Comparison of Ambulation and Respiratory Kinesiotherapy in Hemodynamic and Ventilatory Parameters in Healthy Individuals
Rodrigo Daminello R1*, Angélica Queiroz FDR1, Alan Patrício da S1*, Blanca Elena GD1and Juliana ZR1
Laboratório de Delineamento de Estudos e Escrita Cientifica (Laboratoryof Design in ResearchandScientificWriting), Centro Universitário Saúde ABC, Santo André, São Paulo, Brasil
Received Date: 24/09/2020; Published Date: 27/10/2020
*Corresponding author: Rodrigo Daminello Raimundo, Laboratório de Delineamento de Estudos e Escrita Cientifica, Faculdade de Medicina ABC, RuaPrincipe de Gales, 667, Santo André, São Paulo, Brazil. E-mail: rodrigo.raimundo@fmabc.br
Abstract
Introduction: The immobilization of inpatients can cause several dysfunctions. Patient mobilization has shown to be effective in reducing hospital stay and is a key factor for functional recovery.
Objective: To compare the hemodynamic and ventilatory parameters in healthy individuals who underwent ambulation with respiratory kinesiotherapy.
Methods: A comparative study with 20 healthy individuals, aged between 21 and 35 years old. All participants went through two sessions on different days. The first day underwent three lung expansion exercises and ambulation in the second one. We measured hemodynamic and ventilatory values both at the beginning and end of each session.
Results: At baseline and final moment of "Respiratory Kinesiotherapy" (RK), the parameters showed statistical differences: maximal inspiratory pressure (MIP) (p = 0.035) and Borg dyspnea scale (p <0.001). For initial and final moments of the "Ambulation" (A) statistical differences were found in parameters: heart rate (HR) (p <0.001), maximal inspiratory pressure (MIP) (p = 0.003), maximal expiratory pressure (MEP) (p = 0.024) and Borg Scale for dyspnea and lower limb fatigue (p <0.001). By comparing the respiratory exercise with ambulation, there were small differences in heart rate (p = 0.004), respiratory rate (p = 0.004), peak expiratory flow (p = 0.025) and perception of dyspnea (p <0.001).
Conclusion: When comparing the initial and final parameters of respiratory kinesiotherapy and shortly after walking in healthy individuals, weidentified a difference in heart rate, respiratory rate, peak expiratory flow and perception of dyspnea.
Keywords: Mobilization; Physiotherapy; Inspiratory Pressure; Heart Rate
Introduction
Most hospitals in developed countries consider physiotherapy a crucial resource for the treatment of patients in Intensive Care Units (ICUs) [1]. With its insertion defined in the multidisciplinary team and with greater attribution aimed at preserving respiratory functions, physiotherapists face pathological situations and conditions that oblige them to reflect and act in a systematic, global and interactive way in order to minimize and/or reverse processes resulting from longer survival and prolonged stay in bed [2].
Immobilization of hospitalized patients can lead to several dysfunctions, such as respiratory excursion and stasis of secretions, whic mayresult in atelectasis, pneumonia, orthostatic hypotension and depression of the response of carotid baroreceptors due to prolonged decubitus, reduction of muscle contraction, especially in the lowerlimbs, which may cause decreasedreturn venous [3].
Over the last thirty years, early mobilization has shown a reduction in time to we an from ventilation and is the base for functional recovery. Recently, early physical activity received more attention as a safe andviableintervention in patients with neurological and cardio-respiratory stability. Earlymobilization includes progressive therapeutic activities, such as motor exercises in bed, bedsides edation, orthostatism, transfer to the chair and walking [4].
Accordingto some authors, inspiratory muscle training can improve inspiratory muscle strength and lower MIP and will likely decrease the sensation of respiratory effort. Therapeutic resources for pulmonary expansion or reexpansion in the management of critically illpatients arose due to the need to prevent or treat pulmonary volume reduction [5,2]. Some of the practices for pulmonary expansion are diaphragmatic exercises, deepinspiration, inspiration in times, localized chest expansion exercises and incentive spirometry. In 1980, Nicholson was the first to describe the use of deep inspiration for the treatment of respiratory diseases, it occurs when an inspiration that starts in the functional residual capacity (FRC) involves maximum inspiration upto total lungcapacity (TLC).
The inspiration by times consists of performing short, successive and programmed nasal inspirations, which can occur from two to six times. The various inspirations must be performed within the same respiratory cycle and oral expiration must be performed upto FRC level [6].
