Cryptococcal Meningitis in Immunocompetent Patients
Mandela Charles Makakala*
Consultant Internist, Senior Instructor, Internal Medicine Department, Aga Khan University Hospital, Dar es salaam, Tanzania
Received Date: 13/05/2023; Published Date: 01/09/2023
*Corresponding author: Mandela Charles Makakala, Consultant Internist, Senior Instructor, Internal Medicine Department, Aga Khan University Hospital, Dar es salaam, Tanzania
Abstract
Cryptococcal meningitis in immunocompetent and non- HIV patients is rare but important cause of meningitis because of significant morbidity and mortality associated with it. This review of literature has looked at how common is cryptococcal meningitis in immunocompetent patients and described constrasting presentations of cryptococcal meningitis in immunocompetent patiensts in comparison to immunocompromised patients.
Introduction
Cryptococcal meningitis is a sub-acute meningitis causes by inhalation of cryptococcal spores. It is more common in immunosuppression states such as HIV/AIDS with CD4 count of less than 100, malignancy such as lymphoma and leukemia, patients on chemotherapy and immunosuppressant [1]. The most common species are cryptococcal neoformans neoformans, cryptococcal neoformans grubii and cryptococcal gattii [1]. Recently cryptococcal gattii has been implicated in some epidemic cases in immunocompetent patients but there are also some sporadic cases reported in literature [2].
Human gets infected by inhaling the basidiospore which is small desiccated yeast with small polysaccharide capsule which makes it easy to be deposited in the alveoli and terminal bronchioles [3].
In immunocompetent individuals the yeast is engulfed by macrophages forming a small granuloma/hilar lymphadenopathy, in most of the cases the infection is cleared [4]. Some patient develops symptomatic focal pneumonitis presenting with a cough, sputum production, hemoptysis, dyspnea, chest pain, fever, malaise, night sweats, and weight loss [5]. Less commonly the patients may have a rash and gastrointestinal symptoms and very rarely superior vena cava obstruction and Pancoast syndrome due to a granulomatous extension to the apex of the chest wall [6].
In Immunocompromised individuals such as stem cell and solid organ transplantation, HIV infection, malignancies, cirrhosis, renal failure, chronic lung, Cushing's syndrome, sarcoidosis, and treatment with glucocorticoids or tumor necrosis factor-alpha antagonists reactivation of latent infection may occur and result in disseminated extra pulmonary infection to the skin and central nervous system [7,8].
Cutaneous manifestations are seen in 15% of patients with disseminated infection; which present as papules, plaques, purpura, ulcers, cellulitis, superficial plaques, abscesses, and sinus tracts [9].
Dissemination to the central nervous system will cause inflammation of the meninges, brain matter and granuloma formation in the brain parenchyma resulting in acute and subacute meningoencephalitis symptoms like fever, headache, vomiting, altered mentation and convulsions [7].
In Sub Saharan Africa majority of cryptococcal meningitis cases are HIV/AIDS associated due to burden of disease in this regions. Due to very low CD4+ T cells in HIV the individuals the immune system makes memory T- cells without exaggerated immune response. When the patients are initiated on ARV CD4+ cell increase and are activated through the memory cell to produce cytokines mostly interleukin-6(IL6), Interferon gamma (IFNγ) and TNF causing cryptococcal immune reconstitution syndrome (cIRIS) [10].
But because there is a direct synapse of Activated T-cells and macrophages in HIV positive individuals this results in a better antigen clearance compared to HIV negative individuals. In contrast, the HIV negative individuals with the cryptococcal infection present with a similar inflammatory response just after acquiring the infection termed as Cryptococcal post-infectious immune response syndrome (cPIIRS) [10].
The objective of this review is to describe the proportion of cryptococcal meningitis in immunocompetent patients, compare clinical presentation between immucompetent cases and immunocompromised cases and prognosis of infection. The knowledge of the difference in presentations between the two groups may guide management of cryptococcal meningitis.
