Comparative Study of Anterior Cervical Discectomy and Fusion by Cages versus Tricortical Bone Graft with Anterior Plate Fixation for Degenerative Cervical Disc Disease
Islam MA*, Goit RK, Shohidullah M, Rahman S, Arifeen KMN and Chowdhury AZ
Department of Orthopaedics, Bangabandhu Sheikh Mujib Medical University, Bangladesh
Received Date: 08/09/2020; Published Date: 09/11/2020
*Corresponding author: Md Anowarul Islam, Department of Orthopaedics, Bangabandhu Sheikh Mujib Medical University, Spine surgery, Dhaka, Bangladesh. E-mail: maislam.spine@gmail.com
Abstract
Background: Cervical degenerative disc disease is a common cause of neck pain and radiating arm pain. It develops when one or more of the cushioning discs in the cervical spine start to break down by wear and tear due to its degeneration. Multiple techniques and modalities of fixation are used in Anterior Cervical Discectomy and interbody Fusion (ACDF), each with some merit and demerit against others.
Objectives: To compare the safety and efficacy of ACDF by cages versus tricortical bone graft with anterior plate fixation for degenerative cervical disc disease.
Methods: This prospective observational study was conducted in the Department of Orthopaedics, BSMMU, Dhaka from March 2017 to February 2020. Forty patients with cervical spondylotic myelopathy diagnosed based on presenting complaints, clinical examination and investigations were enrolled in this study. Modified Odom’s criteria, Visual Analogue Scale (VAS), Nurick Grading and bridwell criteria for cervical spondylotic myelopathy was used for evaluation of the results.
Result: Male were predominant in this study. Male female ratio was 2.9: 1. Mean age of the patients was 48.6±7.4 years within the range of 40-65 years. Most of the patients were farmer (30%), C5/6 (55%) was the most commonly involved disc level. Most of the patients had clinical features of neck pain, gait difficulty and myelopathy sign. Regarding perioperative complications - transient dysphagia was seen in 5 (12.5%) patients and transient paraparesis was observed in 2 (5%) patients. Post-operative complications showed paresthesia, bone graft donar site pain and wound infection seen in significant number of patients of both groups who were recovered within 3 to 6 months. According of Bridwell grade of fusion, Grade I fusion was observed in 16 patients (80%) in cage group & 18 patients (90%) in tricortical ICG with plate group. The difference between two groups was not statistically significant (P=0.762). According to VAS, postoperatively pain was gradually decline and after 12 month, 12 patients (60%) patients were found in no pain group and 11 patients (55%) were found in no pain group of the tricortical ICG with plate group. There was no significant difference between the two groups (P=0.04). According to modified Odom’s criteria functional outcome after 12 month was excellent in 18 patients (90%) and good in 2 patients (10%) in cage group and excellent in 17 patients (85%) & good in 3 patients (15%) in tricortical ICG with plate group. There was no statistical significant difference between two groups (P=0.432).
Conclusion: ACDF is the ideal technique for the treatment of cervical disc disease with excellent functional outcome & good fusion, which could be achieved by either cage or tricortical ICG with plate. There is no significant difference in the post-operative follow up, fusion rate, clinical and functional outcomes between the cage and tricortical ICG with plate groups. Key words: Cervical degenerative disc disease, tricortical bone graft, ACDF.
Introduction
Cervical myelopathy is a syndrome that may result from spondylosis involving cervical vertebrae. When cervical myelopathy occurs as a result of spondylosis, it is referred to as cervical spondylotic myelopathy. Cervical spondylotic Patients present with various findings, including clumsiness, loss of manual function, difficult gait or balance, urinary problem, motor weakness, sensory changes, and abnormal or pathologic reflexes [1].
The circumferential compression due to spondylosis leads to spinal cord compression and a static impingement on the spinal cord. In addition, there is a dynamic component of spinal cord compression, as extension of the cervical spine can cause thickening of the ligamentum flavum and flexion can cause disc bulging. Cadaver studies confirm that the area inside the spinal canal is larger in forward bending than in backward [2]. Cervical motion and instability can cause pinching of the spinal cord between the anterior chondro-osseous spurs and the posterior ligamentous components [3].