After a week of rest, muscle strength may decrease by up to 20%, with an additional 20% loss of strength the subsequent week. In immobility, the systems have changes that can lead to complications. One of the main objectives of the rehabilitation process is to help patients achieve the highest possible level of functional independence [6,7].
The importance of early walking has been discussed for some time. In 1972, Foss described a technique to increase ventilation in patients discharged from mechanical ventilation, while they walked, he also described the therapeutic benefits of this physical activity: a feeling of well-being and an increase in general strength [7].
Early mobilit in patients with respiratory diseases is not only viable and safe, but it is also an intervention that has the potential to prevent or treat the complications of critical neuromuscular disease [7].
Thus, in this study we aim to compare the hemodynamic and ventilatory parameters after walking in relation to respiratory kinesiotherapy (RK) in healthy individuals.
Method
This study was carried out in a private college located in São Paulo State, Brazil. Twenty healthy individuals of both sexes, aged between 21 and 35 years old who accepted to be part of the research and signed the free and informed consent form comprised the final sample of this study. Individuals with lung diseases, cardiovascular diseases and a body mass index (BMI) above 29.9 kg / m² were excluded.
The researchers conducted a small-scale pilot with three individuals to determine the time that would be set for walking, which would have to be approximately the same time spent for breathing exercises. The time was measured for the three individuals. The first one consumed 7 minutes and 51 seconds to perform 1 set often repetitions of each exercise. The second participant received the instruction to perform 2 sets of ten repetitions of each exercise. He spent 13 minutes and 42seconds. The third subject performed three sets of ten repetitions of each proposed exercise in 22 minutes and 30seconds.
Study Design and Intervention
After acomplished the small scale pilot, the scientists came to a consensus of conducting the study with 1 set of ten repetitions of each of the three exercises and a eight minutes walking.
Each participant performed one session, then after a 5 minutes rest, the hemodynamic andventilatory parameters were measured as follows: Systolic blood pressure (SBP), diastolic blood pressure (DBP) witha Premium® aneroid sphygmomanometer and Premium stethoscope ®, respiratory rate (f)andheart rate (HR) with a Nonin-onyx® pulseoximeter, thepeakexpiratoryflowwitha Pocketpeak® device, maximal inspiratorypressure (MIP), maximumexpiratorypressure (MEP) withthe Gerar® brand manuvacuometer and subjective perception of effort by the modified BORG scale (MBS).All data were transcribed into a spreadsheet.
Then, the participants received instructions to perform respiratory kinesiotherapy consisted of inhaling air until reaching TLC,d oinganapnea for ten seconds and exhaling slowly. They executed three exercises of lung expansion as follows:Maximum Deep Inspiration, Inspiration in Times withshoulderflexionat 90º andInspiration in Times with shoulder abductionat 90º, with 1 set of ten repetitions each. After the end of the exercises, all parameters were checked again.
The next day the participants performed the ambulation, so that the parameters were at baseline again. Before walking, parameters were collected. Participants got the instruction towalk in a flat corridor, at their own speed, without running and maintaining a fixed cadence. They received a verbal commandfor the beginning and end of walking, whichlasted 8 minutes. At theend, all individuals underwent for checking parameters and recorded them again.
Statistical Analysis
For analysis of statistical data, the researchers handled the program Sigma Statversion 3.5, using the x2 test for qualitative variables. For the quantitative variables, the Kolmogorov-smirnov test was performed to verify its normal distribution, and the Levine test to verify the homogeneityof the variances. For variables that showed normal distribution, thepaired t-testand / or t-test was used and for therest,theWilcoxontestand / or Mann-Whitney test. This study defined a significance level of 0.05 (5%) with 95% confidence intervals.
Results
The average age of participants was 25 with a standard deviationof 4 and a median of 25 years. The test of equality of two proportions indicated 30% menand 70% women. On average, the group had aweightof 67 kilograms, heightof 1.69 metersand a body mass index (BMI) of 24 Kg / m2. The parameters Maximum Inspiratory Pressure (MIP) and Borg Scale for Dyspnea showed statistical diferences at the starting and ending moments of the Respiratory Kinesiotherapy
The median of Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) remained at 110mmHg (p = 0.563) and 70mmHg (p = 0.750) respectively. The Mean Arterial Pressure ( MAP) increased from 80mmHg to 83mmHg (p = 0.734). The mean Heart Rate increased from 76 ± 13bpm to 80 ± 14bpm (p = 0.246). The median of Respiratory Rate (RR)remained at 18 rpm (p = 0.123). The median peak flow increased from 380L / min to 425L / min (p = 0.134). The mean of MIP increased from -106 ± 32cmH2O to -116 ± 31cmH2O (p = 0.038).