Methodology
We searched in PUBMED data base using the following search terms “((((cryptoccocal[All Fields] AND ("infection"[MeSH Terms] OR "infection"[All Fields])) OR ("meningitis, cryptococcal"[MeSH Terms] OR ("meningitis"[All Fields] AND "cryptococcal"[All Fields]) OR "cryptococcal meningitis"[All Fields] OR ("cryptococcal"[All Fields] AND "meningitis"[All Fields]))) OR (("cryptococcus"[MeSH Terms] OR "cryptococcus"[All Fields] OR "cryptococcal"[All Fields]) AND gatii[All Fields])) AND (Immunocompetent[All Fields] AND ("patients"[MeSH Terms] OR "patients"[All Fields]))) AND "immunocompetence"[MeSH Terms]
Results
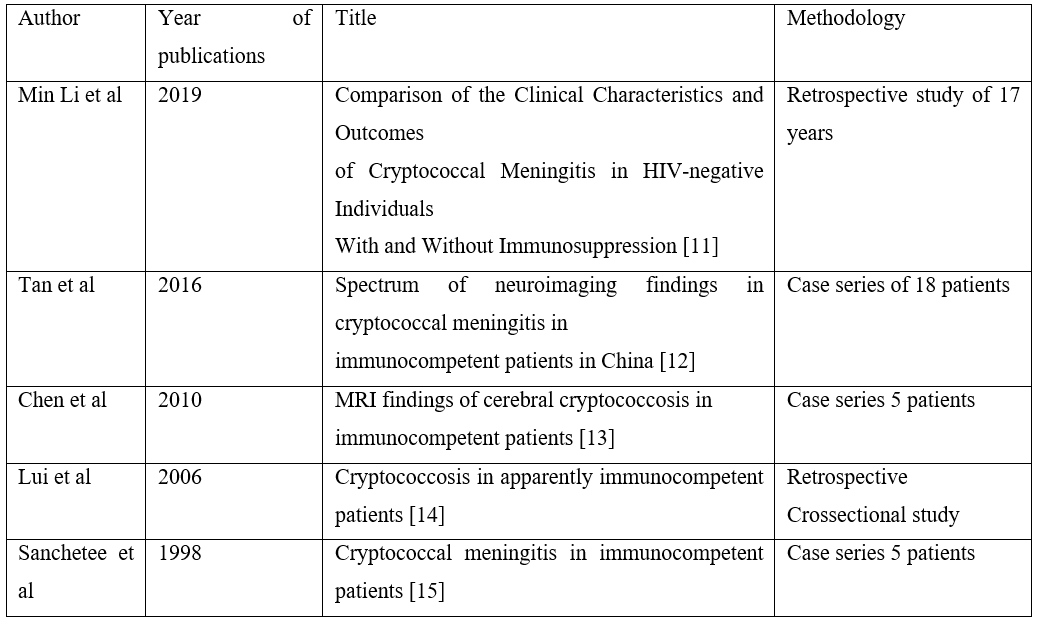
31 articles were found to be related to cryptococcal meningitis in immunocompetent patients, two were review articles, 24 were case reports. Five articles remaining were includes for this review as showed in the Table 1.
Question 1. How common is cryptococcal meningitis in immunocompetent patients?
In a retrospective study of 255 cryptococcal meningitis china, a record review of 17 years; 91 (35.7%) appeared immunocompetent [16]. This results were not far off from a retrospective case series done of 46 patients done in Hong Kong where twenty patients (43.5%) were apparently immunocompetent [14].
Question 2. Is there a difference in clinical presentation of CM between Immunocompetent and Immunocompromised patients?
Cryptococcal meningitis in Immunocompetent patients were found to be significantly younger compared to immunocompromised patients (above 50 y, 19.8% vs. 32.3%, P=0.026) [11]. Immunocompetent have more symptoms of meningitis (80.0% vs. 47.1%, p=0.03), visual symptoms and auditory symptoms (45.1% vs. 27.4%, P=0.004; 19.8% vs. 9.1%, P=0.016) respectively [11,14]. Immunocompetent patients had longer mean time from illness onset to presentation (34.4 vs. 12.6 days, p=0.02) [14].
Both Min Li et al and Lui et al found higher WBC in CSF of immunocompetent patients compared to immunocompromised patients, (30.8% vs. 45.1%, P=0.009) and (white blood cells 108 vs. 35x109/l, p=0.03) in their respective study.
Question 3. What are the common radiological findings of CM in immunocompetent patients?
Immunocompetent patients with CM were more likely to have a normal MRI compared to immunocompromised patients (10% vs. 2%, P=0.028) [11]. A retrospective series of 18 cases revealed radiological finding in 16 patients; that included multiple intraparenchymal lesions with or without enhancement, prominent basal ganglia involvement, miliary distribution of parenchymal nodules, multiple dilated Virchow-Robin spaces and leptomeningeal enhancement and six out of 18 patients had venticulomegaly [12].
Question 4. What is the outcome of CM in immunocompetent patients?
Min Li et al showed that both groups of patient CM in immunocompetent and immunocompromised had high mortality mortality 10.9% vs. 7.0%, P=0.416, but there was no significant difference between the two groups. This was similar to another study that found a mortality of 25.0% vs.52.9%, p= 0.06 [11].
Table 1: Summary of studies
Discussion
There is significant paucity of data on cryptococcal meningitis in immunocompetent patients and the studies that were done are retrospective crossectional studies/case series with small sample size. This entails that cryptococcal meningitis in Immunocompetent rare . Although in the two retrospective studies reviewed, proportion of cryptococcal meningitis in immunocompetent patients is only slightly less compared to immunocompromised patients. There for screening for CM in immunocompent patients with insidious development of symptoms and signs of meningitis is important.
