Sphincter of Oddi Dysfunction: A Narrative Review
Eduardo Ramirez-Pimentel1, Wence F Villalvazo-Zuniga1, Martin Pena-Nunez1, Carlos A Bautista-Lopez1,2 and Jose M Aceves-Ayala1,*
1Department of General & GI Surgery, Hospital Civil de Guadalajara “Dr. Juan I. Menchaca”, Guadalajara, México
2Department of Surgical Clinics, University of Guadalajara, Guadalajara, Mexico
Received Date: 30/09/2023; Published Date: 04/03/2024
*Corresponding author: Jose M Aceves-Ayala, MD, Department of General & GI Surgery, Hospital Civil de Guadalajara “Dr. Juan I. Menchaca”Salvador Quevedo y Zubieta 750, 44340, Guadalajara, Jalisco, Mexico
Abstract
Sphincter of Oddi Dysfunction (SOD) is a rare clinical condition that often goes undetected within the traditional spectrum of differential diagnoses. Patients typically receive this diagnosis based on exclusion criteria, and they commonly experience recurrent biliary colic-like symptoms, especially after undergoing cholecystectomy. These symptoms frequently coincide with transaminitis, pancreatitis, or a combination of both. In severe cases, the condition can progress to clinically evident obstructive jaundice, and although rare, it can lead to chronic pancreatitis.
Despite the resemblance of several signs and symptoms to more serious pathological conditions, once these have been definitively ruled out, careful consideration must be given to sphincter of Oddi dysfunction as a potential underlying cause of the patient's discomfort.
This review discuses classification, diagnostic methods and treatment options for sphincter of Oddi dysfunction, with a particular focus on the significant role of minimally invasive diagnostic and therapeutic techniques like manometry and sphincterotomy in effectively managing this condition.
Keywords: Sphincter of Oddi Dysfunction (SOD); Common bile duct; Post-Cholecystectomy pain; Sphincterotomy; Functional biliary disorder; Manometry
Introduction
The term sphincter of Oddi dysfunction (SOD) is reserved for a seemingly heterogeneous group of pain conditions attributed to a benign disorder or dynamic anomalies in the sphincter of Oddi. Conceptualizing this disease process is easier when it is understood that SOD is a broad term describing a spectrum of hepatobiliary disorders [1]. The sphincter of Oddi dysfunction falls within the category of biliary dyskinesias, which are a group of conditions that can manifest as a motor dysfunction of the gallbladder or the sphincter of Oddi [2]. The exact epidemiology is unknown; however, it occurs more frequently in women between 20-50 years of age [1] and has an approximate prevalence of 1.5% in the USA [3]. The prevalence has significantly increased due to the availability of diagnostic tools we have today, such as Oddi sphincter manometry [4].
The typical clinical presentation of patients with SOD is characterized by colicky pain episodes in the right upper quadrant, with or without alterations in pancreatic enzymes or liver function tests. It can also manifest as recurrent episodes of idiopathic pancreatitis without an apparent site of obstruction. This condition is classified according to modified Milwaukee criteria, where SOD can be divided into 3 types, as outlined in Table 1 [3].
Table 1: Modified Milwaukee Classification.

The classic symptoms include nausea, vomiting, pain in the right upper quadrant that may radiate to the back, postprandial pain, worsening pain with fatty foods, weight loss, anorexia, and pain reproduction upon cholecystokinin stimulation. Additionally, there are some atypical symptoms such as diarrhea, chest pain, reflux symptoms, epigastric pain, and cramps [4].
