Unlocking the Locks in IV Thrombolysis
Satya Rao K1,*, Likhitha2 and Hemanth Kumar B3
1Former Professor of Neurology, Senior Consultant Medicover Hospital, India
2Junior Resident Neurology, Medicover Hospital, India
3MRCEM ER Physician Medicover Hospital, Visakhapatnam
Received Date: 11/07/2024; Published Date: 11/10/2024
*Corresponding author: Satya Rao K, Md, Dm (Neuro), Former Professor of Neurology, Senior Consultant Medicover Hospital, Visakhapatnam, India
Abstract
Stroke is the third most common cause of death in the world.
Ischemic stroke is most common when compared to haemorrhage. Management of ischemic stroke is most challenging one for the neurologist. Time is brain, is the concept which makes the management of ischemic stroke crucial as the so called golden period or Window period 3 to 4.30 hrs during which the patient is to be thrombolysed which makes the patient 's life useful to live and earn his bread and butter for the whole family. But we are not able to thrombolyse most of the cases. Our concern is why we are not able to do to all eligible patients and find out ways and means to improve thrombolysis.
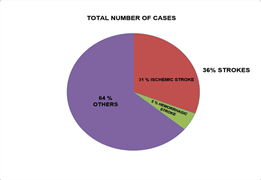
We have taken up this study in a 700 hundred bedded multi-speciality hospital in one year where we have analysed all the cases admitted under one senior neurologist analysed the stroke cases. Total number of cases admitted were 436 and ischemic stroke were 31 %. Thrombolysis could be done in only 9% of cases. We have interviewed the Patients and attendants the reasons why they could not come in time. We found the ultimate cause is unawareness. We came out with few solutions to improve the number of eligible cases the ways and means to improve.
Introduction
Brain Stroke is the third most common cause of death after RTA and CAD.
It is mainly divided into Ischemic and haemorrhagic strokes. Haemorrhagic stroke is nothing but intracerebral Haemorrhage where the management is entirely different. Ischemic stroke is further classified in to atherothrombotic and Embolic strokes. The main stay of management of ischemic stroke is acute and chronic stroke management. The acute stroke management is THROMBOLYSIS WHEN THEY REACH WITH IN THE SO CALLED WINDOW period that is between 3 to 4.5 hrs from the onset of Stroke.
We have collected all the ischemic stroke patients who were admitted under a single consultant both from OP and Emergency department from May 2023 to April 2024. All the patients aged beyond 18 yrs were taken. The risk factors of stroke were analysed and the time of arrival and fitness for THROMBOLYSIS were analysed. In this study our aim is to analyse the possible causes why a greater number of patients could not be thrombolysed were studied.
This is a study from a single tertiary 700 bedded hospital where there is established stroke unit with all imaging, Neurology and Neurosurgery facilities are available.
Materials and Methods and Analysis of data
We have studied all admissions under one senior neurologist and
collected all ischemic stroke patients beyond 18, yrs of age. This is a
Multi-specialty hospital with well-developed stroke team including the Neurosurgery back up.
- Statics in this study [1-6]
Total number of admissions in 1 year from May 2023 to April 2024 are 436.
Total number of strokes are 36.
Percent ischemic strokes: 31 percent
Haemorrhagic strokes: 5 percent
Thrombolysis done in 9 percent
Thrombolysis and thrombectomy done in 2 cases.
Number of deaths: 1
Analysis of risk factors:
Diabetes mellitus: 68
Hypertension: 109
Diabetes mellitus plus Hypertension: 54
Thrombophilia: 3 cases
Protein C deficiency: 1, Protein S deficiency: 1
Hyper homocysteinemia: 1 HYPERLIPIDEMIA: 5
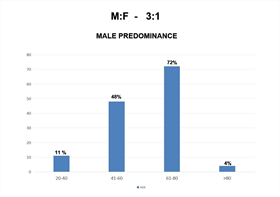
Age distribution: 20 to 40 yrs: 11
41 to 60 yrs: 48
60 to 80 yrs: 72
More than 80 yrs: 4
Sex Distribution: Dominant male distribution 3: 1
Analysis of Risk Factors in Stroke Patients [1]
The analysis of data from the study indicates several key points
regarding the demographics and risk factors associated with ischemic stroke patients:
- *Gender Predominance: *
The study shows a higher incidence of stroke in males compared to females. This male predominance is consistent with many other epidemiological studies on stroke.
- *Age Distribution: *
- The highest risk group for ischemic stroke is individuals aged 60 to 80 years. The second highest risk group is individuals aged 40 to 60 years.
- The second highest risk group is individuals aged 40 to 60 years.
- The 20 to 40 years age group has the lowest risk among the studied age ranges.