The pathophysiology of cervical spondylotic myelopathy has multi factorial cause [4]. Static mechanical factors result in the loss or reduction of spinal canal diameter and spinal cord compression. With increasing age, the intervertebral discs desicates resulting in loss of disc height [5].
Anterior Cervical Discectomy and Fusion (ACDF) is surgical procedure for treating cervical disc disease. Classically, spinal fusion was obtained by means of iliac crest autograft. Since tricortical bone graft harvesting causes donor site morbidity in up to 30% of patients, the use of cage gained great popularity among surgeons in recent years. Physical characteristics of Polyetheretherketone (PEEK) cages improve spinal fusion whereas iliac crest auto graft for single or multilevel ACDF was found to be associated with higher fusion and significantly lower costs compared with cages, PEEK cages or other implants [6].
Interbody fusion provides spine surgeon the ability to decrease abnormal painful motion in the spine. Recent treatments confirms that that fusion is the ideal treatment in cervical PID. Several modalities of surgery for performing ACDF such as Cloward technique, Smith Robinson technique, Bailey/Badgley technique. Autograft and allograft along with different cages are used for fusion. If the graft is used alone without any cage, it could be collapsed, extruded and there could be pseudoarthosis. To achieve further stability and reduce complication plate with screw is used along with bone graft [7].
The goal of surgery is to decompress the cord and nerve roots while providing a stability and to restore alignment. ACDF using iliac crest autograft is the gold standard with excellent functional outcome. But donor site morbidity is a concern with the use of iliac crest autograft. PEEK cages have emerged as the implant of choice for interbody fusion in ACDF [8].
Method & Material
This prospective study was carried out at the Department of Orthopaedic Surgery at BSMMU, Shahbag, Dhaka from March 2017 to February 2020. A total of 40 patients were included were included: 20 in group A and 20 in group B. Patients with Progressive spinal cord compression due to Degenerative cervical disc prolapse, motor weakness in the upper and lower extremities, gait disturbance. Signs of myelopathy and radiculopathy and positive findings in X-ray, MRI, CT scan were included while patients with any fracture, dislocation of cervical spine infection, tumors, inflammatory or autoimmune disorder of cervical spine, hereditary spastic paraplegia were excluded from the study. After taking informed consent, detailed history and physical examination of each patient was performed. Plain radiographs and MRI of cervical spine were performed in all patients. All necessary investigations for surgery were performed before operation. Patients were allocated into two groups by purposive randomized sampling methods. One group received cage and other group received tricortical ICG with plate. A structured case record was used to interview and collect data. Patients were interviewed and case record form was filled up by the interviewers. Outcome is measured by using Visual Analogue Score (VAS) for pain, Nurick Grading for neurological, Bridwell criteria for radiological fussion. Final overall improvement was evaluated by Modified Odom´s criteria. All the data were compiled as well assorted properly and the quantitative data was analyzed statistically by using Statistical Package for Social Science (SPSS-22). The results were expressed as percentage and mean±SD and p<0.05 was considered as the level of significant. Comparison of continuous variables between the two groups was made with Student’s t-tests. Comparison of proportions between two groups was made with Chi-Square tests.
Surgical Procedure
Patient was positioned in supine. The Gardener-wells tong traction was applied. A sandbag was placed in the inter scapular area to extend the neck. Patient’s head is rotated slightly to the opposite of the planned approach. Transverse skin incisions over the targeted vertebral level was performed. The platysmal muscle was identified and incised. Extensive subplatysmal dissection was performed to reduce retraction injury. The esophagus was identified and retracted medially, while the sternocleidomastoid and underlying carotid sheath was retracted laterally. The prevertebral fascia was divided, and the longuscolli musculature was further retracted. Intraoperative radiographs was obtained to confirm the appropriate cervical level. The offending disc was removed with a rongeur. As the posterior aspect of the vertebral body was reached, osteophytes was removed. The posterior longitudinal ligament was visualized. The entire disc, vertebral body endplateds was decorticated. Bone graft was taken from the illic creast fot tricorticag group. Position was checked by fluoroscope. Then after proper haemostasis, longuscolli muscle along with cut edge of anterior longitudinal ligament were approximated, omohyoid muscle was repaired, platysmal layer, subcutaneous layer and skin were closed in layer. Sterile dressing was given and cervical orthosis was applied before extubation. The donor area was closed layer by layer and sterile dressing was applied (Figure 1A&B, Figure 2A&B).
