Autoimmune Encephalitis Masquerading Creutzfeldt- Jakob Disease
Satya Rao Kolli1,*, Mohan S Maharaj2 and Tejasree D3
1Former Professor of Neurology, Senior Consultant, Medicover Hospitals, Visakhapatnam, India
2Director of Critical Care and Pain Management Services. MD (Anaesthesia), PDCC IDCCM. MBA, AMPH, Medicover Hospitals, India
3Junior Resident Neurology, Medicover Hospitals, India
Received Date: 03/06/2023; Published Date: 03/10/2023
*Corresponding author: Satya Rao Kolli, Former Professor of Neurology, Senior Consultant, Medicover Hospitals, Visakhapatnam, India
Abstract
CJD a very uncommon disease which occurs in one in 1 million cases. It should be diagnosed by clinical, radiological and laboratory evaluation. Clinical presentation is behavioral disturbances, progressive memory disturbances, involuntary movements like dystonia, catatonia, seizures and Myoclonic jerks. MRI shows hyper intense foci in the bilateral ganglionic regions and ribbon like hyper intense lesion in the parieto - occipital cortex in DWI. CSF examination shows positive protein 14-3-3 with mild rise in protein and cellular response. There is no treatment for the disease except for symptomatic management and progresses over a period of 1-2 years and succumbs to death. There are 4 types of CJD which will be discussed later.
In the recent 10-15 years several varieties of Autoimmune encephalitis have been identified, out of which Hashimoto's Encephalopathy is a common entity. In the early stage of disease, the patient will have similar symptoms like CJD, like behavioral disturbances, progressive memory loss, involuntary movements like dystonia, catatonia and seizures. The diagnosis can be made by way of the presence of autoimmune antibodies in the CSF and blood. This makes us to differentiate between Autoimmune encephalitis and CJD as the earliest manifestation are similar in both the conditions. The early diagnosis makes the correct early management of Autoimmune encephalitis where the patient recovers fast whereas CJD has no treatment and the patient succumbs subsequently.
Here we have a 51 years old female, who presented with similar symptomatology which made us to think of Hashimoto's Encephalopathy. The patient was treated with Methylprednisolone and later IV IG with no improvement at all. Here the patient has positive TPO anitibodies and myxoedema. Subsequently the patient was evaluated further because of progressive deterioration in the sensorium, uncontrolled seizures and myoclonic jerks. Further evaluation of CSF and MRI are in favour of CJD. These things made us to think of the possibility of CJD. Here the confusion between CJD and Hashimoto's encephalopathy is because of similar symptomatology in the early stage but subsequent evaluation confirms the diagnosis.
Keywords: CJD: Creutzfeldt- Jakob Disease; AE: Autoimmune Encephalitis; BSE: Bovine Spongiform Encephalopathy
Case Vignette
A 51 years old female presented with behavioral disturbances for one month, drowsiness for 15 days, jerks for 10 days. Patient was admitted elsewhere with these symptoms and evaluated. The laboratory evaluation showed TPO positive antibodies and myxoedema. Hence the possibility of Hashimoto's Encephalopathy was considered. She was given Methylprednisolone 1gm per day for 5 days. Patient did not show any improvement and shifted to the present hospital. On examination patient was drowsy, not responding to verbal commands. Dolls eye movements was normal. Dystonia of the limbs present. is evidence of multi focal and generalized seizures and frequent myoclonic jerks present. Rigidity of the limbs present. Plantares were bilateral extensors.
Investigations:
Haematological investigations were normal except TPO positive antibodies
1300 units /ml (0 to 34 iu/ ml normal range)
Thyroid profile- Myxoedema+
MRI Brain:
Predominant Grey matter involvement was seen.
Bilateral hyper intense foci in bilateral ganglionic regions present in DWI.
Hyper intense ribbon like manifestation with diffusion restriction is seen in dw1 images in the cortical Grey matter extending from fronto parietal to occipital regions.

Figure 1: EEG showed periodic sharp waves with slow background.
