A Mini Review in Opioid‑Induced Constipation
Fawaris FF1 * and Rufaida I2
1Departmnet of Nursing, Nurse Educator at King Hussein Cancer Center, Amman, Jordan
2Departmnet of Nursing, Quality Nurse, Ministry of health Amman, Jordan
Received Date: 18/07/2020; Published Date: 31/07/2020
*Corresponding author: Fadi F Fawaris, Department of Nursing, Clinical Nurse Educator at King Hussein Cancer Center, Amman, Jordan. Tel: 00962780373897; E-Mail: Fadi862005@yahoo.com, ORCID ID: https://orcid.org/0000-0001-8461-3733
Abstract
Patients using opioids to treat chronic cancer and non-cancer pain are frequently experiencing burden side effects that may distress patients' quality of life. These side effects include opioid induced constipation. Despite of the number of treatment guidelines, the treatment regularly wasn't established well.
Keywords: Opioid-Induced Constipation; Opioids; Constipation; Patient-Experience
Introduction
The opioids are commonly prescribed in the treatment of chronic pain in the past decade. Chronic pain occurs in association with cancer and non-cancer Conditions. Prescription opiate use has increased severely in several parts of the United States in the last period it has been estimated that 20% of people experiencing pain problems at medical clinics in the United States were given opioids [1] (Figure 1). Opioid induced constipation (OIC) is a wide spread burden side effect and impaired quality of life among patients using chronic opioids [2]. Opioids have pharmacological effect through the gastrointestinal tract, it is characterized by constipation, less than three bowel movement per week and hard stool than normal, it also may associated with pain, discomfort, sensation of incomplete evacuation, anorexia, nausea and insomnia [3].
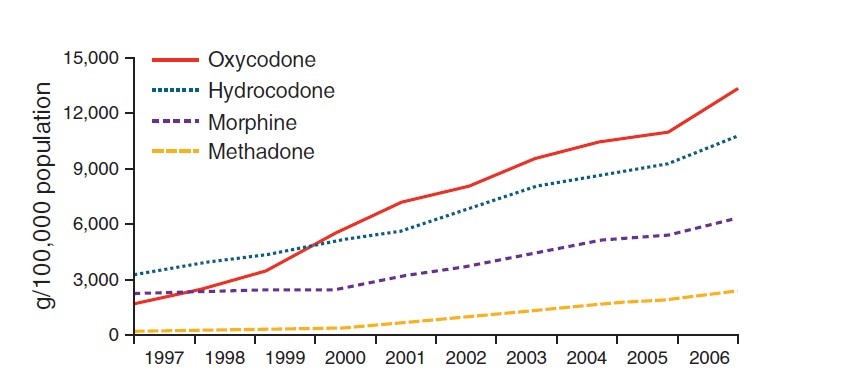
Figure 1: Therapeutic opioid use in the United States (g / 100,000 population) from 1997 to 2006.
Three types of receptors for opioid peptides have been recognized as having effects on human gastrointestinal function: δ -, κ -, and μ -receptors. They all fit to the family of G-protein-coupled receptors, and inhibit adenylate cyclase. At the membrane level, they reduce neuronal excitability and neurotransmitter (acetylcholine) release with an overall inhibitory effect on the neuron. In the gastrointestinal tract, μ -receptors are extensively distributed in the submucosa, in addition to in the ilea mucosa where they impact ion carriage changes .Stomach and proximal colon have the greatest dense μ - and κ -opiate receptors [4].
The impact of constipation in opioid consumers is multidimensional. Opioids interact with normal gastrointestinal motility by delaying movement, activating non propelled motility, segmentation and Tone and relaxation of sphincters throughout their effects on enteric neurons [5].
The prevalence of opioid-induced constipation (OIC) in populations with advanced cancer ranges between 25% and 90% [6]. In prospective cross-sectional descriptive study of 156 patients attending a newly organized pain and palliative care clinic result revealed that constipation prevalence was 31.4 % while pain prevalence was 100% which palliated by opioid administration. More and more using of opioid it result in high prevalence of opioid induced bowel disorder (OBD), result of 146 chronic non cancer pain patients showed that most common symptoms of OBD was constipation (46.9%), nausea (27%), vomiting (9%), and gastro-esophageal reflux disease (33%). It was associated with prolonged used of opioid not with dose of opioid in other hand study indicated that there is no effect of constipation on heath related quality of life [7].
One multinational internet survey of 322 palliative patients revealed that OBD occurs frequently despite the use of laxative, patient experience, constipation (81%), straining (58%), fatigue (50%), small or hard stool movement (50%) and insomnia all these symptoms had at least moderate negative impact on patients quality of life, more over one third of the patient had missed, deceased or stopped using of opioid in order to relieve constipation [8].
Screenings of OIC in palliative unit depend on many criteria, in one descriptive, multicenter cross sectional study of one hundred twenty palliative patient aimed to establish screening criteria for constipation in palliative unit; researchers found that constipation should be assessed and screen as a syndrome not as a symptoms; signs and symptoms, also frequency and consistency, should be assessed, more over associated symptoms could be quantify. Participants experienced associated symptoms such as; pain, discomfort and sensation of incomplete evacuation [6].