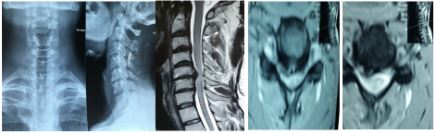
Figure 1A: Pre-operative X-ray and MRI of cervical spine.

Figure 1B: Per-operative picture, post-operative x-ray and 12 month post-operative CT scan of cervical spine showing ACDF with cage.
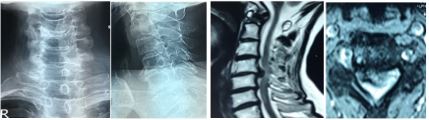
Figure 2A: Pre-operative X-ray of cervical spine A/P and lateral view and MRI of cervical spine.

Figure 2B: Per-operative picture with postoperative x-ray showing plate fixation.
Results
Most of the patients were found in the age of 51-60 years, 18 patients (45%) , 15 patients (37.5%) were seen in the age group 41-50 years, 5 patients (12.5%) were found in the age group ≤ 40 years, 2 patients (5%) were found in the age group ≥ 60 years. Mean age of the patients was 48.6±7.42 years, Mean age of cage group was 48.4±3.02 and tricortical ICG group was 47.3±2.12.
29 patients (72.5%) were male and 11 patients (27.5%) were female. Therefore, it commonly affects male population. Male female ratio was 2.9:1. Most of the patients were Farmers 12 (30%), housewife 10 (25%), business 8 (20%), day labour 7 (17.5%), service man 3 (7.5%).
Most commonly involved disc level was C5/6 (55%), then respectively C6/7, C4/5 and C3/4 disc level. In cage group, 12 patients (60%) found in C5/6 level and in tricortical ICG group, 10 patients (50%) found in C5/6 level of disc space.
Transient dysphagia was seen more in tricortical bone graft group. 5 (12.5%) patients were suffering from transient dysphagia among them 2 patients (10%) in cage group and 3 patients (15%) in tricortical ICG group. Transient paraparesis was developed in 2 (10%) patients among them 1 patient (5%) in cage group and 1 patient (5%) in tricortical ICG group who were recovered within very short period. Damage to the dura was not observed. Post operative paresthesia developed in 2 patients (10%) in 1 month in cage group and 2 patients (10%) in 1 month in tricortical bone graft group who were recovered within 2 months. Bone graft donor site pain developed in 5 patients (25%) in 1 month and 2 patients (10%) in 3 months seen only in tricortical bone graft with plate group. Wound infection was seen in 1 patient (5%) in 1 month seen only in tricortical bone graft with plate group.
According to VAS, among the 40 patients preoperatively 17 patients (42.5%) with s painful state level - 7, 13 patients (32.5%) with painful state level - 6 and 6 patients (15%) with painful state level 5 & 4 patients (10%) with painful state level 9. Postoperatively pain was gradually decline and at 12 month 12 patients (60%) were found in none pain level and 7 patients (35%) found in level 1 and 1 patient (5%) was found in pain state level 2 of the cage group and 11 patients (85%) were found in none pain level, 8 patients (40%) found in pain level 1 and 1 patient (5%) was found in pain level 2 of the tricortical ICG with plate group. There was no significant difference between the two groups (P=0.04).
According to Nurick grading (Table 1), out of 40 patients preoperatively 35 patients (87.5%) found in grade 3 level and 5 patients (12.5%) found in grade 4 level. Post operatively at 12 month in cage group 18 patients (90%) excellent and 2 patients (10%) good. In tricortical ICG group 16 patients (80%) excellent, 3 patients (15%) good and 1 patient (5%) fair. The difference between these two groups was not statistically significant (P=0.042).
According of Bridwell grade of fusion (Table 2), Grade I fusion was observed in 16 patients (80%) in 12 month in cage group and 18 patients (90%) in 12 month in tricortical bone graft with plate group. Grade of fusion was more in tricortical bone graft with plate group. The difference between these groups was not statistically significant (P=0.007).
