Gynecomastia Surgery: A 15-Year Experience at Rabat’s Children’s Hospital
Hamza Bensaghir*, Chaimae Ben Driss and Nawfel Fejjal
Plastic surgery unity, Department surgery C, Children’s hospital of Rabat, Morocco
Faculty of medicine and pharmacy of Rabat, University Mohammed V Rabat, Morocco
Received Date: 06/12/2024; Published Date: 10/01/2025
*Corresponding author: Hamza Bensaghir, Plastic surgery unity, Department surgery C, Children’s hospital of Rabat, Morocco; Faculty of medicine and pharmacy of Rabat, University Mohammed V Rabat, Morocco
Abstract
Introduction: Gynecomastia is an abnormal hypertrophy of the mammary glandular tissue in men, it is the most frequent male breast pathology, it has important psychological repercussions in patients. The objective of our work is to study the diagnostic and therapeutic aspects of gynecomastia, comparing the different surgical techniques in the light of the literature.
Patients and Methods: We report the results of a descriptive and retrospective study of 15 Moroccan patients with gynecomastia, treated in the pediatric plastic surgery department of the Children's Hospital of the CHU Avicenne in Rabat over a period of 15 years.
Results: The average age of our patients was 20.93 years. The most represented age group was [13-20] with a rate of 66.67%. A family history of gynecomastia was found in 13.33% of cases, 13% were overweight and 20% were obese. 73.33% of patients consulted after more than one year of evolution. Gynecomastia was bilateral in 86.67% of cases, unilateral in 13.3%. Simon's stage II accounted for 57.1% of the breasts operated on. A subcutaneous mastectomy alone by inferior hemiareolar incision was applied in 3 patients (20%), liposuction alone in 2 patients (13%), and a combination of both techniques in 8 patients (53.3%), the "Round-Block" technique was used in 2 patients (13%). The total complication rate was 20%, 100% were satisfied with the aesthetic results.
Conclusion: The diagnosis of gynecomastia is mainly clinical; a thorough check-up is not always necessary. The combination of subcutaneous mastectomy and liposuction offers the best aesthetic results.
Introduction
Gynecomastia is the most common breast pathology in men, it occurs at any age with frequency peaks in the puberty and adult period, it can be uni or bilateral and is clinically manifested by a flexible retro-areolar mass, mobile and of different sizes depending on the development time of the pathology. Imaging and histology make it possible to distinguish three distinct forms: florid, dendritic and fibrous gynecomastia [1].
Gynecomastia can be physiological in certain periods of life or be pathological or secondary when a hormonal imbalance between androgens and testosterone exists, the latter can be brought about by drug intake, endocrinopathy or other systemic, tumoral or metabolic pathologies.
Medical treatment of this condition is often unable to mediate total regression of gynecomastia, especially when gynecomastia reaches the fibrotic stage. It is here that the role of Plastic surgery is illustrated, which by several types of approaches, makes it possible to treat the hypertrophy of the gland and bring a satisfactory aesthetic result for the patients and in an instantaneous way [2].
The aim of our work is to study the clinical, paraclinical and therapeutic aspect in our patients and to develop the diagnosis of gynecomastia and the surgical management by conducting a preliminary comparative study of the different surgical techniques in the light of the literature.
Materials and Methods
Study Population
This is a descriptive retrospective study of a series of 15 patients treated for gynecomastia who received surgical treatment, collected in the pediatric plastic surgery department of the children's hospital of the CHU Avicenne in covers a period of 15 years from February 2005 to November 2020. This study was conducted with institutional review board approval. No consent was required.