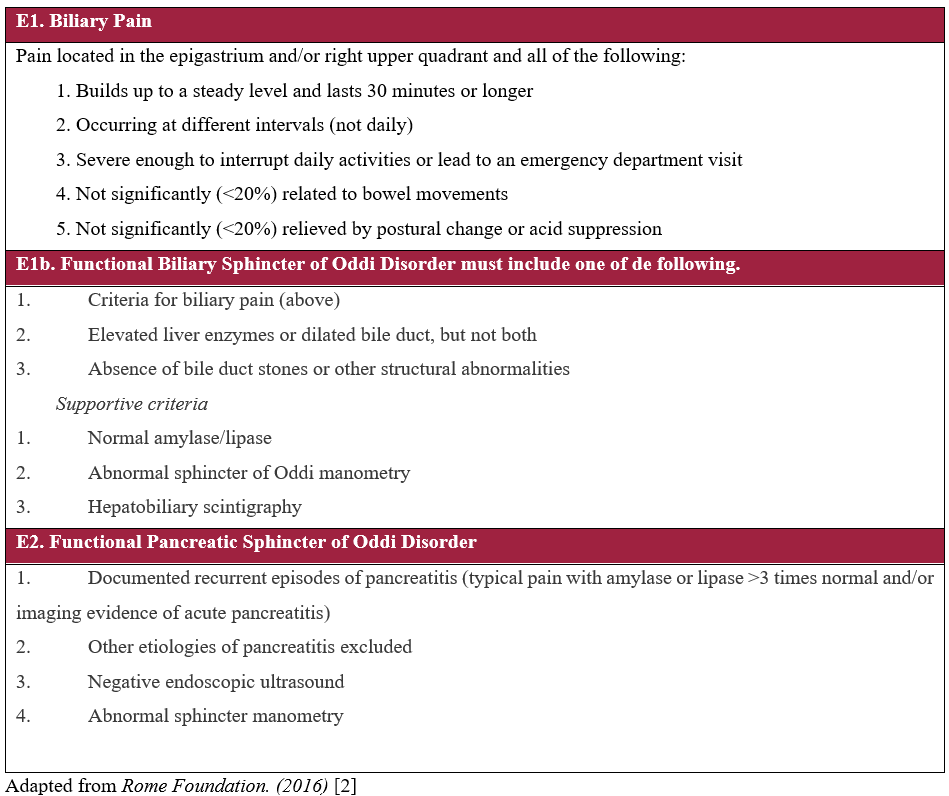
Being a rare, functional condition with challenging diagnosis, it requires proper assessment and differential diagnosis, ruling out mechanical obstructions such as cancer, cholelithiasis, and choledocholithiasis. Oddi sphincter problems are often identified after biliary surgery; however, they can also be associated with other functional disorders like irritable bowel syndrome [5]. The most recent diagnostic guidelines were established in the Rome IV [2] criteria for functional disorders of the gut and are listed in Table 2.
Table 2: Rome IV Criteria for Gallbladder and Sphincter of Oddi Disorder.
Anatomy and Physiology
While the sphincter of Oddi is often considered a single entity, it is actually composed of four sphincters that make up what is known as the sphincter of Boyden (also known as the choledochal sphincter) (Figure 1). The common ductal segment passes obliquely through the duodenal wall and ends at the Vater's papilla, a small protrusion with a diameter of less than 1 cm. Numerous variations are observed as the common bile and pancreatic ducts join [6].
The function of the sphincter of Oddi involves three main functions: regulating the flow of bile into the duodenum, preventing reflux into the bile or pancreatic ducts and promoting gallbladder filling between digestive cycles. Its function is mediated by various neurohumoral stimuli and regulated by Cajal's interstitial cells. During fasting, this sphincter remains active, preventing the passage of bile into the duodenum and the reflux of food content into the biliary and pancreatic ducts. During feeding periods, when cholecystokinin (CCK) stimulates its relaxation, the sphincter reduces its basal tone to allow the passage of biliopancreatic content [7,8].

Figure 1: Schematic representation of the four sphincters that make up the Boyden sphincter. 1) superior choledochal sphincter. 2) inferior choledochal sphincter (submucous). 3) sphincter of the ampulla (papilla). 4) pancreatic sphincter.
Diagnosis
Diagnosis is based on the clinical criteria of Rome IV[2] and is complemented by liver function tests, pancreatic enzymes (amylase and lipase), and endoscopic biliary manometry[9].
Manometry of the sphincter is performed during endoscopic retrograde cholangiopancreatography (ERCP) and provides direct information about the motor activity of the sphincter itself. However, this method has been infrequently used because it is invasive and carries a high risk of complications, with the potential to develop pancreatitis in up to 30% of cases [9,10]. It's important to note that certain drugs can affect manometry results, including midazolam, calcium channel blockers, anticholinergics, cholinergics, nitrates, and opioids.
Among the manometric diagnostic criteria are the following [5]:
- Sphincter pressure > 40 mmHg or 3 Standard Deviations (SD) above the average.
- Contractions > 8 per minute.
- Retrograde propagation increase > 50%.
