may affect the results of the FAST examination, such as the presence of multiple other distracting injuries, higher likelihood for missed solid organ injuries and reduced sensitivity for fluid in patients with only low-grade injuries.The reason for this could be that hemoperitoneum is not always seen in liver or splenic injuries and hence it doesn’t matter if FAST has a high sensitivity for peritoneal fluid [12].
A systemic review evaluating the diagnostic accuracy of point‐of‐care sonography (POCS) for diagnosing thoracoabdominal injuries in patients with blunt trauma included 34 studies with a cumulative cohort of 8635 participants. For abdominal trauma, POCS had a sensitivity of 0.68 (95% CI 0.59 to 0.75) and a specificity of 0.95 (95% CI 0.92 to 0.97), with statistically significant lower values in children. To put this in perspective, it meant 73 false negatives and 29 false positives for every 1000 adult patients, assuming the observed median prevalence of thoracoabdominal trauma of 28% [25].
In paediatric BAT patients, the diagnostic accuracy of FAST has been reported to be lower compared to adults. A multi-institutional (n=14) analysis of level1 paediatric trauma centres yielded low sensitivities (28%) and high specificities (91%) for IAI consistent with paediatric literature but improved sensitivities (44%) and similar specificities (89%) for IAI requiring acute intervention. However, FAST missed 75% of liver injuries and 57% of spleen injuries and 56% of 27 patients whom required acute intervention for IAI had negative FAST. All the patients were normotensive and had abnormal abdominal examination [26]. However, in a separate observational prospective study comparing FAST evaluation of hypotensive and normotensive children with BAT, FAST showed a 100% sensitivity in detecting peritoneal fluid in hypotensive patients [27]. A prospective study was done on 160 hemodynamically stable paediatric trauma patients who had undergone both FAST and CT. Forty-four of the 160 patients had an intraabdominal injury on CT, 24 (55%) of which had normal screening sonography. Accuracy of sonography compared with CT was 76% with a negative predictive value 81% [28]. While the statistics of these three studies on the use of FAST in paediatric BAT patients do vary, sensitivities and specificities are both generally on the lower threshold of the adult range. They also show consistency of hypotension as a strong predictor of IAI and the poor ability of FAST to detect solid organ injuries.
FAST and Other Modalities
A prospective study [16] was done of 601 adult trauma patients at the ED who underwent a Chest Abdominal-Focused Assessment Sonography for Trauma (CA-FAST) exam prior to a thoracoabdominal CECT. Free fluid was detected in 116 patients with an overall accuracy of 91 % (95 % CI 85–93%). The following table illustrates the results of 4-view FAST and its individual views
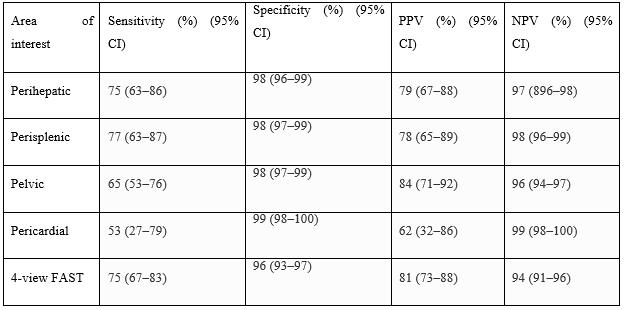
FAST has different sensitivities for each abdominal cavity view, which translates to different diagnostic accuracies for the various types injuries previously mentioned in the methodology has well. In this study, FAST exhibits moderate to good sensitivity than previously quoted and with similar sensitive for the upper abdominal regions, followed by the pelvis and least able to detect fluid in the subxiphoid, pericardial space. It also shows good PPV, high specificity and NPV, consistent with previous studies [16].
This is supported by a 2-year review at a level1 trauma centre of 1027 patients who underwent FAST were stratified by operator skill level. It was shown that compared to patients with concordant FAST results, those with equivocal results had higher mortality (9.8 vs 3.7%, P = 0.02), decreased positive predictive value in the right upper quadrant (RUQ) (55 vs 79%, P = 0.02) and left upper quadrant (LUQ) (50 vs 83%, P < 0.01). However, unlike the previous study, this study observed worse outcomes has a result of the high rate of false negatives in the FAST examination.