Were included in this study, patients referred by the endocrinology department after a complete clinical and paraclinical assessment for aesthetic management of gynecomastia. Any patient with a hormonal pathology or a syndromic picture not explored by the endocrinology department or a suspicious neoplasia was excluded from the study
Statistical Analysis
Patient data was collected using a pre-established data sheet. We used patient files and operating reports to complete our operating sheets, which enabled us to obtain the results that we will reveal in the next chapter.
These data include: Epidemiological, clinical, paraclinical, therapeutic, evolution and complication data. The computer analysis of the data of our files was carried out by the Excel software. With simple variables: means and percentages
Results
Our study involved a total of 15 patients with gynecomastia, the age of our patients varied between 13 and 57 years with an average of 20.93 years. The most affected age group is 13-20 years old with a percentage of 66.67%. In our series, 8 patients, i.e., 53.33% of cases, had a personal history
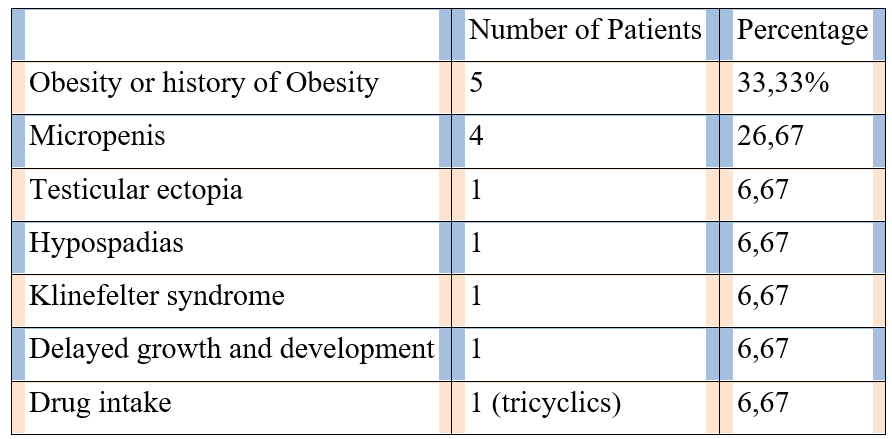
Table 1: Distribution of patients according to history favoring gynecomastia.
Aesthetic discomfort was the main reason for consultation in all our patients, but there wasn’t a clear psychological impact.
The inspection objectified in 86.67% (N=13) a bilateral gynecomastia, symmetrical in 84.62% (N=11) of them (Figure 1) and asymmetrical in 15.38% (N=2) (Figure 2), 13.3% (N=2) presented a left unilateral gynecomastia (Figure 3). In our study, we opted for the Simon classification (Figure 4) in order to stage the gynecomastia of 28 breasts, grade II represented the majority of cases with 57.1% of operated breasts, distributed as follows: 32.1% grade IIA and 25% guard IIB. Grade III accounted for 32.1% of operated breasts and only 10.7% were classified as Simon's grade I.
Our patients benefited from a complete hormonal assessment in the endocrinology department, liver, kidney and thyroid function tests, as well as hormonal tests (E2, total and free testosterone, A, LH, FSH, PRL, hCG, DHEA-SO4 or 17 ketosteroids, SHBG and αFP) were negative.
Ultrasound and mammography assessment was carried out systematically in all patients preoperatively. In Mammography: Cancer was excluded and has differentiated gynecomastia from a mass that requires a biopsy, it was coupled with Ultrasound that assessed the Diagnostic of Idiopathic gynecomastia.
Therapeutic Data
All operations were performed in the supine position, arms outstretched.
All our patients (100%) benefited from short general anesthesia with orotracheal intubation.
In our study, we used the following surgical procedures: - Subcutaneous mastectomy alone via the lower hemi-areolar approach was used in 3 of our patients (Figure 5), which corresponds to 20% of cases. 16 - Aspirative liposuction alone was used in 2 of our patients, which corresponds to 13.33% of cases. The approach used was an incision applied to the lateral part of the thorax at the level of the anterior axillary line. - The combination of subcutaneous mastectomy alone via the lower hemi-areolar route and suction liposuction was used in 8 of our patients, which corresponds to 53.33% of cases (Figure 6). - The “round-block” skin reduction technique was used in 2 of our patients (Figure 7), which corresponds to 13.33% of cases.
All the surgical pieces were sent for anatomo-pathological examination.
Post-operatively, we applied adhesive silicone blades at the level of the scars.
We encountered a total rate of complications of 20% (3/15 patients) distributed as follows: A case of unilateral hematoma observed in a patient who underwent a subcutaneous mastectomy by the lower hemi-areolar approach associated with liposuction - A case of serous effusion observed in a patient who underwent liposuction alone and which resolved after an aspiration puncture - A case of nipple retraction in the right breast was observed in a patient who underwent liposuction Subcutaneous mastectomy via the lower hemi-areolar approach combined with liposuction.