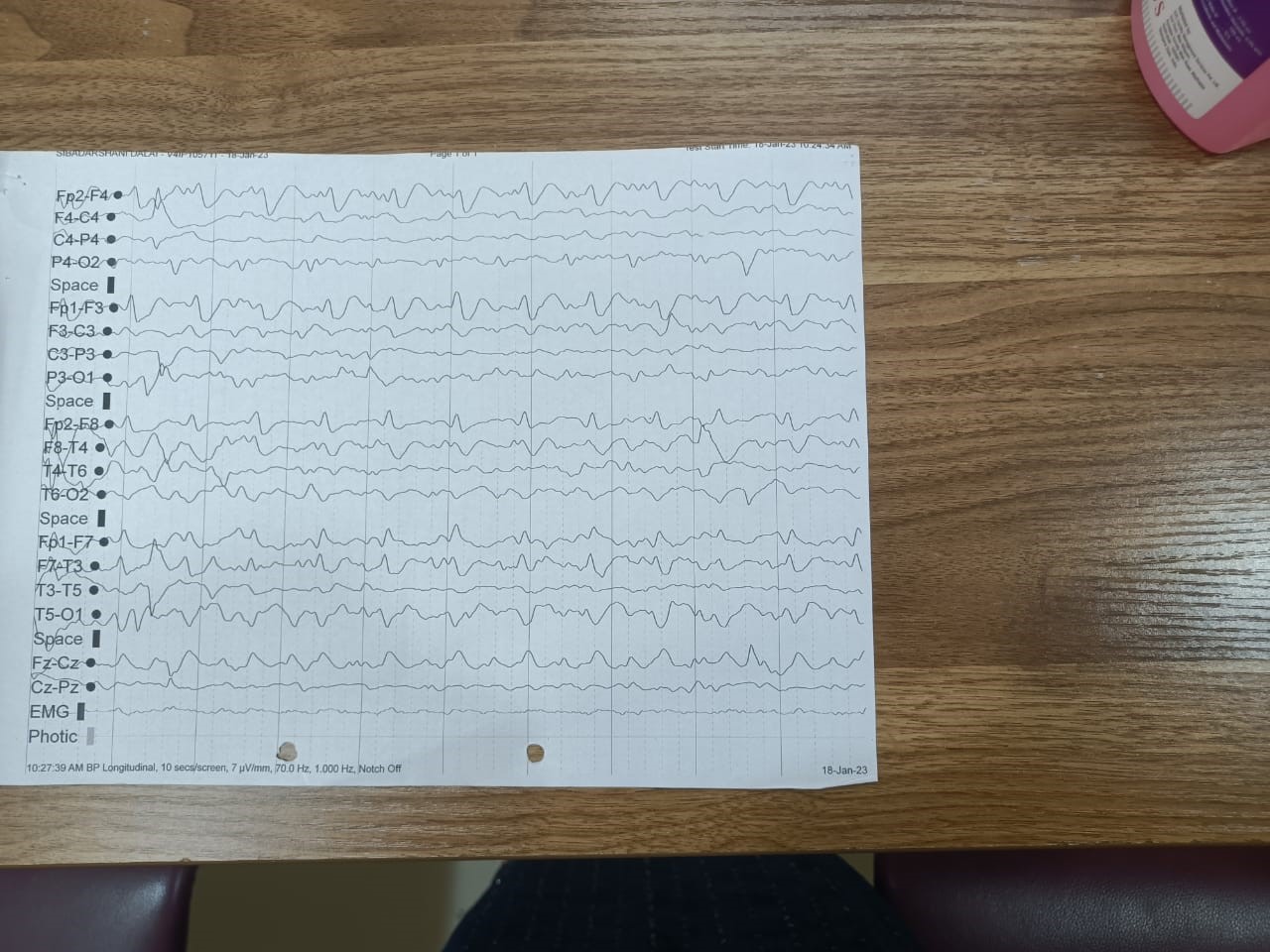
Figure 2: CSF showed postive protein 14-3-3.