There are various non-invasive diagnostic methods, such as scintigraphy, functional magnetic resonance imaging, optical coherence tomography, and the Functional Lumen Imaging Probe (FLIP) [11]. Technetium-99m (99mTc) scintigraphy is a quantitative, reliable, and non-invasive method used in patients who have undergone cholecystectomy. It is employed to assess the bile flow rate into the duodenum. However, the cutoff point is not well established and is difficult to interpret due to variations in methodology, clinical indications, patient characteristics and a lack of consensus regarding its diagnostic use [9].
In their original article, Sostre et al. [12] describe a scoring system where patients are divided based on their total score; a score <4 (14 pts) is considered negative, and a score >5 (12 pts) is considered positive for SOD. When correlated with manometry, the study achieved a sensitivity of 100% and specificity of 100%. Therefore, all positive patients either had elevated basal sphincter pressure (>40 mmHg), demonstrated a paradoxical response to CCK with sphincter pressure elevation, or had normal basal pressure but with common bile duct dilation and delayed contrast emptying during ERCP [13].
Functional MRI is considered a non-invasive method with good resolution, using gadolinium to assess the biliary tract, based on the premise that SOD is caused by delayed emptying of a contrast agent into the duodenum [9].
Optical coherence tomography generates high-resolution, real-time images of the microstructure of the sphincter using a probe inserted into the common bile duct via a catheter during ERCP [4].
Another study, with lower sensitivity and specificity but widely used for diagnosis, is ultrasound with fatty meal or CCK stimulation, where duct dilation of at least 2 mm after 45 minutes of ingestion suggests sphincter dysfunction [5].
Treatment
There is limited high-quality data on the management of SOD because the diagnosis is often accompanied by an underlying gallbladder condition, such as gallbladder dyskinesia, and the indiscriminate use of ERCP with sphincterotomy, which delays proper diagnosis and management [14].
Patients with type I and II SOD generally respond well to endoscopic treatment with sphincterotomy, which should be performed after ruling out any underlying mechanical causes and ideally confirming sphincter hypertension through manometry. A small group of patients may experience ampullary restenosis, which will require repeat sphincterotomy [5,10]. The EPISOD trial demonstrated that there was no benefit associated with endoscopic sphincterotomy for patients with type III SOD [10]. In these patients, however, the endoscopic injection of botulinum toxin into the sphincter has been shown to significantly reduce pain [15].
Conservative treatment with medications works in selected patients, primarily in those with type III SOD, providing pain relief mainly with IV opioids, amitriptyline, antispasmodics (hyoscine) or calcium channel blockers like nifedipine. The use of octreotide 100 mcg/day also appears to play an important role in reducing sphincter tone [5,16].
Laparoscopic cholecystectomy can be considered an acceptable surgical intervention in patients with concurrent biliary disease and Oddi sphincter dysfunction who experience chronic pain in the upper right quadrant [17]. Current recommendations suggest selecting patients with classic biliary symptoms for a period of 3 months. Predictors of a favorable response to treatment include classic biliary pain and onset of pain triggered by a cholecystokinin test and [5]. It should be noted that in patients with atypical symptoms such as abdominal distension, dyspepsia, early satiety, or weight loss, other causes, including neoplasms, should be investigated [5,16].
Conclusion
Sphincter of Dysfunction (SOD) remains a rare condition that is easily overlooked in the differential diagnosis of abdominal pain. It affects a young and working segment of society, leading to significant limitations and changes in their quality of life. Being a functional disorder with a challenging diagnosis, many of these patients are often misdiagnosed with other conditions. Due to the limited amount of evidence available, widely accepted diagnostic tests are still lacking, so its diagnosis continues to rely on functional criteria and ruling out other pathologies. Treatment remains a topic of controversy, with endoscopic therapy being the most supported option. However, it is not universally effective, highlighting the need for further research to explore potential therapeutic alternatives and provide patients with the best treatment options. In the ever-evolving landscape of medical research, there is a pressing need for further investigation into SOD. Ongoing studies and emerging therapies hold promise for improving patient outcomes and their overall quality of life.
Authorship Criteria:
Eduardo Ramírez-Pimentel, MD: Concept, data acquisition and drafting.
Wence Villalvazo-Zuñiga MD: Design and drafting.
Martin Peña-Núñez MD: Data acquisition.
Carlos A. Bautista-López, MD, MSc: Concept and revision.
José M. Aceves-Ayala MD: Drafting, final revision and approval. Guarantor author.