The MEP ranged from a median of 95 cmH2O to 100 cmH2O (p = 0.495). The Borg scale for dyspnea and for lower limb fatigue increased on average from 6 ± 1 to 10 ± 3 (p <0.001) and 7 ± 2 to 8 ± 2 (p = 0.330) respectively.
The parameters HR, MEP and Borg Scale for Dyspnea and for lower limb fatigue observed statistical diferences at the starting and ending moments of ambulation.
The medianof SBP and DBP remained at 110mmHg (p = 0.313) and 70mmHg (p = 0.990) respectively. The median MAP increased from 86mmHg to 88mmHg (p = 0.148). The mean HR increased from 77 ± 8bpm to 93 ± 15bpm (p <0.001). (Figure 1)
The median of Respiratory Rate (RR) increased from 18rpm to 25rpm (p = 0.003). The median of PEAK FLOW ascended from 405L / min to 406L / min (p = 0.107). The MAP median increased from -100cmH2O to -115cmH2O (p = 0.003) andMEP changed up from a medianof 95cmH2O to 105 cmH2O (p = 0.024). The Borgscale for dyspnea and for lowerlimb fatigue increased on average from 6 ± 1 to 9 ± 1 (p <0.001) and 7 ± 1 to 10 ± 2 (p <0.001) respectively. (Figure 2)
For comparison between the two moments (RK x A), the difference between the initial and final moments was calculated and analyzed by the t test or the Mann-Whitney test. Statistical differences werefound in the parameters: HR, RR, PEAK FLOW and MBS for lower limb fatigue.
The difference in median of SBP, DBP and MA Premained without alterations (p = 0.271, p = 0.574 and p = 0.527 respectively). The difference in the mean of HR increased from 3 ± 8bpm to 15 ± 14bpm (p = 0.004). The medianof RR changed from a decreaseof 2 rpm to an increase of 2 rpm (p = 0.004).
The median of PEAK FLOW varied from a decrease of 15L / min to an increase of 10L / min (p = 0.025). The median difference between MIP and MEP continued at 10 cmH2O (p = 0.844) and 10 cmH2O (p = 0.485). The MBS for dyspnea and for lower limb fatigue changed, median went from 3 to 2 (p = 0.450) and 0 to 2 (p <0.001) respectively. (Figure 3)
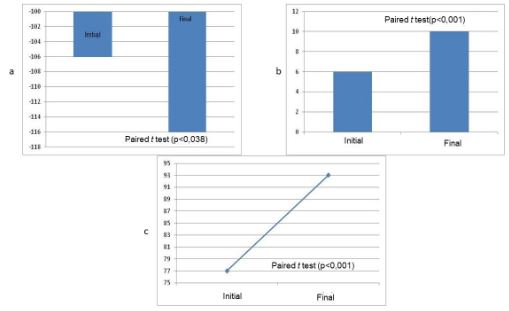
Figure 1: a) Performance of Maximum Inspiratory Pressure before and after Respiratory Kinesiotherapy; b) Borg Scale for Dyspnea at the Moment of Respiratory Kinesiotherapy; c) Response of Heart Rate before and after Ambulation.
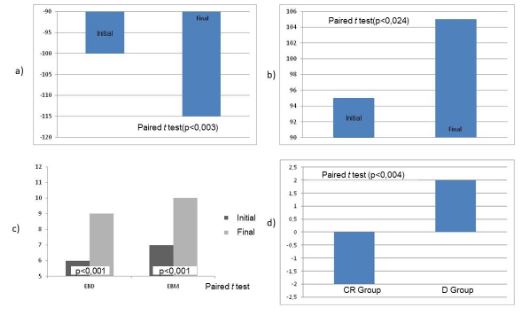
Figure 2: a)Performance of Maximum Inspiratory Pressure before and after Ambulation; b) Performance of Maximum Expiratory Pressure before and after Ambulation: c)Behavior of the Borg Scale for Dyspnea and the Borg Scale for Lower Limb Fatigue before and after Ambulation; d) Difference of Heart Rate between the Respiratory Kinesiotherapy Moment and the ambulationmoment.