*Risk Factors: *
- *Hypertension [7] is identified as the most significant risk factor for ischemic stroke. This is consistent with global data indicating hypertension as a major modifiable risk factor for stroke.
- *Diabetes Mellitus [8] is the second most significant risk factor. Diabetes is known to increase the risk of stroke through various mechanisms, including accelerated atherosclerosis.
- The combination of *hypertension and diabetes mellitus* presents a higher risk than either condition alone, highlighting the compounded risk in patients with both conditions.
- *Thrombophilia [9] is also identified as a significant risk factor. Specific cases in the study include:
One patient with *protein C deficiency*.
One patient with *protein S deficiency*.
One patient with *hyperhomocysteinemia*.
Implications for the Management
Based on the identified risk factors, the management strategies for ischemic stroke patients in the study are as follows:
*Anti platelets vs. Anticoagulants: *
- *Anti platelets* are generally indicated for most patients with ischemic stroke, especially those with hypertension and diabetes mellitus. These medications help prevent platelet aggregation and subsequent thrombus formation in the arteries.
- *Anticoagulants* are specifically required for patients with thrombophilia. Conditions such as protein C deficiency, protein S deficiency, and hyperhomocysteinemia warrant the use of anticoagulants to prevent thrombus formation in the venous system and the heart. In addition, the patients with cardioembolic stroke needs to be treated with anticoagulants.
When once the patient enters the hospital the stroke team' will start working.
Fast history along with risk factors are taken and simultaneously all hematological investigations like blood sugar RFT, LFT, ECG, 2 D ECHO X-ray chest and PT with INR are done and immediately subjected for MRI or CT scan brain. when once the haemorrhage is ruled out and other investigations are normal we thrombolyse with Tenacteplase 0.25 mg per kg body weight except in 2 cases who were thrombolysed with,0.1 mg per kg body weight as they crossed 4.5 hrs [10] and the exact time could not be assessed.Taking the radiological picture( MRI) into consideration we have thrombolysed with 0.1mg dose basing on other studies where they found equally good results and the incidence of haemorrhagic transformation is very low.
Various studies showed that the lower dose is equally effective and younger patients, small infarcts, high risk individuals can be given this low dose got good results with least complications
All the patients who were thrombolysed are followed up in the stroke unit and followed the stroke protocol in monitoring the vitals. CT scan was done after 24 hrs and monitored the sensorium. If there is any bleed and there is altered sensorium, Neurosurgeon was alerted and if necessary, the patient will be subjected for surgery. In our study we didn't come across such situations.
We have followed the stroke protocol as given by SMART Criteria [3].
The earlier criteria laid down were very stringent and very few cases were thrombolysed. The present SMART guidelines show the only
contraindication for THROMBOLYSIS is Intracerebral haemorrhage. Leave alone the age, high or low blood sugar, previous head injury, previous
UGI or urethral bleed and size of infarct or seizures will not come in the way of THROMBOLYSIS.
Patients with accelerated hypertension are also taken for THROMBOLYSIS after reducing the blood pressure to normal range. Even if the patients are on anticoagulants we can correct the INR by giving the concerned antidote and thrombolyse. Patients who are on antiplatelets are not a contraindication for THROMBOLYSIS. Here in our study, we could thrombolyse two cases who were on oral anticoagulants. Warfarin in one case for Double valve replacement and another for Mitral valve replacement. Their INR was less than 1.7 and we could thrombolyse. Though patients on anticoagulants were an absolute contraindication for THROMBOLYSIS, taking INR into consideration of more than 1.7 corresponding antidote can be given along with FFP and thrombolyse but the time constraint is very important and to be done very fast. With the present guidelines the number of patients who can undergo THROMBOLYSIS have been increased. We have followed all the cases for more than 3 months except the last 2 cases who left the hospital on the third day because of financial constraints. All the other cases showed good improvement. They regained grade 3 power in the first week and at end of three months. Patients could do their normal activities without any support. Now the crux of the problem is why we are not able to get all eligible cases for THROMBOLYSIS and help them. Now our main aim is to identify the ways and means by which we can increase THROMBOLYSIS in eligible patients. We will discuss about this at the end of the study. Further evaluation was done with angiogram along with MRI for further management. We have not done thrombectomy in any patient.