Other retrospective study of 8836 cancer patients revealed that OIC impact patient decision related the use of opioid, recourse utilization and cost as they need more visits to clinic in order to solve OIC and its associated symptoms. In other dimension; qualitative research aimed to understand psychological distress and burden associated with OIC and its treatments in twelve advanced cancer patients, researcher found that patients had irrational thoughts about nutrition and its relation with OIC also they though that constipation is an indication of heath deterioration, more over patients experienced depressive and anxiety symptoms related to constipation, also results confirm pervious results that constipation affect decision about using opioids [6]. Many articles in literature studied patients experiences with irritable bowel syndrome, results of qualitative study indicated that patients living with unpredictability, they need to planning and organizing everything in order not to loss control over their bowel symptoms [9,10], also they experience dignity preserving specially in social activity and in their work place, moreover physical suffering (stuffiness, fatigue, sleeplessness and pain) made their experience more trouble [11].
Many alternatives management method of opioid induced constipation are in use, one literature review of u-opioid antagonist indicated that Methylnaltrexone, Naloxone, Naldemedine [12] and Naloxegol, and Lubiprostone may help in decrease from intense discomfort that result from constipation [11,12]. Recent guidelines recommend fluid and fiber intake and a laxative treatment with the beginning of opioid therapy. Nevertheless, as laxatives do not determine the causal of OIC, constipation, and straining to pass a bowel movement might still be observed in patients receiving laxative therapy.
Conclusion
Despite increasing understanding of the opioid induced constipation there is lake of systematic research on patient experience living with OIC. Actually the first step to meet patients with OIC needs is to understanding of how they living with OIC.
In summary, there is a need for qualitative research that is directed at gaining understanding about the lived experience of adult the living experience of adult palliative patients living with OIC.
References:
- US Drug Enforcement Administration Automation of Reports and Consolidated Orders System (ARCOS); ( www.deadiversion.usdoj.gov/ arcos/retail_drug_summary/index.html ).
- Fredericks A, Hollis G, Stricker C. Diagnosis and management of opioid-induced bowel dysfunction in patients with advanced cancer. Clin J Oncol Nurs [Internet]. 2010;14(6):701-4. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L360274905%5Cnhttp://sfx.library.uu.nl/utrecht?sid=EMBASE&issn=1538067X&id=doi:&atitle=Diagnosis+and+management+of+opioid-induced+bowel+dysfunction+in+patients+with+advanced+cancer.&st.
- Camilleri M. Opioid-Induced Constipation: Challenges and Therapeutic Opportunities. Am J Gastroenterol [Internet]. 2011;106(5):835-42. Available from: http://journals.lww.com/00000434-201105000-00008.
- Farmer AD, Drewes AM, Chiarioni G, De Giorgio R, O’Brien T, Morlion B, et al. Pathophysiology and management of opioid-induced constipation: European expert consensus statement. United Eur Gastroenterol J. 2019;7(1):7-20.
- Blair HA. Naldemedine: A Review in Opioid-Induced Constipation. Drugs [Internet]. 2019;79(11):1241-7. Available from: https://doi.org/10.1007/s40265-019-01160-7.
- Dhingra L, Shuk E, Grossman B, Strada A, Wald E, Portenoy A, et al. A qualitative study to explore psychological distress and illness burden associated with opioid-induced constipation in cancer patients with advanced disease. Palliat Med. 2013;27(5):447-56.
- Lal M, Raheja S, Kale S, Das N, Gogia A, Bhowmik K. An experience with 156 patients attending a newly organized pain and palliative care clinic in a tertiary hospital. Indian J Cancer. 2012;49(3):293-7.
- Clark K, Hipwell A, Byfieldt N. A retrospective pilot study to explore the timing of cessation of laxatives before death in a palliative care unit. Int J Palliat Nurs. 2012;18(7):326-30.
- Keller MS, Jusufagic A, Spiegel BMR. Patient and provider differences in the treatment of opioid-induced constipation: a qualitative study. BMC Gastroenterol. 2019;19(1):182.
- Farmer AD, Drewes AM, Chiarioni G, De Giorgio R, O’Brien T, Morlion B, et al. Pathophysiology and management of opioid-induced constipation: European expert consensus statement. United Eur Gastroenterol J. 2019;7(1):7-20.
- Crockett SD, Greer KB, Heidelbaugh JJ, Falck-Ytter Y, Hanson BJ, Sultan S. American Gastroenterological Association Institute Guideline on the Medical Management of Opioid-Induced Constipation. Gastroenterology [Internet]. 2019;156(1):218-26. Available from: https://doi.org/10.1053/j.gastro.2018.07.016.
- Blair HA. Naldemedine: A Review in Opioid-Induced Constipation. Drugs [Internet]. 2019;79(11):1241–7. Available from: https://doi.org/10.1007/s40265-019-01160-7.

