Eyebrow and Eyelash Alopecia Areata: Clinical Insights, Trichoscopic Features, and Nail Associations
Bouayad Khalil*, Hanane Baybay, Hanae Boumaaza, Meryem Soughi, Zakia Douhi, Sara Elloudi, Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II of Fez, Morocco
Received Date: 04/05/2025; Published Date: 11/06/2025
*Corresponding author: Bouayad Khalil, Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Abstract
Background: Alopecia areata (AA) is a common autoimmune disorder that primarily affects the scalp, but eyelash and eyebrow involvement, as well as nail changes, are less frequently studied.
Objective: to investigate the specific characteristics of eyelash and eyebrow involvement across different forms of alopecia areata, to analyze the trichoscopic features associated with these manifestations, and to explore the potential relationship between nail involvement and the presence of alopecia affecting the eyelashes and eyebrows.
Methods: This descriptive study was conducted at the dermatology department of the university hospital Hassan II in Fez over a 2-year period (May 2022 to May 2023). A total of 124 patients with clinically and dermoscopically confirmed AA were included. Eyelash and eyebrow involvement, trichoscopic findings, and nail changes were evaluated.
Results: Eyebrow involvement was observed in 68% of cases (84/124), and eyelash involvement in 50% (62/124). Severe AA (SALT ≥ 50%) was present in 76% of patients. Eyelash and eyebrow involvement was the main reason for consultation in 13% of cases. A strong correlation was found between eyebrow severity (ClinRO grades 2/3) and increasing SALT scores: 42% of patients with SALT 50–74, 60% with SALT 75–94, and 88% with SALT 95–100 had significant gaps or complete eyebrow loss. Nail changes were observed in 59% of patients, with pitting (23%) and trachyonychia (21%) being the most common findings. Trichoscopic markers of active disease included black dots (79%), bent hairs (67%), and exclamation mark hairs (32%). Combined involvement of eyelashes, eyebrows, and nails was noted in 45% of patients, underscoring the widespread nature of the disease.
Conclusion: Eyelash, eyebrow, and nail involvement are important clinical indicators of disease severity in AA and may reflect underlying systemic immune dysregulation. Recognizing these patterns can aid in early diagnosis, guide therapeutic decisions, and improve patient outcomes by addressing both clinical and psychosocial aspects of the disease.
Keywords: Alopecia areata; Eyebrow involvement; Eyelash alopecia; Trichoscopy; Nail abnormalities
Introduction
Alopecia Areata (AA) is a common autoimmune disorder characterized by non-scarring hair loss. While scalp involvement is well-documented, eyelash and eyebrow involvement remain understudied. These areas play crucial roles in facial aesthetics, emotional expression, and ocular protection. This study aims to:
- Describe the specific features of eyelash and eyebrow involvement in different forms of AA.
- Analyze trichoscopic patterns associated with this involvement.
- Explore the relationship between nail, eyelash, and eyebrow involvement in AA.
Materials and Methods
This descriptive study was conducted in the dermatology department of CHU Hassan II in Fès over a 2-year period (May 2022 to May 2023). Patients with a confirmed diagnosis of AA based on clinical and dermoscopic criteria were included. The study focused on evaluating eyelash and eyebrow involvement, trichoscopic features, and associated nail changes.
Results
The study comprised 124 patients with alopecia areata (AA), with a male-to-female ratio of 0.6 (indicating female predominance). The mean age was 22.9 years (range: 2–77), with nearly equal distribution between adults (48%) and pediatric patients (51%). Clinical subtypes included alopecia totalis (3%), patchy AA (42%), ophiasis-type AA (6%), and alopecia universalis (44%).
Eyebrow and/or eyelash involvement was the primary reason for consultation in 13% of cases (n=16/124). Among patients with AA:
- 62 cases (63.9%)exhibited bilateral involvement of both eyebrows and eyelashes.
- 22 cases (22.7%)had isolated eyebrow involvement (no eyelash involvement).
- No casespresented with isolated eyelash involvement.
- Unilateral involvement(limited to one side) was observed in 13 cases (13.4%). (Figure 1).