2.3 NG/ml. (0 to 0.2 normal range)
Patient has already received Methylprednisolone 1 gm per day for 5 days and now started on IV IG 400mg/kg body weight per day for 5 days. The patient did not show any further improvement. Hence, we considered the diagnosis of Creutzfeldt-Jakob disease of sporadic variant and symptomatic management with Sodium valproate, Levetiracetam, Lacosamide and other supportive medications were started. There was no improvement what so ever and continuous deterioration was there and went in to unconscious state. The patient was discharged as the attendants want to take the patient to their home.
Discussion
The diseases Autoimmune Encephalitis and CJD are quite rare.
Though the topics are quite big enough to discuss we try to review this to the possible extent.
CJD: Occurs 1-2 per million population. It is a prion disease. It is not known how the disease began. It was presumably through Cannibalism of a person with CJD. Women and children are more involved as they consume brain and spinal cord which contains more prions.cessation of ritual of cannibalism eliminated the disease. It was seen in Papua New Guinea along with kuru because of the ritual of Endocannibalism. Non-human spread like beef eating contaminated with BSE is important cause in developing vCJD. CJD is commonly seen in beyond 50 years of age group most of the times. Famillial and variant type of CJDs may be seen in the early age group. There are 4 types of CJD's identified.
- Sporadic -60-80% more common. No apparent reason was identified. May be through spontaneous transformation of the prion protein Prpc into Prsc
- Variant CJD - less common, transmitted through the animal flesh eating which is infected with BSE.
- Genetic CJD - occurs in the early age group and commonly seen in the family members. This comes to about 7.5 percent and has Autosomal dominant inheritance.
The genetic CJD conditions are:
- A) GERSTMANN-STRUSSLER-SCHEINKER SYNDROME (GSS)
- B) FATAL FAMILIAL INSOMNIA.
- Iatrogenic- This occurs most commonly during the surgeries where they do the duroplasty from the affected person and corneal transplant, injection of pituitary growth hormone of infected person and skin transplants from infected people.
Phenotypic Variants1-
- Amyotrophic variant: Amyotrophic lateral sclerosis type of presentation initially.
- Brownell-Oppenheimer variant: Initial presentation is cerebellar ataxia.
- Heidenhain variant: Initial visual symptoms like impaired vision, visual hallucinations, and loss of vision.
- Stern - Garcin variant: Initial extra pyramidal symptoms.
The commom clinical presentation are behavioural disturbances, memory loss which is progressive. The patient may have involuntary movements like dystonia of the limbs, catatonia and incoordination. Some patients may have blurring of vision and blindness. They may have multiple seizures, status epilepticus and more common myoclonic jerks. These patients detoriate fast and they usually die within 1-2years.
Diagnosis:
- The clinical presentation as described above
- CSF analysis which show lymphocytic cellular response, Raised protein and positive protein 14-3'-3. Recently they use t -tau and S 100 β as markers which are more sensitive2.
- Radiological: Hyperintense signals in bilateral ganglionic regions and Ribbon like Hyperintense lesion along fronto parietal and occipital regions along the cortex.Grey matter involvement is very common and probably diagnostic
- Recently CSF and / or olfactory mucosal real time queaking induced conversion seeding assays are more sensitive than 14-3-3 protein.But yet to be evaluated further.
The confusion with Autoimmune encephalopathy and CJD is because of the early clinical manifestations which are similar which we have already discussed. The early identification and evaluation for the antibodies and proper management make the patient do better and survive well.
Autoimmune encephalopathies4: There are several Autoimmune encephalopathies which came into picture in the last 10 years. Some of the auto immune encephalitis are 1. APMDAR 2. LGI 1 3.GABA B R 4.CASPAR 2 5. GABA A R 6. MOG 7. GLYCINE R 8. AMPAR 9. DPPX 10. IGLON 5
The earliest clinical presentation is same in both the conditions making us to confuse in the early clinical diagnosis. Among all these Autoimmune encephalopathies, Hashimoto's Encephalopathy is more common and also called as steroid responsive encephalopathy. All these encephalopathies have common symptomatology but 1-2 symptoms which are specific for AE which should be identified so that diagnosis is made easy. These Autoimmune Encephalitis divided mainly into 2 types
- Tumoral where in AE is associated with a tumor elsewhere and removal of the tumor only can improve the encephalitis.