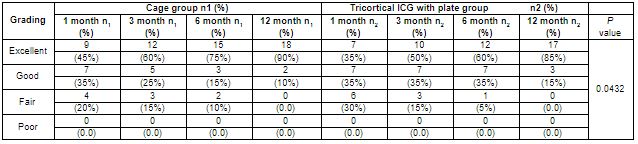
According to modified Odom’s criteria (Table 3) on post operative outcome - at 12 month of follow up 18 patients (90%) showed excellent, 2 patients (10%) showed good outcome in cage group and 17 patients (85%) showed excellent & 3 patients (15%) showed good outcome in tricortical bone graft with plate group. Poor and fair outcome was not found. The difference between these two groups was not statistically significant (P=0.0432).
Table 1: Distribution of study subjects according to Nurick grading (n=40; n1= 20 & n2 =20).
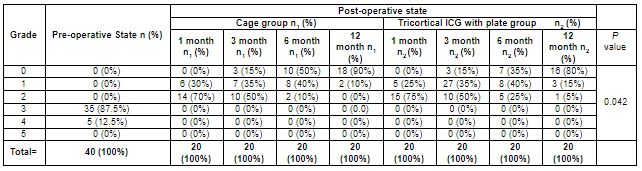
Table 2: Distribution of study subjects according to Bridwell grading system (n=40; n1= 20 & n2 =20).

Table 3: Distribution of study subjects according to modified Odom’s criteria (n=40; n1= 20 & n2 =20).
Discussion
Most of the patients were found in the age group 51-60 years and 10 patients (50%) were in cage group & 8 patients (40%) were found in tricortical bone graft group. Mean age of the patients was 48.6±7.42 years, Mean age of cage group was 48.4±3.02 and tricortical ICG group was 47.3±2.12. Spallone A et al., 2014 found mean age of their study subjects was 49.1±12.1 years [6]. Sharma A et al, 2018 found mean age in autograft group was 51.07±9.39 years compared with 47.3±9.3 years in PEEK cage group [8]. Male was predominant in this study. Male were 29 (72.5%) and female were 11 (27.5%) in number. Male female ratio was 2.9:1.0. Male was also predominant in the study of Sharma A et al., Siddiqui AA et al., Lee JC et al., and Adam FF et al., [8-11].
In this study, most of the patients were farmers (30%) then housewife (25%), business man (20%), day labourer (17.5%) and service man (7.5%). Among the 12 patients of farmer group 8 patients (40%) in the cage group and 4 patients (20%) in tricortical ICG group. Farmers are generally carry weight on head. Islam MA et al, 2012 showed sedentary workers (43.75%), heavy worker (18.75%) and housewife (37.5%) [12].
In this study, highest number of disc space involvement intervertebral was in the level of C5/6 (55%). Among that level of involvement, 12 patients (60%) in cage group and 10 patients (50%) in tricortical ICG group. Abdullah A et al., showed in their study highest number of patients in the level of C5/6 and among them 1 patient (8.3%) in cage group and 4 patients (33.3%) in plate group [13]. Ayman et al., showed that regarding the levels operated; there were 14 patients in C3/4 level, 18 patients in C4/5 level, 26 patients in C5/6 level and 4 patients in C6/7 level. All these are similar to our study [14].
Regarding perioperative complications, in our study transient dysphagia was seen in 5 patients (12.5%) and transient paraparesis in 2 patients (10%) who were recovered within very short period. 2 patients (10%) in cage group and 3 patients (15%) in tricortical ICG group were suffering from transient dysphagia. 1 patient (5%) in cage group and 1 patient (5%) in tricortical ICG group were suffering from transient paraparesis. Ayman et al., stated that there were some transient complications; dysphagia was reported in 5 patients (12.5%) which was improved within the first 2 weeks [14]. Islam MA et al., stated that in their study dysphagia was reported in 4 patients (13.3%) which was improved after 3 weeks [7]. Paresthesia developed in 2 patients (10%) in 1 month in cage group and 2 patients (10%) in 1 month in tricortical bone graft group who were recovered within 2 months. Bone graft donor site pain developed in 5 patients (25%) in 1 month and 2 patients (10%) in 3 months seen only in tricortical bone graft with plate group. Wound infection was seen in 1 patient (5%) in 1 month seen only in tricortical bone graft with plate group. Islam MA et al., stated that SSI in graft site reported in 1 patient (3.3%) [7]. Sharma A et al., stated in their study that perioperative complications seen in 18 patients in autograft group and 4 patients in PEEK cage group (P<0.05) [8].