The severity of Eyebrow and Eyelash Involvement was graded using the Clinician-Reported Outcome (ClinRO) scale (range: 0–3). The distribution of severity scores was as follows:
- Score 1(minimal hair loss with regular distribution): 6% of cases.
- Score 2(significant hair loss or irregular distribution): 2% of cases.
- Score 3(complete absence of visible hair): 9% of cases.
Severity of Alopecia and Hair Loss Patterns
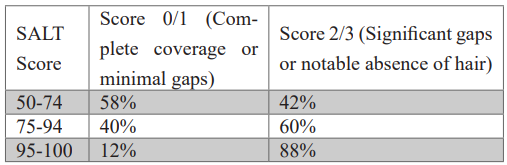
The Severity of Alopecia Tool (SALT) revealed 24% of patients (n=30) had mild-to-moderate hair loss (SALT <50%), while 76% (n=94) exhibited severe hair loss (SALT ≥50%) (Figure 3). A significant association was observed between eyebrow hair loss severity (ClinRO scores) and SALT categories (Table 1):
- SALT 50–74%: 58% of patients had ClinRO score 0/1 (minimal gaps) vs. 42% with score 2/3 (significant gaps).
- SALT 75–94%: 40% scored 0/1 vs. 60% scored 2/3.
- SALT 95–100%: Only 12% scored 0/1 vs. 88% scored 2/3 (p<0.001).
Table 1: Association between SALT Scores and Eyebrow Hair Loss Severity (ClinRO).
Nail Involvement
Nail changes were present in 59% (n=74) of patients
Dermoscopic nail abnormalities included (Figure 5) :
- Pitting (23%), trachyonychia (21%), and leukonychia (17%).
- Rare findings: lunular erythema (4%), scaly cuticle (8%), and longitudinal striations (6%).
Co-occurrence of nail and eyebrow/eyelash involvement was noted in 45% (n=56) of patients.
Nail Changes Stratified by Eyebrow/Eyelash Severity (ClinRO) (table 2):
- Pitting(46% with ClinRO 0/1 vs. 68% with ClinRO 2/3) and trachyonychia (28% vs. 32%) were most common (Table 2).
- Leukonychiawas observed in 29% of mild cases (ClinRO 0/1) vs. 24% of severe cases (ClinRO 2/3).
Table 2: Nail Changes Stratified by Eyebrow/Eyelash Severity (ClinRO).
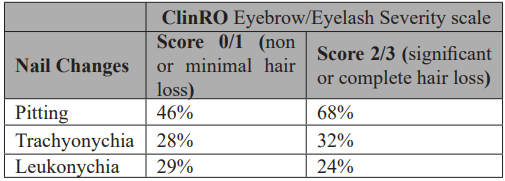

Figure 1: Eyebrow and/or eyelash involvement in patients with AA.
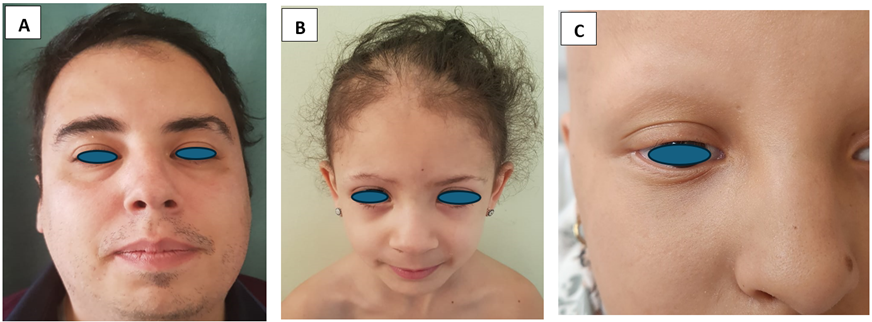
Figure 2: The severity of Eyebrow and Eyelash Involvement using the Clinician-Reported Outcome (ClinRO) scale. A: score 1 B: score 2 C: score 3.

