Pityriasis Lichenoides et Varioliformis Acuta : An Atypical Presentation
Mejjati Kaoutar1,*, Douhi Zakia1, Soughi Meryem1, Elloudi Sara1, Baybay Hanane1, Layla Tahiri Elousrouti2 and Mernissi Fatima Zahra1
1Department of Dermatology, University Hospital Hassan II, Morocco
2Pathology Department, University Hospital Hassan II, Morocco
Received Date: 03/11/2023; Published Date: 10/04/2024
*Corresponding author: Kaoutar Mejjati, Department of Dermatology, University Hospital Hassan II, Fez, Morocco
Keywords: Pityriasis lichenoides et varioliformis acuta; Dermoscopy, Lichenoid pattern
Sir,
Pityriasis lichenoides is a group of inflammatory skin conditions that includes pityriasis lichenoides and varioliformis acuta (PLEVA) and chronic pityriasis lichenoides [1].
Pityriasis lichenoides et varioliformis acuta (PLEVA) is a rare inflammatory dermatosis of the young adults, with a sudden onset and a mostly spontaneous favorable evolution.
Although the etiology of PLEVA is unknown, it is probably an inflammatory reaction to foreign microorganisms such as infectious agents and drugs [2].
Clinically, PLEVA manifests as an acute eruption of small erythematous to brown macules evolving into papules topped by hemorrhagic crusts, by flare-up and remission.
Dermoscopy plays an important orienting role. The lesions are divided in two: early aspect of brownish amorphous zone, white scales, and dotted vessels in periphery. And lesions in late phase with structureless white areas in the center, glomerular and dotted vessels in periphery [3].
Treatment options are not codified; include phototherapy, oral antibiotics, dermocorticoids, and antihistamines [4,5]. Systemic therapies such as corticosteroids, methotrexate, cyclosporine, and retinoids may be warranted in severe manifestations of PLEVA resistant to conventional treatments.
Remission is complete, however, an evolution towards a hematoderma was reported, hence the interest of a prolonged follow-up of the patients.
Herein, we report a case of a patient who presented PLEVA.
Mrs R, 51 years old, with a history of arterial hypertension under treatment and vitiligo, presented with a 2 years history of a generalized rash evolving in flare ups and remission for 2 years. The patient denied any new medications, infection or vaccination. The dermatological physical exam showed multiple rounded umbilical papules, with haemorrhagic crusts, confluent for some in small patches, symmetrically located on the lower limbs, buttocks, abdomen and upper limbs (Figure 1A). The examination of the mucous membranes was normal. The lymph nodes were free, without hepatosplenomegaly, infectious signs or alteration of the general state
Dermoscopy revealed an erythematous background, and bright whitish structures in favor of wickham’s striae (Figure 1B et 1C).
Skin biopsy showed staggered apoptotic cells with parakeratosis and major lymphocytic exocytosis scattered throughout the epidermis. The dermis was the site of a predominantly lymphocytic infiltrate fanning out towards the epidermis (Figure 2). The immunohistochemical complement excluded any sign of mycosis fungoides.
The findings were consistent with a clinical diagnosis of PLEVA. A complete remission was noted after 3 weeks with dermocorticoids.
The originality of our observation lies in the presence of a previously undescribed lichenoid network on dermoscopy. Further studies of dermoscopy of lichenoides pityriasis may be beneficial to increase diagnostic confidence.
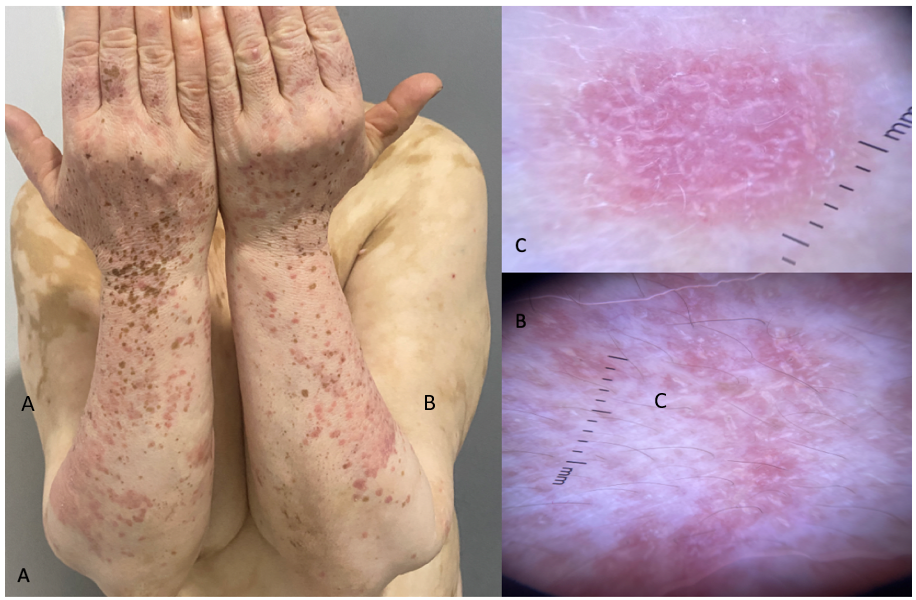
Figure 1: (A) Erythematous papules with fine scaling (B)(C) : Dermoscopy: Wickham striae on erythematous background.
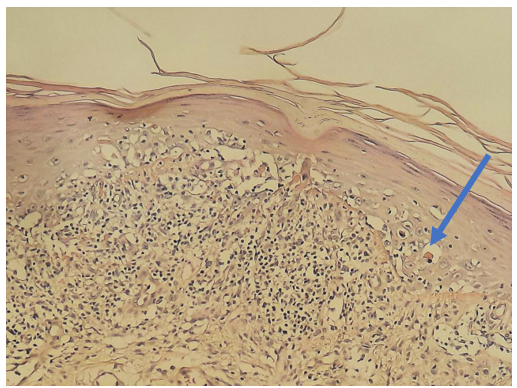
Figure 2: Epidermis with lymphocytic exocytosis and presence of staged apoptotic cells (arrow) with parakeratosis (HESx100).
Consent: The examination of the patient was conducted according to the Declaration of Helsinki principles.
Conflicts of interest: The authors do not declare any conflict of interest.
References
- Bowers S, Warshaw EM. Pityriasis lichenoides and its subtypes. Am. Acad. Dermatol, 2006; 55: 557–572.
- Fernandes NF, Rozdeba P, Schwartz RA, Kihiczak G, Lambert WC. Pityriasis lichenoides et varioliformis acuta: A disease spectrum. J. Dermatol, 2010; 49: 257–261.
- Lacarrubba F, Micali G. Dermoscopy of pityriasis lichenoides et varioliformis acuta. Arch Dermatol, 2010; 146(11): 1322.
- Bellinato F, Maurelli M, Gisondi P, Girolomoni G. A systematic review of treatments for pityriasis lichenoides. J. Eur. Acad. Dermatol. Venereol, 2019; 33: 2039–2049.
- Di Costanzo L, Balato N, La Bella S, Balato A. Successful association in the treatment of pityriasis lichenoides et varioliformis acuta. J. Eur. Acad. Dermatol. Venereol, 2009; 23: 971–972.