However, some of these findings were obtained from only a single FAST scan (i.e. [23]), with the underlying assumption that fluid accumulates in the deepest parts of the abdomen. This can be influenced by anatomy, location of bleed, respiratory physiology, intra-abdominal adhesions etc. Thus, it would be prudent to consider the value of serial FAST scans, Contrast Enhanced Ultrasonography (CEUS), additional abdominal views and other imaging modalities such as CT with or without contrast media. A retrospective analysis [29] comparing the use of CTAP and Complete Ultrasonography of Trauma (CUST) in 19128 patients to screen for blunt abdominal trauma (BAT) from 2000 to 2011 in a Level 1 trauma centre was performed. It found that outcomes in CUST is equivalent to routine CTAP for BAT and leads to an average of 42% less radiation exposure and more than $591,000 savings per year.
The shortcomings of FAST can be bolstered by the application of CEUS. A recent meta-analysis [30] of 9 studies investigating the diagnostic accuracy of CEUS of abdominal trauma patients at the ED demonstrated that the CEUS had a sensitivity of 0.981 (95% CI: 0.868-0.950) and a false positive rate of 0.018 (95% CI: 0.010-0.032) for identifying parenchymal injuries, with an AUC of 0.984. These accuracies are similar to that of contrast-enhanced CT. Another study done on the application of CEUS in paediatric patients concluded CEUS proved to be an effective investigation in the hemodynamically stable child for identifying parenchymal injuries and for the characterization of focal liver lesions. It also showed comparable performance to CT and MRI with a specificity of 98% for identifying benign lesions and a negative predictive value of 100% [31]. However, the need for contrast in identifying intra-abdominal injury may not always be relevant in contributing diagnostic value. It can add confidence in cases of interpretation doubts or diagnostic difficulties, but some studies have shown CEUS to have similar sensitivities to baseline US [32].
Splenic injuries are the most common intra-abdominal injury followed the liver in the setting of acute blunt abdominal trauma. CEUS has been shown to be able to overcome the lower sensitive of FAST in detection of traumatic injuries with the reference standard as CT, to reach almost similar levels of accuracies. Evaluation of severity of splenic injuries is particularly important in the decision for surgical management as the spleen should be preserved if possible, due to the dual immunological and haematological functions [33]. However, a retrospective cohort study [34] at a level 1 trauma centre of 332 patients found that patients with spleen, liver, or abdominal vascular injuries were less likely to have false-negative FAST examination results (OR 0.3; 95% CI 0.1 to 0.5). Surprisingly, false-negative FAST results were not associated with increased mortality (OR 0.89; 95% CI 0.42 to 1.9) and these patients were fortunately also less likely to require therapeutic laparotomy. (OR 0.31; 95% CI 0.19 to 0.52).This at first glance may seem puzzling compared to previous studies; however, this is consistent with the generally high specificities of FAST and its lower sensitivities for solid organ injury and lower grade injuries which naturally may be less likely to require surgical intervention or carry a high mortality rate.
Computed Tomography and Abdominal Injuries
Computed Tomography is superior to FAST in evaluating solid organ, hollow vicus, mesenteric injuries and active haemorrhage. However, it has disadvantages such as radiation exposure, risk of contrast nephropathy or allergy, high cost, limited availability, requires more time and the potential need for sedation in paediatric patients. A level 1 trauma canter in the USA reported the radiation exposure of patients with a median ISS of 14 within the first 24 hours at a median of about 40 mSv. The lifelong risk of dying from a carcinoma is assumed to increase by about 0.1 % per 10 mSV. This risk also depends on gender, age and radiation location [19]. Although this is a minute amount, we can conclude that CT scans should be avoided when possible as it does expose the patient to a significant amount of radiation, enough cause a measurable increase in cancer risk.