Conflict of Interest and Grant Information:
There are no disclaimers, grant support, or conflicts of interest to declare. The present publication is being submitted in the category of Mini-Review. This paper is not based on any previous communication o meeting. Ethical clearance has been obtained by the authors through a proper informed consent format that the patient signed to authorize the use of his personal information.
References
- Afghani E, Lo SK, Covington PS, Cash BD, Pandol SJ. Sphincter of Oddi Function and Risk Factors for Dysfunction. Front Nutr, 2017; 4. https://doi.org/10.3389/FNUT.2017.00001.
- Rome Foundation. Rome IV Criteria. Rome IV Criteria Gallbladder and Sphincter of Oddi Disorders, 2016.
- Small AJ, Kozarek RA. Sphincter of Oddi Dysfunction. Gastrointest Endosc Clin N Am, 2015; 25: 749–763. https://doi.org/10.1016/J.GIEC.2015.06.009.
- Clark CJ. An Update on Biliary Dyskinesia. Surgical Clinics of North America, 2019; 99: 203–214. https://doi.org/10.1016/j.suc.2018.11.004.
- Kim JV, Wu GY. Update on Sphincter of Oddi Dysfunction: A Review. J Clin Transl Hepatol, 2022; 10: 515–521. https://doi.org/10.14218/JCTH.2021.00167.
- Lee J Skandalakis. Surgical Anatomy and Technique. Cham: Springer International Publishing, 2021. https://doi.org/10.1007/978-3-030-51313-9.
- Yoo BM, Kim JH, Yang MJ, Lehman GA, Hwang JC, Kim SS, et al. Cyclic Change of Sphincter of Oddi Motility and Its Relationship with Small Bowel Migrating Motor Complex in Humans. Dig Dis Sci, 2018; 63: 3425–3433. https://doi.org/10.1007/S10620-018-5276-0.
- Crittenden JP, Dattilo JB. Sphincter of Oddi Dysfunction - StatPearls - NCBI Bookshelf. StatPearls, 2023.
- Kegnæs M, Novovic S, Shabanzadeh DM. Dysfunction of Biliary Sphincter of Oddi—Clinical, Diagnostic and Treatment Challenges. J Clin Med, 2023; 12. https://doi.org/10.3390/jcm12144802.
- Smith ZL, Shah R, Elmunzer BJ, Chak A. The Next EPISOD: Trends in Utilization of Endoscopic Sphincterotomy for Sphincter of Oddi Dysfunction from 2010-2019. Clin Gastroenterol Hepatol, 2022; 20: e600–609. https://doi.org/10.1016/J.CGH.2020.11.008.
- Boivineau G, Gonzalez JM, Gasmi M, Vitton V, Barthet M. Sphincter of Oddi dysfunction. J Visc Surg, 2022; 159: S16–21. https://doi.org/10.1016/J.JVISCSURG.2022.01.008.
- Sostre S, Kalloo AN, Spiegler EJ, Camargo EE, Wagner HN. A noninvasive test of sphincter of Oddi dysfunction in postcholecystectomy patients: the scintigraphic score. J Nucl Med, 1992; 33: 1216–1222.
- L B. A New Approach to Identify Sphincter of Oddi Dysfunction. Journal of Advances in Radiology and Medical Imaging, 2016; 1. https://doi.org/10.15744/2456-5504.1.104.
- Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder Dysfunction: Cholecystitis, Choledocholithiasis, Cholangitis, and Biliary Dyskinesia. Prim Care, 2017; 44: 575–597. https://doi.org/10.1016/J.POP.2017.07.002.
- Menon S, Kurien R, Mathew R. The role of intrasphincteric botulinum toxin injection in the management of functional biliary pain: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol, 2020; 32: 984–989. https://doi.org/10.1097/MEG.0000000000001773.
- Isherwood J, Oakland K, Khanna A. A systematic review of the aetiology and management of post cholecystectomy syndrome. Surgeon, 2019; 17: 33–42. https://doi.org/10.1016/J.SURGE.2018.04.001.
- Rehman S, Singh KK, Sajid MS. Role of laparoscopic cholecystectomy in the management of chronic right upper quadrant pain due to biliary dyskinesia: A systematic review and meta-analysis. Transl Gastroenterol Hepatol, 2019; 4. https://doi.org/10.21037/TGH.2019.08.10.

