Laparoscopic Procedures in Urology Department: Experience from A Dedicated Cancer Hospital
Syed Adeel Ahmed1,*, Muhammad Mubashir Nawaz1, Areej Salim1, Arsalan Pervaiz1, Yasir Masood2, Saqib Shakeel1, Abdullah Maqbool1, Muhammad Zubair Cheema3, Mohammad Usman Khan1, Tariq Latif1, Aamir Ali Syed1 and Khurram Mir1
1Shaukat Khanum Memorial Cancer Hospital and Research Centre, Lahore Pakistan
2East Lancashire hospital NHS trust England
3Evercare Hospital, Lahore, Pakistan
Received Date: 04/04/2024; Published Date: 06/09/2024
*Corresponding author: Syed Adeel Ahmed, Shaukat Khanum Memorial Cancer Hospital and Research Centre, Lahore, Pakistan
Introduction
Approximately two decades ago, laparoscopy made its way into urology, starting slowly with procedures like pelvic lymphadenectomy, nephrectomy, and varicocelectomy. However, as enthusiasm grew, it became widely adopted across almost all urological operations. Technological advancements, including robotic-assisted laparoscopy, expanded its use in complex procedures like prostatectomy and cystectomy. These changes had a substantial impact on urological practices, significantly improving patient outcomes [1].
Laparoscopic approach is a minimally invasive alternative to open surgery for both non-malignant and malignant urological diseases. In 1990 Clayman & colleagues pioneered laparoscopic nephrectomy [2] when they removed a renal oncocytoma. Later Coptcoat and co-workers used same technique for radical nephrectomy [3].
Although laparoscopy is being increasingly used to treat urological malignancies, there is still concern regarding oncological safety [4]. Internationally published literature initially suggested short-term results suggest that laparoscopic radical nephrectomy does not carry an elevated risk of port site or retroperitoneal recurrence. However, a more extended follow-up was required to compare the long-term survival and disease-free rates with those associated with open surgery [5]. With time many studies indicated that laparoscopic surgery in renal and adrenal cancer is associated with oncologic long-term outcomes similar to those of open surgery.
A meta-analysis reported laparoscopic radical nephrectomy was associated with better surgical outcomes as assessed by overall mortality and postoperative complications compared with open radical nephrectomy, especially for those with small tumors (tumor size <7 cm); as well as better outcomes on cancer-specific mortality and local tumor recurrence. However, these results did not reach statistical significance [6].
Shaukat Khanum Memorial Cancer Hospital is dedicated oncology centre in a low – middle income country. We aimed to analyse our experience of laparoscopic surgery for malignancies of urological tumors.
Materials and Methods
This retrospective study will include all the patients who underwent laparoscopic procedures in the urology department at Shaukat Khanum memorial Cancer Hospital and Research Centre (SKMCH&RC). After approval from the Institutional Review Board (IRB), data was retrieved from the Hospital Information System (HIS) with the diagnosis of urinary tract and /or testicular malignancy from September 2019 till June 2023.
Variables including demographic details, age, gender, site, size of tumor, staging and grading of tumor, histological type, operative time, transfusion requirements, intra operative complication, conversion to open surgery, length of stay & post operative complications were assessed by filling a pre-designed proforma. The IBM SPSS version 20 (IBM Corp., Armonk, NY, USA) was used for data analysis. Mean and standard deviations were used to describe continuous variables data while frequencies and proportions were used to describe categorical data.
Results
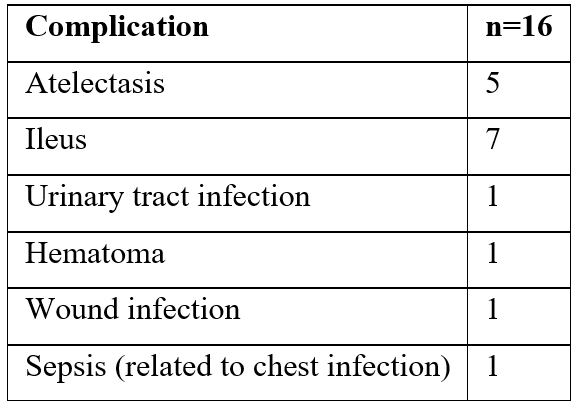
A total of 186 patients underwent laparoscopic surgeries during the study period. Majority of patients undergone radical nephrectomies (n 155) with mean age of 49.7 years, slight male predominance (n=101) (Table 1). Average tumor size was 5.27 +/_ 2.01 cm. Clear cell Renal cell cancer was the most common histopathology. The mean operative time was 155 +/- 49.3 minutes. Average blood loss was 43.2 ml with only 6 patients requiring post-operative blood transfusion. However, the average hospital stay was 3.6 (+/_1.3) days. A total of six patients were converted to open radical nephrectomy mainly due to injury to adjacent organs (Bleeding, IVC, Difficulty in reaching hilum, mesentery and small gut adherent to lower pole – fibrosis, large tumor and neo-vascularization, due to tumor covering hilum). Post-operative complications (Clavien-Dindo1 1and 2) occurred in 16 patients (8.6%) as detailed in Table 2.