A recent retrospective analysis evaluated the diagnostic performance of CT for detection of hollow vicus injury (HVI) in patients presenting with penetrating abdominal trauma at a level 1 Nordic trauma centre. Out of the 636 patients with penetrating abdominal trauma, 155 (85%) had a CT-scan on arrival, of which 41 (30%) subsequently underwent emergent surgery. Surgery revealed only 26 (63%) has HVI, showing that CT had 69.2% sensitivity and 90.5% specificity in detecting HVI [35].
Although FAST showed high accuracy for peritoneal fluid, it’s non-specific for solid organ injuries and prevalence of organ injury without accompanying free fluid can range from 5% to 37% [36]. It also lacks sensitivity for hollow viscos and mesenteric injuries, which not are only the most commonly missed but also associated with high morbidity and mortality and has a higher likelihood for requirement of surgical intervention than solid organ injuries. A retrospective study done on 32 patients showed that MDCT could diagnose bowel injury in all of the patients except one. The minor signs showed a higher sensitivity than the major signs [3]. This suggests a sensitivity for bowel injury much greater than FAST which was 12.5% amongst 4 patients and 37.4% in another study [36]. Other studies have also quoted high sensitivities (94%) and PPV (92%) for CT in detecting bowel injury [37]. A meta-analysis [38] of articles concerning the incidence and significance of free intra-abdominal fluid on CT scan of blunt trauma patients without solid organ injury concluded that isolated finding of free intra-abdominal fluid on CT scan in patients with blunt trauma and no solid organ injury does not warrant laparotomy. Instead, its aetiology should be evaluated and other CT signs of GI perforation should be searched for. Small bowel injury had the highest incidence of positive free fluid without evidence of solid injury, but the combination of both pneumoperitoneum and free fluid increased the sensitivity of detection of small bowel injury [3].
When compared with its predecessor DPL, it showed significant advantage in its pre-test probabilities with a positive LR of 10.83 (95% CI 6.45 ± 18.17) and a negative LR of 0.11 (95% C.I. 0.06 ± 0.21). When compared to CT, FAST still had a positive LR 11´42 (95% C.I. 8.01 ± 16.29)) in confirming presence of intra-abdominal injuries, but it was still below acceptable thresholds in safely excluding abdominal injuries (negative LR 0.21 (95% C.I. 0.16 ± 0.29)), which is essentially the gold for immediate trauma management. Hence FAST is unable to be the diagnostic standard for obtaining a definite diagnosis [22].
Whole body CT (WBCT) is the gold standard for trauma imaging, however it is usually only supported by highly specialised trauma centres with the appropriate infrastructure. A clinical review highlighted observational data that suggested WBCT was associated with decreased mortality and time required for trauma evaluation [39]. On the other hand, randomized controlled data from the REACT-2 trial [40] suggests no mortality benefit to this diagnostic tool. There is no clear evidence or sufficient data to prove that CT should be the first line imaging modality in acute blunt abdominal trauma. As we simply lack the resources and time to conduct CT for every patient, not to mention the higher costs and having to subject every patient to ionizing radiation, the decision for CT should remain on a case to case basis. Decision making should be based on a combination of history, physical examination, clinical signs and other imaging modalities i.e. FAST/X-ray. More studies (i.e. RCTs) will have to be done to assess its outcomes over FAST in the emergency setting of BAT and its utility in assessing need for surgical intervention.
A study [41] assessed CT scans of paediatric patients with abdominal trauma for presence, location, and severity of intraabdominal injury, and amount of peritoneal fluid. It was found that only 17% of the 1,486 children had peritoneal fluid demonstrated by CT but 80% had concomitant intraabdominal injury. This suggests that although presence of peritoneal fluid is a strong indicator of intra-abdominal injury, it can be present without, with solid organ injury being the most frequent (68%). Furthermore, it may also indicate that like FAST, CT may have reduced sensitivity in picking up intra-abdominal injuries without peritoneal fluid. CEUS may be applicable for the 37% of patients with intra-abdominal injuries picked up by CT but no peritoneal fluid was detected.