Figure 3: The Severity of Alopecia Tool (SALT) A: SALT <50%. B: SALT ≥50%.
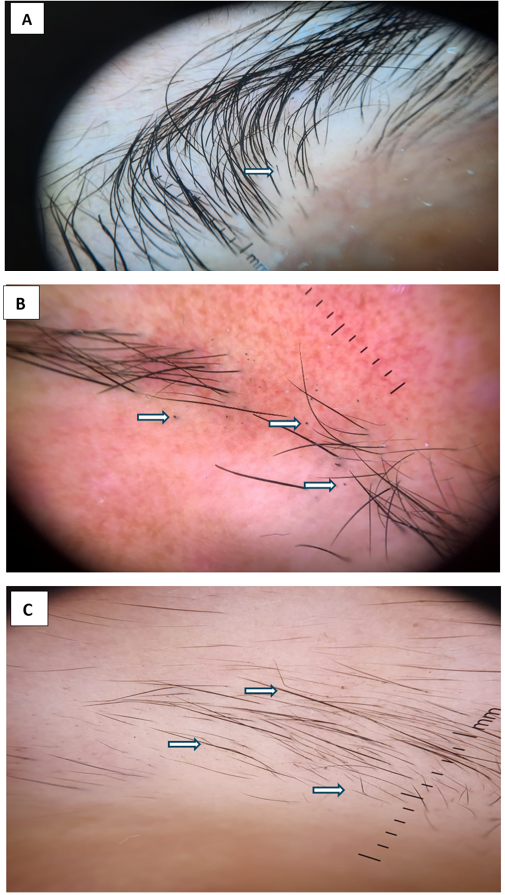
Figure 4: trichosopic finding: A: exclamation mark hair B: Black dots C: Bent hairs.

Figure 5: Nail dermoscopy: A: Trachyonychia B: Pitting C: Leuconychia.
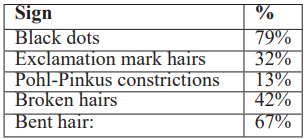
Trichoscopic Findings:
Trichoscopy revealed active disease markers (Table 3):
- Black dots (79%), bent hairs (67%), and yellow dots (67%) were predominant.
- Exclamation mark hairs (32%) and Pohl-Pinkus constrictions (13%) were less frequent.
Table 3: Trichoscopic Findings.
Discussion
Eyebrows and eyelashes serve critical protective and psychosocial functions beyond aesthetics. While their loss (madarosis) profoundly impacts non-verbal communication and quality of life. In AA, madarosis induces significant emotional distress. Their multifunctional role underscores because even partial loss warrants clinical attention.
Our study highlights critical limitations of the Severity of Alopecia Tool (SALT), which remains the most widely used metric for assessing AA severity. While SALT effectively quantifies scalp hair loss (e.g., 76% of our patients had SALT >50%), it fails to characterize the multidimensional clinical spectrum of AA severity
For instance, our cohort exhibited frequent eyebrow/eyelash involvement (67% of cases) and likely significant psychosocial burden—factors not captured by SALT.
These shortcomings align with recent critiques by King et al. [1], who proposed the Alopecia Areata Scale (AAS) as a pragmatic alternative. The AAS integrates the Scalp involvement (similar to SALT), Extra-scalp manifestations (e.g., eyebrows, eyelashes), Treatment response history, Rapid/diffuse progression, and the psychosocial impact.
Eyebrow/eyelash severity assessment benefits from combining both ClinRO (clinician-reported) and PRO (patient-reported outcomes) [2]. Recent advances, such as the Brigham Eyebrow Tool for Alopecia (BETA) and Brigham Eyelash Tool for Alopecia (BELA), were developed to quantitatively assess progression of AA-related eyebrow and eyelash involvement [3]. Despite their utility, routine clinical application remains challenging due to practical limitations.