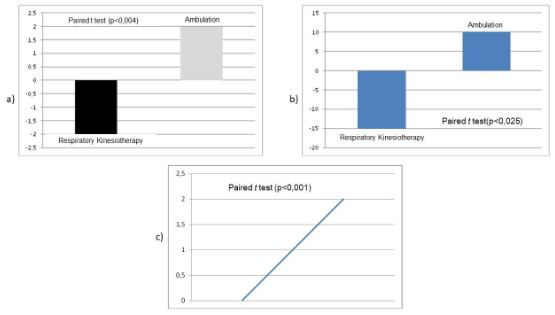
Figure 3: a) Difference of Respiratory Rate between the Respiratory Kinesiotherapy Moment and the Ambulation Moment; b) Difference of Peak Expiratory Flow between the moments of Respiratory Kinesiotherapy and Ambulation (A); c) Difference of the Borg scale for Lower Limb Fatigue between the moments of Respiratory Kinesiotherapy and the Ambulation.
Discussion
Therapeutic resources for pulmonary expansion orre-expansion in the management of critically ill patients arose due to the need to prevent or treat pulmonary volume reduction. The techniques are indicated mainly in situations where thereis a reduction in lung volumes and there is the presence or riskof alveolar collapse. Evidence shows that early mobilization (motor exercises in bed, sedation at the bedside, orthostatism, transfer to the chair and walking) has a positive impact in the time to we an from ventilation and is the basis for functional re-recovery [6,4,2] .
In this study, hemodynamic and ventilatory values were measured at the beginning and end of a series of lung expansion exercises of RK and walking. At the stage of RK there was a statistically significant increase only in the behavior of MIP.
Parreira et al., 2007[20] conducted a study with 103 healthy individuals, comparing the values of MIP and MEP which were collected after an nevaluation. They reported that the mean of MIP values in women was significantly lower than the predicted one, in men there was no significant difference between the values found and predicted. Notice that both studies used the same manuvacuometer model to measure the parameters MIP and MEP. Bruschi et al [21] in 1992, measured MIP and MEP in a population-based study with 625 healthy individuals. They found that MEP was significantly elevated compared to MIP. These results confirm that the most valuable use of MIP and MEP is the monitorization of changes in each patient.
In 2006, Cader et al. [22] evaluated the effect of inspiratory muscle strengthening on MIP inelderlypeople living in a nursing home. The elderly group performed 7 series ofs treng the ning, during 10weeks, 3 times a week, where the load was gradually increased. They concluded that isolated strengthening of the inspiratory muscles caused an increase in MIP. In the same perspective, the study by Costa et al. [23] evaluated respiratory muscle strength after 18 sessions of Functional Respiratory Reeducation, which consisted of respiratory guidance, breathing coordination exercises associated with trunk and limb movements, general muscle stretching and muscle relaxationtwice a week for 9 weeks, the result indicated a significant increase in MIP.
The work performed by Weiner et al.24 in 2002, also showed a significant increase in MIP, whereas the maticpatients were submitted to inspiratory muscle training. In addition to the increase in MIP, therewas a decrease in the scale of perception of dyspnea, so we see that there are no changes in MIP in healthy individuals when measured without any previous activity. After strengthening respiratory muscles or breathing exercises such as pulmonary expansion maneuvers, there is an increase in MIP, as there is an increase in TLC.
The other measured values (SBP, DBP, HR, RR andsensationofdyspnea) did not show significant results. This suggests us that RK, emphasizing on lung expansion exercises is effective for improving MIP, without causing any damage or significant changes in other body parameters. The PEAK FLOW and the MEP did not change significantly, so in pulmonary expansion therapy the main elevationisMIP.
At the time of ambulation, which was performed with the same individuals, there was a significant increase in the scale of perception of dyspnea, HR, MIPandMEP.
In 2008, thetask force of the European Respiratory Society and European Society of IntensiveCare Medicine[25] established a hierarchy of mobilization activities in the ICU, basedon a sequence of exercise intensity: change of decubitus and functional positioning, passive mobilization, assisted and active exercises, use of cycleergometers in bed; sit on the edge of thebed; orthostatism, static walking, transferring from bed tochair, exercise in thechairandwalking. The task force also recommends that the physiotherapist must be the professional responsible for implementing and managing the mobilization plan.
Dias et al.26 carried out a study in 2008 in individuals with acute myocardial infarction and unstable angina, to verify the circulatory response to a 50 meters walking after hospitalization. Theyobserved a post-walk increase in HR and a good tolerance to exercise according the Borgscale. A research with 49 adults who had undergone cardiopulmonary surgery to verify whether maximum inspiratory exercises or incentive spirometry had a therapeutic advantage over early mobilization. Patients were randomly assigned to one of three exercise programs, consisted of only early mobilization, early mobilization plus maximal inspiration exercises and early mobilization plus incentive spirometry. It was found that early mobilization together with inspiratory exercises or with incentive spirometry do not offer anytherapeutic advantage over early mobilization by itself (Dull, 1982) [27].