Discussion
In the emergency department today, E-FAST is still the diagnostic standard for ATLS in the event acute abdominal trauma. Its findings, combined with history taking, physical examination and other imaging modalities (i.e. chest/abdominal radiography) would then determine the need for a CT-scan or emergent surgical intervention (i.e. laparotomy). Training with learning objectives and the duration as well as supervision should be standardized with the help of existing scientific principles. FAST demonstrates low to moderate sensitivity and high specificity as a single examination. There have been no studies that examined the utility of serial FAST examination. This is dependent on several factors such as, the time elapsed since trauma, type and extent of injury, patient group (i.e. age, BMI), quality of ultrasound machine, and skills of the FAST examiner. It was also mentioned previously that FAST results are also made on the assumption that fluid tracks to the most gravity dependant parts of the abdomen, and can be influenced by anatomy, location of bleed, respiratory physiology, intra-abdominal adhesions etc. However, it was seen in many studies that many patients who tested negative on FAST did have intra-abdominal injuries subsequently detected on CT or intra-operatively.
To improve sensitivity, the three standard abdominal FAST views should be supplemented by six further sections: sub diaphragmatic, caudal liver margin, parabolic groove, between intestinal loops, retroperitoneal and right upper abdomen view for the detection of free air. The examination should also include visualisation of solid organs such as spleen, liver, and kidneys to assess for injury. Serial exams can also be done at 12hourly intervals to reduce the likelihood of false negatives and reconfirm earlier findings. The effectiveness of serial FAST examinations in patients of deteriorating clinical status was demonstrated in a study that showed a 50% decrease in false-negative rates by 50% and an 85% increase in sensitivity for free fluid detection. The sensitivity and NPV for injury detection increased to 71% and 97%, respectively [42]. These aforementioned strategies can be investigated further through the conducting of randomized controlled trials. Diagnostic errors owing to human error can also be reduced through a more systematic approach such a diagnostic checklist, or management of physician fatigue. Albanese et al. also believed that serial physical examinations are the gold standard for diagnosing GI perforation from blunt abdominal trauma [43].
FAST does offer greater insight than solely relying on clinical signs but it is unsuitable to obtain a diagnosis with sufficient certainty nor can a negative result safely exclude intra-abdominal injury? Possible reasons for poorer accuracy could be that it was in the early post-injury phase, where sufficient hemoperitoneum had not yet accumulated thus leading to false-negative results. FAST has also shown poor sensitivity to identify hollow viscos or solid organ injuries not associated with hemoperitoneum such as early bowel injury or pancreatic injury and limited utility in detecting retroperitoneal haemorrhage. Other potential sources of error include obesity and subcutaneous fat, body habitus and positioning, ascites due to pre-existing medical condition, pre-existing pericardial effusion, and the presence of intra-abdominal cysts or masses [44]. Patients with these characteristics should be evaluated with a subsequent CT-scan if hemodynamically stable.
A comparative study [45] evaluating the use of FAST was done on 706 patients with blunt abdominal trauma. 460 patients were managed with FAST and 246 without FAST. Respectively, both groups showed similar accuracies at 99.1% and 98.0% respectively, and frequency of laparotomies at 13.5% and 14.2%. FAST patients also had a lower mean diagnostic cost and lower mean time required for diagnostic work up. In the FAST group, the computed tomographic rate was 24%, whereas it was 91% in the no-FAST group. As previously established, it’s been shown in many studies that FAST greatly reduced the need for CT-scans, a recent review quoting rates as high as 50%. Although there are surprisingly no significant differences in mortality or laparotomy rates. These two studies show that FAST is cheaper, fast, decreases the length of hospital stay, duration to definitive treatment, and use of healthcare resources [6]. However, it does not actually improve accuracies nor change the management or treatment outcomes of BAT.