According to VAS among the 40 patients preoperatively 17 patients (42.5%) with painful state level - 7, 13 patients (32.5%) with painful state level - 6, 6 patients (15%) with painful state level 5&4 patients (10%) with painful state level 9. and 10 patients (25%) with painful state level 7&6. Postoperatively pain was gradually decline at 12 month 12 patients (60%) were found in none pain level and 7 patients (35%) found in level 1 and 1 patient (5%) was found in pain state level 2 of the cage group. 11 patients (55%) were found in none pain level, 8 patients (40%) found in pain level 1 and 1 patient (5%) was found in pain level 2 of the tricortical ICG with plate group. There was no significant difference between the two groups (P=0.04). According to Spallone A et al., described that VAS for both neck and arm pain were significantly reduced within groups. Particularly, VAS score for neck pain decreased from 5.6±3.7 to 2.5±2.3 in patients treated with mini-invasive autologous bone graft (p .002) and from 5.9±3.8 to 2.4±2.5 in whom treated with PEEK cage (p 0.002). In the same fashion, VAS score at arm level reduced from 6.8±3.7 to 2.33±2.3 (p 0.001) in autologous group and from 6.2±3.8 to 2.6±2.7 in cage group (p 0.001). No differences have been observed between groups for both neck (p 0.847) and arm pain (p=0.532) [6]. Islam MA et al., described that significant post operative improvement was recorded after 24 months by VAS [7].
According to Nurick grading - out of 40 patients preoperatively 35 patients (87.5%) found in grade 3 level and 5 patients (12.5%) found in grade 4 level. Post operatively at 12 month in cage group 18 patients (90%) in grade 0 level (excellent) and 2 patients (10%) in grade 1 level (Good). In tricortical ICG group 16 patients (80%) in grade 0 level (excellent), 3 patients (15%) in grade 1 level (Good) and 1 patient (5%) in grade 2 level (Fair). The difference between these two groups was not statistically significant (P=0.0525). Islam MA et al., described that significant post operative improvement was recorded after 24 months by Nurick scale 93% were excellent in PEEK cage group and 86% in the ICG group. stastically it was not significant between two group p value <0.35 [7]. Smith and Robinson, 1958 outcome obtained as excellent in 64.2%, good in 14.2%, fair in 14.2% and poor in 7.1%. As a whole satisfactory outcome was 78.4% [16].
According of Bridwell grade of fusion, Grade I fusion was observed in 16 patients (80%) at 12 month in cage group and 18 patients (90%) at 12 month in tricortical ICG with plate group. The difference between these two group was not statistically significant (P=0.0762). Bony fusion was more in tricortical ICG group than cage group. Islam MA et al., stated in their study that fusion occurred in 13/15 patients (86%) segments of the PEEK group, while it was 14/15 (93.3%) of the ICG group segments [7]. Ayman et al., stated that fusion occurred in 17/20 patients (85%) and 29/34 (85.2%) segments of the PEEK group, while it was 18/20 patients (90%) and 25/28 (85.2%) segments of the ICG group [14,15]. Lee JC et al., stated that fusion status of the final follow up was 94.1% in allograft group, which showed 16 out of 17 patients had achieved union. In autograft group, 23 out of 24 patients had achieved union with the fusion rate of 95.7%. Fusion status was not significantly different between groups (P=0.663) [16].
In our study, according to modified Odom’s criteria functional outcome at 12 month of follow up excellent grade found in 18 patient (90%) & good grade found in 2 patients (10%) in cage group and excellent grade found in 17 patients (85%) & good grade found in 3 patients (15%) in tricortical ICG with plate group. There was no statistical significant difference between two groups. Ayman et al., stated in their study that according to Odom criteria, 18/20 patients (90%) were graded excellent - good in the cage group compared to 16/20 patients (85%) in the group with bone graft. No patients as graded poor. Islam MA et al., stated that according to Odom criteria, they graded 14 patients (93.3%) excellent-good in the cage group in comparison to 13 patients (86.6%) in the bone graft group [7].