Table 1: Laparoscopic Procedures.
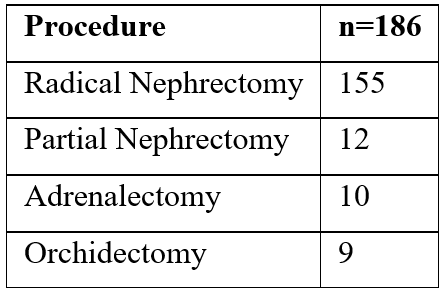
Table 2: Post-operative complications.
Discussion
Although laparoscopy is being increasingly used to treat urological malignancies, there is still concern regarding the induction of local recurrence and port site metastasis [4].
Laparoscopic radical nephrectomy has been shown to offer superior perioperative results to Open radical nephrectomy, including shorter hospital stay days, time to start oral intake, and convalescence time, and less estimated blood loss, blood transfusion rate, and anaesthetic consumption.[6] These results are comparable to our patients as well. With only 6 patients requiring blood transfusion, a short hospital stay of 3.6 (+/_1.3) days.
Although some studies report possible cause and effect between tumor size and complications [7]; in our study we did not find any correlation between tumor size and stage with intra operative or post operative complications or conversion to open surgery.
Conclusion
Laparoscopic nephrectomy appears to be efficient and reliable technique. This technique has led to a significant improvement in operative morbidity, mainly represented by length of stay, operative time and reduced need of blood transfusions.
Author’s Contribution
- Syed Adeel Ahmed: Concept and design of study, acquisition of data
- Muhammad Mubashir Nawaz: Drafting the article
- Areej Salim: Manuscript writing, analysis of data
- Arsalan Pervaiz: analysis of data , literature search
- Yasir Masood: acquisition of data
- Saqib Shakeel: acquisition of data
- Abdullah Maqbool: acquisition of data
- Muhammad Zubair Cheema: Concept
- Mohammad Usman Khan: ‘Guarantor’
- Tariq Latif: Final approval of the version to be published
- Aamir Ali Syed: Final approval of the version to be published
- KhurramMir: Final approval of the version to be published
Conflict of interest: There is no conflict of interest for any authors.
Ethical considerations: Institutional Review Board approval has been obtained. And informed consent for utilization of patient data for research and educational purposes was also obtained.
Funding: This study received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Janetschek G, Marberger M. Laparoscopic surgery in urology. Current Opinion in Urology, 2000; 10(4): 351-357.
- Clayman RV, Kavoussi LR, McDougall EM, Soper NJ, Figenshau RS, Chandhoke PS, et al. Laparoscopic nephrectomy: a review of 16 cases. Surgical Laparoscopy Endoscopy & Percutaneous Techniques, 1992; 2(1): 29-34.
- Rassweiler JJ, Henkel TO, Potempa DM, Coptcoat M, Alken P. The technique of transperitoneal laparoscopic nephrectomy, adrenalectomy and nephroureterectomy. European urology, 1993; 23(4): 425-430.
- Rassweiler J, Tsivian A, Kumar AR, Lymberakis C, Schulze M, Seeman O, et al. Oncological safety of laparoscopic surgery for urological malignancy: experience with more than 1,000 operations. The Journal of urology, 2003; 169(6): 2072-2075.
- Cadeddu JA, Ono Y, Clayman RV, Barrett PH, Janetschek G, Fentie DD, et al. Laparoscopic nephrectomy for renal cell cancer: evaluation of efficacy and safety: a multicenter experience. Urology, 1998; 52(5): 773-777.
- Liu G, Ma Y, Wang S, Han X, Gao D. Laparoscopic versus open radical nephrectomy for renal cell carcinoma: a systematic review and meta-analysis. Translational oncology, 2017; 10(4): 501-510.
- Zhang F, Hu JS, Zhang KY, Liu XH. Perioperative, functional, and oncologic outcomes of laparoscopic partial nephrectomy versus open partial nephrectomy for complex renal tumors: a systematic review and meta-analysis. Frontiers in Oncology, 2023; 13.