Nevertheless, it is shown that peritoneal fluid if present, is highly sensitive to intra-abdominal injury, specifically active haemorrhage which is an indication for emergent laparotomy. This can not only save crucial time in achieving haemostasis instead of waiting for the results of the CT-scan, but is more accurate than DPL which is invasive, or simply clinical signs alone. Moreover, E-FAST is far superior to chest X-ray in terms of detecting haemothorax and pneumothorax and is the only simple bedside method for detecting hemopericardium. Thus, the purpose of E-FAST is for rapid assessment of intra-abdominal that require immediate surgical intervention, especially if the patient is hypotensive, and/or to evaluate the need for a CT-scan. FAST should not replace the abdominal examination or history taking nor be the sole modality replacing CT, for evaluation of abdominal trauma, particularly in patients with abdominal pain, contusions or altered mental status as it’s been shown to intra-abdominal injury can be present even without peritoneal fluid. While CT should not replace FAST either as the 1st line imaging modalities in BAT, a high index of suspicion and low threshold is required. Also, FAST does reduce the frequency of need for CT-scans in the ED and hence the overall costs and radiation exposure to the patient, along with more efficient use of hospital resources. If a new diagnostic algorithm is faster and less expensive it must also be as safe and accurate as the conventional diagnostic algorithm before it can become the new standard of care. Given the current level of evidence we have today, we can conclude that CT should still remain the gold standard for definitive evaluation of blunt abdominal trauma and guide its subsequent management.
Although CT does have greater diagnostic accuracy compared to FAST and is still the gold standard for definitive abdominal trauma imaging, there are little studies done to evaluate the outcomes of patients who have had a CT-scan done without E-FAST. It is established that CT-scan does carry significantly greater number of risks compared to FAST, including requiring more time which the hypotensive patient may not be able to afford. CEUS FAST has showed higher accuracies than conventional FAST in detecting liver, spleen, or kidney injury and active bleeding, similar to that of CT in children and adults with BAT. However, larger randomized trials to evaluated diagnostic accuracy and outcomes will be required to further validate its clinical use as the standard of care [19]. Assuming that major blunt abdominal or multiple trauma is associated with 15% mortality and a CT‐based diagnostic work‐up is considered the current standard of care, 874, 3495, or 21,838 patients are needed per intervention group to demonstrate non‐inferiority of FAST to CT‐based algorithms with non‐inferiority margins of 5%, 2.5%, and 1%, power of 90%, and a type‐I error alpha of 5% [6].
However, studies have shown that despite steady improvement of sonographic resolution properties over the past 20 years, diagnostic precision has not significantly improved, which may suggest that ultrasonography in the emergent setting and the experienced gain may have already reached its limit [22]. Technological advances have allowed recent development of wireless probes [46] and devices capable of short- and long-distance image transmission to remote displays. As ultrasound technology continues to evolve, we expect to see further miniaturization, better image quality and even holography or wearable technology [47]. The FAST exam is easily learned and educational materials are abundant both online (images and video) and in print. As both FAST and E-FAST increase in popularity, implementation of robust educational programs will become increasingly important so that future generations of practitioners are able to acquire high quality sonographic images, interpret those images, and also make real-time clinical decisions based on that information. Trauma centres can look into optimizing infrastructure and trauma protocols to shorten the time required for CT-scan, which has been reported in some studies to be as quick as only a few minutes. It is also crucial to emphasize integration of various sources of information and not to rely solely on a single modality.
Conclusion
FAST is an essential tool for preliminary assessment of intra-abdominal injury, including BAT. A FAST result if positive, in highly confirmative of intra-abdominal injury, for which emergent surgical management is indicated. However, a negative FAST cannot with sufficient diagnostic confidence, rule out intra-abdominal injury. The results of FAST should be considered in conjunction with clinical signs and relevant patient information. Patients with a negative FAST result should continue to be observed clinically, evaluated with serial FAST examinations or CT-scan should intra-abdominal injury be suspected. Developing technologies in Ultrasonography yield promising improvements to the FAST examination but current literature offers no evidence that FAST should replace CT as the diagnostic standard for BAT or its ability to definitively determine the necessity of immediate surgical management.
Assessment of Heterogeneity
It is acknowledged that there is strong heterogeneity amongst the data pooled in these studies across demographics, treatment protocols, measures and types of outcomes etc. and this heterogeneity of finding should be taken into account when reading this article. FAST unfortunately is a form of technology victim to the paradox of the Buxton’s law, that it is unable to be subject to rigorous testing prior to application until it has been widely adopted and used for a long time. Given the nature of FAST application, it is likely that it will never be tested under conditions of an RCT and if possible, requires one of staggering magnitude as earlier discussed. Hence it is important to include all qualitative and quantitative evidence available for such a widely used diagnostic tool.