Conclusion
ACDF is the ideal technique for the treatment of degenerative cervical disc disease with excellent functional outcome & good fusion which could be achieved by either cage or tricortical ICG with plate. There is no significant difference in the post operative follow up, fusion rate, clinical and functional outcomes between the cage and tricortical ICG with plate groups. Tricortical ICG with plate is an effective treatment of cervical disease with solid fusion and anterior cervical plating provides adequate stability. Cage can be an effective alternative with shorter operation time, good fusion and less donor site morbidity.
Ethical Issue
Informed writing was taken from the patients. Confidentiality, privacy of the patients ensured with respect and responsibility.
References:
- Rao RD, Currier BL, Albert TG. Degenerative cervical Spondylosis clinical syndromes, pathogenesis and management. The journal of bone and joint surgery. 2007;89:1360-1378.
- Waltz TA. Physical factors in the production of the myelopathy of cervical spondylosis. Brain. 1967;90:395-404.
- Robinson RA, Afeiche N, Dunn EJ, Northrup BE. Cervical Spondylotic Myelopathy, Etiology and treatment concepts. Spine. 1977;2:89-99.
- Bohlman HH, Emery SE, Goodfellow DB, Jones PK. Robinson anterior cervical discectomy and arthrodesis for cervical radiculopathy. Long-term follow-up of one hundred and twenty-two patients. JBJS. 1993;75:1298-1307.
- Wilkinson M. The morbid anatomy of cervical spondylosis and myelopathy. Brain. 1960;83:589-616.
- Spallone A, Marchione P. Anterior cervical discectomy and fusion with “mini-invasive” harvesting of iliac crest graft versus Polyetheretherketone (PEEK) cages: A retrospective outcome analysis. ELSEVIER International Journal of Surgery. 2014;12:1328-1332.
- Islam MA, Rana MM, Goni MF, Rahman MN. Comparison between anterior cervical discectomy with fusion by polyetheretherketone cages and tricortical iliac crest graft for the treatment of cervical prolapsed intervertebral disc. BSMMU J. 2016;9:169-172.
- Sharma A, Kishore H. Comparative study of functional outcome of anterior cervical decompression and interbody fusion with tricortical stnad alone iliac crest autograft versus stand alone polyetheretherketone cage in cervical spondylotic myelopathy. AO SPINE Global spine journal. 2018;8:860-865.
- Siddiqui AA, Jackowski A. Cage versus tricortical graft for cervical interbody fusion. The journal of bone & joint surgery (Br). 2003;85:1019-1025.
- Lee JC, Jang HD. Comparison of cortical ring allograft and plate fixation with autologous iliac bone graft for anterior cervical discectomy and fusion. ASJ Asian Spine Journal. 2019;13:258-264.
- Adam FF, Hasan KM, Meshtaway EM, Refae EH. PEEK cages versus locked plate for multiple levels cervical degenerated disease. Journal of American science. 2013;9:100-106.
- Islam MA, Habib MA, Sakeb N. Anterior Cervical Discectomy, Fusion and stabilization Bangladesh Medical Research Council Bulletin. 2012;38:62-66.
- Abdallah A, Taha AM. Cages or plates for anterior interbody fusion for cervical radiculopathy: single and double levels. The Egyptian Orthopaedic Journal. 2016;51:65-70.
- Ayman EA, Galhom MD. Comparison between Polyetheretherketone (PEEK) cages versus an iliac crest autograft used in treatment of single or double level anterior cervical discectomy. Med J Cairo Univ. 2013;81:9-17.
- Shao MH, Zhang F, Xu HC, Lyu FZ. Titanium cages versus autogenous iliac crest bone grafts in anterior cervical discectomy and fusion treatment of patients with cervical degenerative diseases: a systematic review and meta analysis. Current Medial Reasearch and Opinion. 2017;33:803-811.
- Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. JBJS. 1958;40:607-624.