Two patients came from outside after THROMBOLYSIS and thrombectomy. One patient showed good improvement at the end of three months and doing the normal activities. We lost one patient with large infarct who underwent THROMBOLYSIS and thrombectomy as they refused for surgical intervention. Along with THROMBOLYSIS, management of blood pressure and Diabetes mellitus were carried out. If any problem like ICH plan for surgical management was considered and the Neurosurgeon was alerted. In our study we didn't have any such problems and all the patients who were thrombolysed were discharged in good condition. All these patients were followed up and most of them showed good improvement in the first few days and the remaining at the end of three months showed good improvement. This shows the value of THROMBOLYSIS in the window period and the time is brain concept well established. Those patients who came after the window period we have tried for THROMBOLYSIS plus thrombectomy but none of them could get it done because of the financial burden, fear of improvement, and refusal from the supporting caregivers. Those patients who came after a day or two we have evaluated by imaging, identification of risk factors and their management was done along with the physiotherapy.
Evaluation of the causes of non Thrombolysed patients who came after the window period:
These patients are subjected for imaging for diagnosing haemorrhagic or ischemic stroke, hematological evaluation for diabetes mellitus, lipid profile, viral markers, RFT, LFT, CBC, ECG, X RAY CHEST, SICKELING, and coagulopathies. All the ischemic strokes are managed with anti-platelets, lipid lowering agents, anti-hypertensives and anti-diabetic drugs along with physiotherapy. If there is evidence of raised intracranial pressure either Mannitol or 3% saline infusion were given. If there is midline shift or deterioration in the sensorium surgical intervention was sought and managed.
All the patients after recovery were discharged with required advice and follow up was done. If there is evidence of carotid stenosis more than 70 percent the interventional radiologist opinion was taken and followed accordingly. Any evidence of coronary artery disease association if noticed Cardiologist consultation was taken and followed accordingly.
Discussion
Stroke is the third most common cause of death and disability after RTA and CAD. Ischemic stroke is one of the common presentations among other subcategories. The management of acute ischemic stroke is the
challenge for neurologist and emergency stroke team. When the patient reaches with in the window period that is between 3 to 4.5 hrs the implementation of the stroke protocol and THROMBOLYSIS needs expertise and dedication of the stroke team. Follow up of thrombolysed patient is very important to prevent further complications and management.
If we consider ASA guide lines 3 which are very stringent very small number of patients could have been thrombolysed. We have taken modified guidelines i.e., SMART criteria where the only contraindication is Intra cerebral haemorrhage. With these modified criteria more number of cases could be thrombolysed. However expected number of patients couldn't be managed because of various issues which will be discussed later.
Here in our study total number of stroke patients admitted are 436.The number of patients who reach in window period are 9%. All these patients were thrombolysed with Tenacteplase 0.25 mg per KG body weight as its half-life is more and ease of administration and economical.
Among these patients 2 patients are post operative double valve replacement one and single valve replacement one who are on anti-coagulants WARFARIN. Though they are on warfarin as the INR was less than 1.7 we could thrombolyse and saved lives. If we were to follow the earlier criteria patients on anti-coagulants is an absolute contraindication. In the present scenario though the patient is on anti-coagulants like vitamin K antagonists or Thrombin antagonists or factor X A inhibitors the corresponding antidote could have been given and thrombolysed. All thrombolysed patients were followed up for a period of one week to ten days and discharged with an advice of antiplatelets and lipid lowering agents, anti-hypertensives, anti-diabetics and physiotherapy and follow up was done every two to three weeks. When we monitored the regaining of power. At the end of three months most of them regained grade four power and were independent in their nature of work.
Two of our patients came from other hospitals where they underwent THROMBOLYSIS and thrombectomy.one of these is doing well with a power of grade four and the other we lost as the attendants are not willing for surgery as it's a big infarct with mid line shift. All the patients who came after the window period the recovery rate was good with small infarct size and out of the others with Zero power and bigger infarct size eighty percent are independent with mild to moderate disability and the remaining twenty percent are dependent on care givers. This study though small in number shows those who were thrombolysed showed very good improvement when compared with non thrombolysed patients.
Interaction with the patients and the attendants regarding the window period:
Interaction with the Patients and Attendants Regarding the Window Period: All the patients who came within and after the window period were interviewed along with their attendants to understand their awareness of the golden period for the management of stroke. The findings were as follows:
- *Lack of Awareness: *
- Many patients and their attendants were not aware of the critical window period for effective thrombolysis.
- There was a general lack of knowledge about the availability of thrombolysis facilities at tertiary hospitals.
- *Accessibility Issues: *
- Patients from remote areas had difficulty in reaching hospitals with the necessary facilities within the window period.
- Limited availability of transportation contributed to delays in reaching the hospital.
- *Transport Challenges: *
- Inadequate ambulance services further exacerbated delays, reducing the chances of timely thrombolysis.
How to overcome this situation or unlock the situation
We came out with few suggestions by which we can improve further the pitfalls or locking systems.