Declaration of Conflict of Interest
The authors have no conflict of interest to declare.
References:
- Shalhub S1, Starnes BW, Brenner ML, Biffl WL, Azizzadeh A, Inaba K et al. Blunt abdominal aortic injury: a Western Trauma Association multicenter study. J Trauma Acute Care Surg. 2014;77(6):879-85.
- Schurink GW1, Bode PJ, van Luijt PA, van Vugt AB. The value of physical examination in the diagnosis of patients with blunt abdominal trauma: a retrospective study. Injury. 1997 May;28(4):261-5.
- Sarita Magu, Shalini Agarwal, Ravinder Singh Gill. Multi Detector Computed Tomography in the Diagnosis of Bowel Injury. Indian J Surg. 2012 Dec; 74(6): 445–450.
- Morrison JE, Wisner DH, Bodai BI. Complications after negative laparotomy for trauma: long-term follow-up in a health maintenance organization.J Trauma. 1996 Sep;41(3):509-13.
- Hamid S, Nicolaou S, Khosa F, Andrews G, Murray N, Abdellatif W. et al. Dual-Energy CT: A Paradigm Shift in Acute Traumatic Abdomen. Can Assoc Radiol J. 2020 Mar 11:846537120905301.
- Stengel D, Rademacher G, Ekkernkamp A, Güthoff C, Mutze S. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database Syst Rev. 2015 Sep 14;(9):CD004446.
- Soto JA, Anderson SW. Multidetector CT of blunt abdominal trauma. Radiology. 2012 Dec;265(3):678-93.
- Moylan M, Newgard CD, Ma OJ, Sabbaj A, Rogers T, Douglass R. Association between a positive ED FAST examination and therapeutic laparotomy in normotensive blunt trauma patients. J Emerg Med. 2007 Oct;33(3):265-71.
- Como JJ, Bokhari F, Chiu WC, Duane TM, Holevar MR, Tandoh MA, Ivatury RR, Scalea TM. Practice management guidelines for selective nonoperative management of penetrating abdominal trauma. J Trauma. 2010 Mar;68(3):721-33.
- Alexander Y. Sheng, Peregrine Dalziel, Andrew S. Liteplo, Peter Fagenholz, Vicki E. Noble. Focused Assessment with Sonography in Trauma and Abdominal Computed Tomography Utilization in Adult Trauma Patients: Trends over the Last Decade. Emerg Med Int. 2013; 2013: 678380.
- Ollerton JE, Sugrue M, Balogh Z, D'Amours SK, Giles A, Wyllie P. Prospective study to evaluate the influence of FAST on trauma patient management. J Trauma. 2006 Apr;60(4):785-91.
- Savatmongkorngul S, Wongwaisayawan S, Kaewlai R. Focused asse.ssment with sonography for trauma: current perspectives. Open Access Emerg Med. 2017 Jul 26; 9:57-62
- Alrajab S, Youssef AM, Akkus NI, Caldito G. Pleural ultrasonography versus chest radiography for the diagnosis of pneumothorax: review of the literature and meta-analysis. Crit Care. 2013 Sep 23;17(5): R208.
- Holmes JF, Lillis K, Monroe D, Borgialli D, Kerrey BT, Mahajan P et al. Identifying children at very low risk of clinically important blunt abdominal injuries. Ann Emerg Med. 2013 Aug;62(2):107-116.e2.
- Kornblith AE, Graf J2, Addo N3, Newton C4, Callcut R5, Grupp-Phelan J et al. The Utility of Focused Assessment with Sonography for Trauma (FAST) Enhanced Physical Examination in Children with Blunt Torso Trauma. Acad Emerg Med. 2020 Mar 11.
- Zanobetti M, Coppa A, Nazerian P, Grifoni S, Scorpiniti M, Innocenti F et al. Chest Abdominal-Focused Assessment Sonography for Trauma during the primary survey in the Emergency Department: the CA-FAST protocol. Eur J Trauma Emerg Surg. 2018 Dec;44(6):805-810.