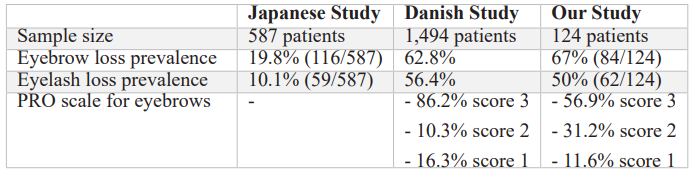
Our results demonstrate a higher prevalence of eyebrow (67%) and eyelash (50%) involvement compared to the Japanese reports [4], but align closely with Danish finding [5] (table 4). Highlighting the possible role of geographic/ethnic factors in AA evaluation.
Table 4: Comparative prevalence of eyebrow/eyelash involvement and severity scores across studies.
PRO: Patient-Reported Outcome. Severity scores range from 1 (mild) to 3 (complete hair loss).
Our trichoscopic findings of black dots (79%), bent hairs (67%) and exclamation mark hairs (32%) are frequent finding of alopecia areata (AA), distinguishing it from other causes of eyebrow/eyelash alopecia. Unlike frontal fibrosing alopecia (FFA), which shows dystrophic hairs, hair growing in different directions and white scarred areas, or infectious etiologies like tinea faciei (corkscrew/comma hairs), AA's trichoscopic profile reflects its non-scarring, inflammatory nature. These features are critical for differential diagnosis, as treatment varies significantly [6].
Consistent with established literature, pitting (46–68%) and trachyonychia (28–32%) represented the predominant dermoscopic abnormalities in our study. These align with Chelidze & Lipner’s (2018) review, which identifies pitting and trachyonychia as hallmark features of AA-associated nail disease. Their frequent co-occurrence with eyebrow/eyelash involvement (45%) reinforces their clinical utility as markers of extensive disease, particularly in universalis/totalis subtypes. these findings should prompt closer disease monitoring and consideration of early systemic therapy.
Conclusion
Our study highlights the high prevalence of eyebrow and eyelash involvement in alopecia areata (AA), often coexisting with nail changes as markers of severe disease. Trichoscopy aids diagnosis through features like exclamation hairs and black dots. Current severity scales (e.g., SALT) should integrate extracapillary involvement to better guide treatment. Recognizing these patterns early improves therapeutic strategies, addressing both physical and psychosocial burdens of AA.
References
- King BA, Mesinkovska NA, Craiglow B, et al. Development of the alopecia areata scale for clinical use: Results of an academic-industry collaborative effort. J Am Acad Dermatol, 2022; 86(2): 359-364. doi: 10.1016/j.jaad.2021.08.043
- Wyrwich KW, Kitchen H, Knight S, et al. Development of Clinician-Reported Outcome (ClinRO) and Patient-Reported Outcome (PRO) Measures for Eyebrow, Eyelash and Nail Assessment in Alopecia Areata. Am J Clin Dermatol, 2020; 21(5): 725-732. doi:10.1007/s40257-020-00545-9.
- Tkachenko E, Huang KP, Ko JM, et al. Brigham Eyebrow Tool for Alopecia: A Reliable Assessment of Eyebrow Alopecia Areata. J Investig Dermatol Symp Proc, 2020; 20(1): S41-S44. doi: 10.1016/j.jisp.2020.06.001.
- Edson-Heredia E, Aranishi T, Isaka Y, Anderson P, Marwaha S, Piercy J. Patient and physician perspectives on alopecia areata: A real-world assessment of severity and burden in Japan. J Dermatol, 2022; 49(6): 575-583. doi:10.1111/1346-8138.16360.
- Andersen YMF, Nymand L, DeLozier AM, Burge R, Edson-Heredia E, Egeberg A. Patient characteristics and disease burden of alopecia areata in the Danish Skin Cohort. BMJ Open, 2022; 12(2): e053137. doi:10.1136/bmjopen-2021-053137.
- Nguyen B, Hu JK, Tosti A. Eyebrow and Eyelash Alopecia: A Clinical Review. Am J Clin Dermatol, 2023; 24(1): 55-67. doi:10.1007/s40257-022-00729-5.
- Chelidze K, Lipner SR. Nail changes in alopecia areata: an update and review. Int J Dermatol, 2018; 57(7): 776-783. doi:10.1111/ijd.13866.