- Awareness Campaigns:
- To conduct educational meetings at various localities where the facilities are available or not and educate them and request to spread the news. This can be done through voluntary organizations like LIONS, ROTARY,MASONIC or any type of missions who does some voluntary service
- Upload speeches by the renowned neurologists in the YOU tube, instagrams or TIK-TOK etc where the youth are following.
- Use patient testimonials to educate public on the importance of timely hospital visits.
- Provide facilities of transport by ambulance where they can reach within a short period.
High end of the suggestion is to provide facilities with well-equipped AMBULANCE WITH A CT SCAN and communication with stroke team and when a stroke case is seen CT scan can be done and contact the stroke team and thrombolyse then and there and bring to the tertiary centre. This solves lot of problems and more number of patients can be treated and given good and reasonable This is the by which Telemedicine is used.
- Using extended window period from 6 to 12 hrs which may someone trials and experience.
- Provide ambulance facility at very short distance.
- Provide stroke units at every district headquarters hospital so that these patients can reach within time and get good treatment.
- Use artificial intelligence in making the patient lie down in the MRI where the patient is not cooperative adjust him in getting the MRI.
Artificial intelligence in stroke [4]
It includes
- A) Mechanical learning supervised and unsupervised and reinforced learning out of which the former most commonly used.
- B) Deep learning and
- C) Convolutional net works
THE SPERES WHERE THE ARTIFICIAL INTELLIGENCE IS USEFUL:
* In the diagnosis where the exact aetiology is not known.
* Useful in the diagnosis of size of ischemic penumbra
* Useful in the diagnosis and risk of stroke in Atrial fibrillation.
* Useful in the exact amount of stenosis in the carotid artery and stenting Useful in the diagnosis of stroke and stroke mimics.
* Great help in the radiological diagnosis.
* Useful in the prognostication of stroke.
* It can identify subclassification, predicts stroke related deaths and recovery time [5,6].
* Deep learning is useful in predicting the rupture of the atheromatous plaque and can classify the time of onset of Stroke.
This Artificial intelligence is of great help in the diagnosis and management of Stroke in many ways.
Conclusion
- *Timely Arrival: *
- Patients with stroke should reach hospitals within the window period for optimal management.
- *Experienced Stroke Teams: *
- Stroke teams with significant experience should handle the cases to improve outcomes.
- *Telemedicine: *
- Implement telemedicine to enhance thrombolysis rates by providing remote consultation and management.
- *Advanced Ambulance Services: *
- Equip ambulances with CT scan facilities and trained staff capable of performing thrombolysis as part of pre-hospital management.
*Artificial Intelligence: *
- Utilize AI to improve diagnostic accuracy and patient management, ultimately increasing the rate of successful thrombolysis.
The most crucial element is increasing public awareness about the "Time is Brain" concept and the significance of the golden period for stroke management. This effort requires collaboration between the medical community and government to ensure widespread understanding and implementation. These concepts proves the value of TIME IS BRAIN. Implementation of the above suggestions will definitely help the patients.
References
- Stroke Statistics: World Health Organization. (2021). Stroke, Cerebrovascular accident.
- Thrombolysis in Stroke: Hacke, W., et al. Thrombolysis with Alteplase 3 to 4.5 Hours after Acute Ischemic Stroke. New England Journal of Medicine, 2008; 359(13): 1317-1329.
- Smart Criteria: Powers WJ, et al. 2018 Guidelines for the Early Management of Patients with Acute Ischemic Stroke. Stroke, 2018; 49(3): e46-e110.
- Artificial Intelligence in Stroke Diagnosis: Chen, S., et al. (2019). AI in the Diagnosis and Management of Stroke. Journal of Stroke, 2019; 21(1): 1-11.
- Artificial intelligence in Acute ischemic stroke sub types G. Micell, National institute of health, 2023.
- Kaushik Chatterjec, Anirhan Dutta, Jayant Roy, et al. Augmenting neurological disorders prediction and rehabilitation using Artificial intelligence, 2022; 293-307.
- Hypertension and Stroke: O'Donnell MJ, et al. Risk factors for ischemic and intracerebral hemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet, 2010; 376(9735): 112-123.
- Diabetes Mellitus and Stroke: Emerging Risk Factors Collaboration. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet, 2010; 375(9733): 2215-2222.
- Thrombophilia and Stroke: Dentali F, et al. Thrombophilic abnormalities, oral contraceptives, and risk of cerebral vein thrombosis: a case control study. Stroke, 2007; 38(9): 2585-2590.
- Steven J, Warach Adrienna, et al. 0.1 to 0.2 mg/kg IV Tenacteplace Safe and feasible No adverse events with 0.1 mg / kg 0 to 12 hrs window period Tenacteplace thrombolysis for acute ischemic stroke, 2020; 51: 3440-3451.