In the frame of theIII Brazilian Mechanical Ventilation Consensus, Jerre et al [28], 2007, showed the benefits of performing active and passive limb exercises during weaning and in patients recently released from mechanical ventilation. A multiprofessional approach that stimulated the early mobilization of patients in the postoperative period of abdominal aortic surgery resulted in decreased morbidity and length of hospital stay. Passive mobilization was instituted with degree of recommendation D (Expert opinion without critical assessment or based on basic materials) and active mobilization with degree of recommendation C (Case report).
A bibliographicsurveybyLopes et al. [29], 2008, aimedto determine the complications in patients with acute myocardial infarction who had early mobilization in relation to those who had the late one. The scientists found that shorter restperiods seem to be as safe as long periods, causing no or few complications. The resultsshowedthat, in addition to the early mobilization seem safe, it canalso decrease the hospital lenght of stay and, after discharge, these patients feel able to return to work earlier, when compared to the late mobilizationgroup. Exercise improves self-confidence, decreasing anxiety about daily physical activities, which encourages the patients to return to their daily lives. Regarding the studies thatcomparedearlyand late discharge, it is assumed that patients could have their hospitalization time reduced, since the complications and mortality of the two groups are similar.
The importance of early ambulation in hospitalized patients has been documented sincemanyyears ago. In 1997, Koch et al.[30] assessed the feasibility of safety and early walking after elective coronary angioplasty and stent placement through catheters and low-dose heparin. Patients who under went the procedure in the morning walked after 4hours and were compared with patients who under went the procedure in the afternoon, who walked the next morning. Walking after 4 hours was successful in all patients, being safe with low incidence of complications at the puncture site.
Cortes et al. [31] ,2007, conducted a study in 2007 to determine the impact of early mobilization on total mortality and non-fatal re-infarction after acute myocardial infarction (AMI). The systematic analysis showed a trendoflower mortality in patients with AMI who receive early mobilization, but does not preventre-infarction.
Conclusion
When comparing the initial and final parameters of respiratory kinesiotherapy and shortly after walking in healthy individuals, weidentified a difference in heart rate, respiratory rate, peak expiratory flow and perception of dyspnea. Therefore, respiratory kinesiotherapy and walking are safe to be performed and may perhaps be established in hospital practice in future studies.
References:
- Stiller K. Physiotherapy in Intensive Care towards an Evidence-Based Practice. Chest. 2000;118:1801-1813.
- França, Eduardo ET; Ferrari, Francimar R; Fernandes Patrícia V; Cavalcanti et al.. Força tarefa sobre a fisioterapia em pacientes críticos adultos: diretrizes da associação brasileira de fisioterapia respiratória e terapia intensiva e associação de medicina intensiva brasileira.
- Rosemary A. A Mobility Protocol for Critically Ill Adults. Dimens crit care nurs. 2007;26(5):175/179.
- Borges VM, Oliveira LRC, Peixoto E, Carvalh NAA. Fisioterapia motora em pacientes adultos em terapia intensiva. RevBras Ter Intensiva. 2009;21(4):446-452.
- Riera HS, Rubio TM, Ruiz FO, Ramos PC, Otero DDC, Hernandez TE et al..Inspiratory muscle training in patients with COPD: Effect on dyspnea, exercise performance and quality of life. Chest 2001;120;748-756.
- Sarmento GJV. O ABC da fisioterapia respiratória. 1 ed. Barueri, SP: Manole; 2009.
- Perme C, Chandrashekar R. Early Mobility and Walking Program for Patients in Intensive Care Units: Creating a Standard of Care. American Journal of Critical Care 2010:18.3:212-221.
- Levorin C, Spósito MMM, Jardim JRB. Fisioterapia respiratória-Princípios e técnicas. Acta Paulista de Enfermagem 1989;2(2):63-68.
- Regenga MM. Fisioterapia em cardiologia: da unidade de terapia intensiva à reabilitação. São Paulo: Roca; 2000.
- Abreu LC, Pereira VX, Valenti VE, Panzarin SA, Filho OFM. Uma visão da pratica da fisioterapia respiratória: ausência de evidência não de ausência. ArqMed ABC 32(Supl. 2):S76-8.