- Non-Tumoral- Here AE is not associated with any tumor supposed to be idiopathic. Those cases which are not associated with tumor they respond very well to immunotherapy whereas tumoral cases unless otherwise the tumor is removed, they will not respond.
The other end of the spectrum which produce AE is those which have antibodies to intracellular antigens which are tumoral antibodies which respond to removal of the tumor such as anti HU antibodies and the other are extra cellular antigens which produce antibodies to ion channel receptors and other proteins such as NMDA receptors and are non-tumoral and respond well to immunotherapy.
Other types are intermediate antibodies to intracellular synaptic proteins such as GAD65.
The other one is antibodies less clear as in ADEMand Lupus cerebritis.
Clinical clues to recognize autoimmune encephalitis3:
PSYCHOSIS: NMDA R, AMPA R, GABA B R
DYSTONIA AND CHOREA: NMDA R, D2R
HYPER EKPLEXIA: Gly R
STATUS EPILEPTICUS: GABA A and GABA B R.
NEW ONSET DIABETES: GAD65
FACIOBRACHIAL DYSTONIC SEIZURES: LGI 1
NEUROMYOTONIA, FASCICULATIONS, SPASTICITY: CASPR 2.
DIAGNOSIS: 1. Ig G testing should be done both in serum and CSF.The sensitivity is 85%, vs120%.
Lymphocytic pleocytosis and elevated protein are seen.
EEG: Variable.Slowing is commonly seen.
One third develop Deltabrush appearance.
MRI: Usually normal.
May show suble mesial hyppocampal FLAIR hyperintesities and multifocal Grey and white matter hyperintesities.
Treatment: Those patients with nontumoral antibodies positive will respond well to immunotherapy.
This includes
- Methylprednisolone 1 gm daily for 5 days.
- IV Ig 400mg per kg body weight per day for 5 days.
- Plasmapheresis
- Mycophenalate, Azathioprine, Rituximab and cyclophospamide can be as second line drugs.
In the present case the patient has symptomatology common to both AE and CJD which made us to confuse in the early diagnosis. The identification of the TPO antibodies further made us to confuse more with AE. Hence, we treated with Methy prednisolone as there is no response, we have treated with IV IG. As there is progressive deterioration of the sensorium, EEG findings, CSF findings with positive protein 14-3-3 and MRI findings made us to confirm the diagnosis of CJD. Though the brain biopsy is the confirmation it’s difficult procedure in the living and the above three criteria satisfies the diagnosis. Some people suggest Tonsillar biopsy in vCJD cases. We have managed symptomatically. There is improvement in seizure control to some extent but there's progressive deterioration in sensorium and comatosed. As the patient has deteriorated further, she was discharged at request.
Take home message: - Patients presenting with behavioural disturbances, progressive memory impairment, involuntary movements and seizures should be evaluated thoroughly for the presence of autoimmune antibodies and treat accordingly as these patients respond very well to autoimmune therapy in Non-Tumoral cases and removal of the tumor in tumoral cases.
The progressive deterioration of sensorium, positive CSF findings, MRI findings and EEG findings should be considered in the diagnosis of CJD. As this disease has no treatment and succumbs to death in 1-2 years. Symptomatic treatment is the only choice.
References
- Cleveland clinic.
- Prion Diseases: Boonlead tee MD, Michdel D Geshwind MD, Neurology in clinical practice Bradley and Daroffs; 8th edition, 2016; 2: 1432.
- Journal of clinical Neurology, 2016; 12(1): 1-13.
- Christopher EUY, Sophie Binks, Sarosa R Irani. Autoimmune Encephalitis clinical spectrum and management. Practical Neurology, 2023; 21(5).