- Arhami Dolatabadi A, Amini A, Hatamabadi H, Mohammadi P, Faghihi-Kashani S, Derakhshanfar H et al. Comparison of the accuracy and reproducibility of focused abdominal sonography for trauma performed by emergency medicine and radiology residents. Ultrasound Med Biol. 2014 Jul;40(7):1476-82.
- Gracias VH, Frankel HL, Gupta R, Malcynski J, Gandhi R, Collazzo L et al. Defining the learning curve for the Focused Abdominal Sonogram for Trauma (FAST) examination: implications for credentialing. Am Surg. 2001 Apr;67(4):364-8 .
- Osterwalder J, Mathis G, Hoffmann B. New Perspectives for Modern Trauma Management - Lessons Learned from 25 Years FAST and 15 Years E-FAST. Ultraschall Med. 2019 Oct;40(5):560-583.
- Akoglu H, Celik OF, Celik A, Ergelen R, Onur O, Denizbasi A. Diagnostic accuracy of the Extended Focused Abdominal Sonography for Trauma (E-FAST) performed by emergency physicians compared to CT. Am J Emerg Med. 2018 Jun;36(6):1014-1017.
- Lawrence A. Melniker. The value of focused assessment with sonography in trauma examination for the need for operative intervention in blunt torso trauma: a rebuttal to “emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma (review)”, from the Cochrane Collaboration. Crit Ultrasound J 1, 73–84 (2009).
- Stengel D, Bauwens K, Sehouli J, Porzsolt F, Rademacher G, Mutze S et al. Systematic review and meta-analysis of emergency ultrasonography for blunt abdominal trauma. Br J Surg. 2001 Jul;88(7):901-12.
- Becker A, Lin G, McKenney MG, Marttos A, Schulman CI. Is the FAST exam reliable in severely injured patients? Injury. 2010 May;41(5):479-83.
- Waheed KB, Baig AA, Raza A, Ul Hassan MZ, Khattab MA, Raza U. Diagnostic accuracy of Focused Assessment with Sonography for Trauma for blunt abdominal trauma in the Eastern Region of Saudi Arabia. Saudi Med J. 2018;39(6):598-602.
- Stengel D, Leisterer J, Ferrada P, Ekkernkamp A, Mutze S, Hoenning A. Point-of-care ultrasonography for diagnosing thoracoabdominal injuries in patients with blunt trauma. Cochrane Database Syst Rev. 20181;12:CD012669.
- Calder BW, Vogel AM, Zhang J, Mauldin PD, Huang EY, Savoie KB et al. Focused assessment with sonography for trauma in children after blunt abdominal trauma: A multi-institutional analysis. J Trauma Acute Care Surg. 2017;83(2):218-224.
- James F. Holmes, William E. Brant, William F. Bond, Peter E. Sokolove, Nathan Kuppermann. Emergency department ultrasonography in the evaluation of hypotensive and normotensive children with blunt abdominal trauma. 2001;36(7):968-973.
- Emery KH, McAneney CM, Racadio JM, Johnson ND, Evora DK, Garcia VF. Absent peritoneal fluid on screening trauma ultrasonography in children: a prospective comparison with computed tomography. J Pediatr Surg. 2001;36(4):565-9.
- Dehqanzada ZA, Meisinger Q, Doucet J, Smith A, Casola G, Coimbra R. Complete ultrasonography of trauma in screening blunt abdominal trauma patients is equivalent to computed tomographic scanning while reducing radiation exposure and cost. J Trauma Acute Care Surg. 2015;79(2):199-205.
- Zhang Z, Hong Y, Liu N, Chen Y. Diagnostic accuracy of contrast enhanced ultrasound in patients with blunt abdominal trauma presenting to the emergency department: a systematic review and meta-analysis. Sci Rep. 2017;30;7(1):4446.
- Nicolaj Grønbæk Laugesen, Christian Pallson Nolsoe, Jacob Rosenberg. Clinical Applications of Contrast-Enhanced Ultrasound in the Pediatric Work-Up of Focal Liver Lesions and Blunt Abdominal Trauma: A Systematic Review. Ultrasound Int Open. 2017;3(1):E2-E7.