- Hall JE, Guyton AC. Tratado de Fisiologia Médica. São Paulo: Elsevier; 1999.
- Renault JA, Costa-Val R, Rossetti MB, Neto MH. Comparação entre exercícios de respiração profunda e espirometria de incentivo no pós-operatório de cirurgia de revascularização do miocárdio. Rev BrasCir Cardiovasc. 2009;24(2):165-172.
- Castro I. Cardiologia-Princípios e prática. Porto Alegre: Artmed; 1999.
- Monteiro MF, Filho DCS. Exercício físico e o controle da pressão arterial. RevBrasMed Esporte _ 2004;10(6).
- matuzzi, Marco Martins. Medicina de Reabilitação aplicada à ortopedia e traumatologia. Ed. 1. Roca. São Paulo, 1999.
- Dittmer DK, Teassel R. Complications of immobilization and bed rest. Canadian Family Physician. 1993;39.
- Souza MHL, Elias DO. Fundamentos da circulação extracorpórea. Rio de Janeiro: Alfa Rio; 2006.
- Almeida MB, Araújo CGS. Efeitos do treinamento aeróbico na freqüência cardíaca. RevBrasMed Esporte. 2003;9(2).
- Brandão MRF, Pereira MHN, Oliveira R, Matsudo VKR. Percepção do esforço: Uma revisão da área. Revista Brasileira de Ciência e Movimento. 3(1):34-40.
- Parreira VF, França DC, Zampa CC, Fonseca MM, Tomich GM et al.. Pressões respiratórias máximas: valores encontrados e preditos em indivíduos saudáveis. Revista Brasileira de Fisioterapia. 2007;11(5)361-368.
- Bruschi C, Cerveri I, Zoia MC, Fanfulla F, Fiorentini M et al.. Reference values of maximal respiratory mouth pressures: a population-based study. Am Rev. Respir. Dis. 1992;146(3):790-3.
- Cader S, Silva EB, Vale R, Bacelar S, Monteiro MD et al.. Efeito do treinamento dos músculos inspiratórios sobre a pressão inspiratória máxima e a autonomia funcional de idosos asilados. Montricidade. 2007;3(1): 279-288.
- Costa D, Sampaio LMM, Lorenzzo VAP, Jamami M, Damaso AR. Avaliação da força muscular respiratória e amplitudes torácicas e abdominais após a RFR em indivíduos obesos. Rev Latino-am Enfermagem - mar/abr. 2003;11(2):156-60.
- Weiner P, Magadle R, Beckerman M, Berar-Yanay M. The relationship among inspiratory muscle strength, the perception of dyspnea and inhaled beta2-agonist use in patients with asthma. Can Respir.J.- v.9, n.5 - sep/oct. 2002;307-312.
- Gosselink R, Bott J, Johnson M, et al. - Physiotherapy for adult patients with critical illness: recommendations of the European Respiratory Society and European Society of Intensive Care Medicine Task Force on Physiotherapy for Critically Ill Patients. Intensive Care Med, 2008;34:1188-1199.
- Dias CMC, Maiato ACCA, Baqueiro AMM, Fiqueredo AMF, Rosa FW et al.. Resposta à caminhada de 50 m na unidade coronariana, na síndrome coronariana aguda. ArqBrasCardiol 2009;92(2):135-142.
- Dull JL, Dull WL. Are maximal inspiratory breathing exercises or incentive spirometry better than early mobilization after cardiopulmonary bypass?. Physical therapy. 1983;63(5)655-659.
- Jerre G, Beraldo MA, Silva TJ, Gastaldi A, Kondo C et al.. Fisioterapia no paciente sob ventilação mecânica. Ver. Bras. de Terapia Intensiva – v.19, n.3 – jul/set, 2007;19(3):399-407.
- Lopes JL, Santos JT, Lima SC, Barros ALBL. Mobilização e alta precoce em pacientes com infarto agudo do miocárdio-revisão de literatura. Acta Paul Enferm - 2008;21(2):345-50.
- Koch KT, Piek JJ, Winter RJ, Mulder K, David GK et al.. Early ambulation after coronary angioplasty and stenting with six French guiding catheters and low-dose heparin. Excerpta medical. 1997;1084-1086.
- Cortes OL, Villar JC, Devereaux PJ, DiCenso A. Early mobilization for patients following acute myocardiac infarction: a systematic review and meta-analysis of experimental studies. International Journalof Nursing Studies. 2009;1496-1504.