Immunocompetent patients seems to be more symptomatic compared immunocompromised patients this is probably because of high inflammatory response compared to immunosuppressed patients. This suggest that there might be a role of steroids in immunocompetent patients with CM to reduce inflammation.
Cryptococcal meningitis in immunocompetent patients with CM has vast variety of radiological findings which may look like other presentations like brain mass, TB, vasculitis. So imaging alone without culture or serological is not enough to make a diagnosis. Lumber puncture is crucial in the diagnosis. There is no difference between outcomes in these two groups, therefore clinicians should be aggressive in managing patient with CM in immunocompetent group.
Conclusion
Cryptococcal meningitis in immunocompetent patients is a rare presentation of subacute meningitis; a patient with signs of meningitis his CSF should always be screened for cryptococcal meningitis. There are more signs of inflammation in immunocompetent patients this might suggest importance of steroids in management of CM in immunocompetent to reduce the inflammatory response in in the early treatment phase. There is no significance difference in mortality between the two groups. We need further studies in this area to understand better CM in immunocompetent patients.
Conflict of Interest: None
Authors contribution: Dr. Mandela Charles Makakala is the main author of the article.
References
- Hill C, Jain A, Takemoto H, Silver MD, Nagesh SVS, Ionita CN, et al. Expanding fungal pathogenesis: Cryptococcus species break out of the opportunistic box. Proc SPIE--the Int Soc Opt Eng, 2015; 73(4): 389–400.
- Saul N, Krockenberger M, Carter D. Evidence of Recombination in Mixed-Mating-Type and -Only Populations of Cryptococcus gattii Sourced from Single Eucalyptus Tree Hollows. Eukaryot Cell [Internet]. 2008; 7(4): 727–734.
- EMMONS CW. Saprophytic sources of Cryptococcus neoformans associated with the pigeon (Columba livia). Am J Hyg, 1955; 62(3): 227–232.
- Campbell GD. Primary pulmonary cryptococcosis. Am Rev Respir Dis, 1966; 94(2): 236–243.
- Shirley RM, Baddley JW. Cryptococcal lung disease. Curr Opin Pulm Med [Internet]. 2009; 15(3): 254–260.
- Mitchell DH, Sorrell TC. Pancoast’s syndrome due to pulmonary infection with Cryptococcus neoformans variety gattii. Clin Infect Dis, 1992; 14(5): 1142–1144.
- Pappas PG, Perfect JR, Cloud GA, Larsen RA, Pankey GA, Lancaster DJ, et al. Cryptococcosis in human immunodeficiency virus-negative patients in the era of effective azole therapy. Clin Infect Dis, 2001; 33(5): 690–699.
- Cameron ML, Bartlett JA, Gallis HA, Waskin HA. Manifestations of pulmonary cryptococcosis in patients with acquired immunodeficiency syndrome. Rev Infect Dis, 2018; 13(1): 64–67.
- Mitchell TG, Perfect JR. Cryptococcosis in the era of AIDS--100 years after the discovery of Cryptococcus neoformans. Clin Microbiol Rev, 1995; 8(4): 515–548.
- Williamson PR, Jarvis JN, Panackal AA, Fisher MC, Molloy SF, Loyse A, et al. Cryptococcal meningitis: epidemiology, immunology, diagnosis and therapy. Nat Rev Neurol, 2017; 13(1): 13–24.
- Li M, Chen Z, Xu L, Gan Z, Peng F, Liu J. A Comparison of the Clinical Characteristics and Outcomes of Cryptococcal Meningitis in HIV-negative Individuals With and Without Immunosuppression. Neurologist, 2019; 24(1): 1–5.
- Tan Z-R, Long X-Y, Li G-L, Zhou J-X, Long L. Spectrum of neuroimaging findings in cryptococcal meningitis in immunocompetent patients in China — A series of 18 cases. J Neurol Sci, 2016; 368: 132–137.
- Chen S, Chen X, Zhang Z, Quan L, Kuang S, Luo X. MRI findings of cerebral cryptococcosis in immunocompetent patients. J Med Imaging Radiat Oncol, 2011; 55(1): 52–57.
- Lui G, Lee N, Ip M, Choi KW, Tso YK, Lam E, et al. Cryptococcosis in apparently immunocompetent patients. QJM, 2006; 99(3): 143–151.
- Sanchetee P. Cryptococcal meningitis in immunocompetent patients. J Assoc Physicians India, 1998; 46(7): 617–619.
- Li M, Chen Z, Xu L, Gan Z, Peng F, Liu J. A Comparison of the Clinical Characteristics and Outcomes of Cryptococcal Meningitis in HIV-negative Individuals With and Without Immunosuppression. Neurologist, 2019; 24(1): 1–5.