- Catalano O, Lobianco R, Sandomenico F, Mattace Raso M, Siani A. Real-time, contrast-enhanced sonographic imaging in emergency radiology. Radiol Med. 2004;108(5-6):454-69.
- Piccolo CL, Trinci M, Pinto A, Brunese L, Miele V. Role of contrast-enhanced ultrasound (CEUS) in the diagnosis and management of traumatic splenic injuries. J Ultrasound. 2018;21(4):315-327
- Laselle BT, Byyny RL, Haukoos JS, Krzyzaniak SM, Brooks J, Dalton TR et al. False-negative FAST examination: associations with injury characteristics and patient outcomes. Ann Emerg Med. 2012;60(3):326-34.e3.
- Sigurveig Thorisdottir, Gudrun L Oladottir, Mari T Nummela, Seppo K Koskinen. Diagnostic performance of CT and the use of GI contrast material for detection of hollow viscus injury after penetrating abdominal trauma. Experience from a level 1 Nordic trauma center. Acta Radiologica. 2020 February.
- Yoshii H, Sato M, Yamamoto S, Motegi M, Okusawa S, Kitano M et al. Usefulness and limitations of ultrasonography in the initial evaluation of blunt abdominal trauma. J Trauma. 1998;45(1):45-50; discussion 50-1.
- Malhotra AK, Fabian TC, Katsis SB, Gavant ML, Croce MA. Blunt bowel and mesenteric injuries: the role of screening computed tomography. J Trauma. 2000;48(6):991-8; discussion 998-1000.
- Rodriguez C, Barone JE, Wilbanks TO, Rha CK, Miller K. Isolated free fluid on computed tomographic scan in blunt abdominal trauma: a systematic review of incidence and management. J Trauma. 2002;53(1):79-85.
- Long B, April MD, Summers S, Koyfman A. Whole body CT versus selective radiological imaging strategy in trauma: an evidence-based clinical review. Am J Emerg Med. 2017;35(9):1356-1362.
- Sierink JC, Treskes K, Edwards MJ, Beuker BJ, den Hartog D, Hohmann J et al. Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2): a randomised controlled trial. Lancet. 2016;388(10045):673-83.
- Taylor GA, Sivit CJ. Posttraumatic peritoneal fluid: is it a reliable indicator of intraabdominal injury in children? J Pediatr Surg. 1995;30(12):1644-8.
- Nunes LW, Simmons S, Hallowell MJ, Kinback R, Trooskin S, Kozar R. Diagnostic performance of trauma US in identifying abdominal or pelvic free fluid and serious abdominal or pelvic injury. Acad Radiol. 2001;8(2):128-36.
- Albanese CT, Meza MP, Gardner MJ, Smith SD, Rowe MI, Lynch JM. Is computed tomography a useful adjunct to the clinical examination for the diagnosis of pediatric gastrointestinal perforation from blunt abdominal trauma in children? J Trauma. 1996;40(3):417-21.
- Natarajan B , Gupta PK, Cemaj S, Sorensen M, Hatzoudis GI, Forse RA. FAST scan: is it worth doing in hemodynamically stable blunt trauma patients? Surgery. 2010;148(4):695-700; discussion 700-1.
- Boulanger BR, McLellan BA, Brenneman FD, Ochoa J, Kirkpatrick AW. Prospective evidence of the superiority of a sonography-based algorithm in the assessment of blunt abdominal injury. J Trauma. 1999;47(4):632-7.
- Ogedegbe C, Morchel H, Hazelwood V, Chaplin WF, Feldman J. Development and evaluation of a novel, real time mobile telesonography system in management of patients with abdominal trauma: study protocol. BMC Emerg Med. 2012;18(12):19.
- Montoya J, Stawicki SP, Evans DC, Bahner DP, Sparks S, Sharpe RP et al. From FAST to E-FAST: an overview of the evolution of ultrasound-based traumatic injury assessment. Eur J Trauma Emerg Surg. 2016;42(2):119-26.