Figure 1: Bilateral symmetrical Gynecomastia.

Figure 2: Bilateral asymmetrical Gynecomastia.

Figure 3: Unilateral Gynecomastia.
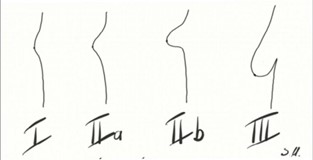
Figure 4: Schematic representation of the different stages of gynecomastia according to the Simons classification.

Figure 5: One of our Patient who presented with stage 1 bilateral gynecomastia which benefited from a subcutaneous mastectomy via the lower hemiareolar procedure.
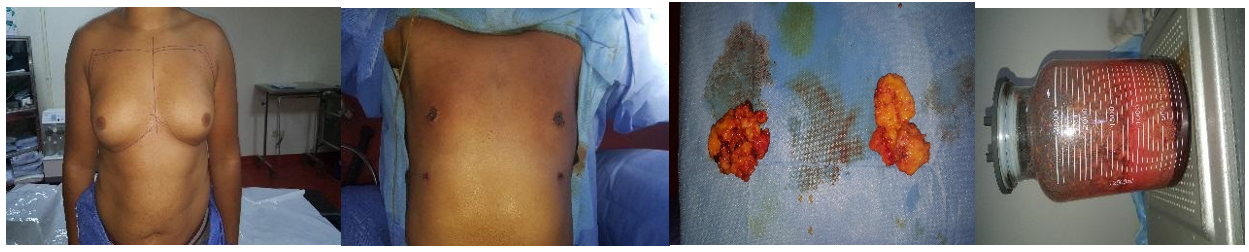
Figure 6: Combination of subcutaneous mastectomy alone via the lower hemi-areolar route and suction liposuction.

Figure 7: The “round-block” skin reduction technique.
Discussion
Gynecomastia is defined by an increase in the volume of the mammary gland in men. It corresponds to unilateral or bilateral hyperplasia. Usually idiopathic; it can in some cases be related to a hormonal imbalance.
Gynecomastia must be distinguished essentially from two other situations: adipomastia, or pseudogynecomastia
When gynecomastia occurs during puberty, it is in most cases idiopathic
The prevalence of gynecomastia was reported to be between 32-65%, due to use of different methods of assessment and the analysis of males of different ages and with different lifestyles, while autopsy data suggest a prevalence of 40% [1,7].
The major cause of gynecomastia is thought to be an altered imbalance between estrogen and androgen effects due to absolute increase in estrogen production, relative decrease in androgen production or a combination of both [1,7,8,9,10,11,12].
Differentiating true gynecomastia from pseudogynecomastia and tumors is based on physical examination. The patient lies on his back with his hands behind his head and the physician places her/his thumb and forefinger on each side of the breast and slowly brings them together. In true cases of gynecomastia, the physician will feel a disc or firm tissue that is concentric with the nipple-areolar complex. In patients with pseudogynecomastia the fingers will not meet any resistance until they reach the nipple [13].
Several classification systems have been proposed over the years each time offering different classification criteria such as breast size, excess skin, histological nature, presence of ptosis and more [3].
Among the most widely used classification systems is the classification of Barros, Rohrich and Simon.
In our study we used the Simon classification which is as follows (Figure 4) [4]:
- Grade I: Slight increase in breast volume without excess skin.
- Grade IIa: Moderate increase in breast volume without excess skin.
- Grade IIb: Moderate increase in breast volume with excess skin.
- Grade III: Severe increase in breast volume with excess skin and furrow
Infra-mammary
The need for an endocrine investigation of gynecomastia will depend on the age of the subject and the results of the history and physical examination [2].
Long-lasting gynecomastia rarely regresses spontaneously and often progresses to very dense fibrosis, so drug treatments are less likely to be effective. Which brings us to surgery, which is the treatment of choice in this type of case, but also when medical treatment is not effective [2].
The grade, the size of the areola and the amount of excess skin are determining factors in the choice of the surgical approach; Several Surgical Techniques: - Open subcutaneous mastectomies - Circumareolar Incision - Periareolar incisions including Webster's lower hemiareolar incision, enlarged lower hemiareolar incision and zigzag hemiareolar incision - Upper hemiareolar incision - L lateral hemiareolar incision – Transareolar incision – Circumthelial incision – Subcutaneous endoscopic mastectomy – Liposuction assisted by aspiration or ultrasound – Liposuction assisted by radiofrequency – Liposuction associated with subcutaneous mastectomy [5].
In our department, our course of action is also determined by the size of the glans, the areola and the skin.If the skin is of good quality, we proceed to liposuction alone or associated with the subcutaneous mastectomy via the lower hemiareolar procedure. If the skin is of poor quality, we perform both liposuctions, the subcutaneous mastectomy and round block.
Wearing compression garments in the postoperative period is a necessity.
Conclusion
Several surgical treatment techniques are possible for the management of GM, and innovation in this area is still relevant. We have concluded from our study and from the literature that the most effective approach is the combination of liposuction and subcutaneous mastectomy via the lower hemiareolar route, given that in the majority of patients we find the association of the two glandular and fatty components. The discretion of the scars, the optimal aesthetic results and the relatively low complication rate are the three strong points of this association [5].
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Neslihan Cuhaci, Sefika Burcak Polat, Berna Evranos, Reyhan Ersoy, Bekir Cakir. Gynecomastia: Clinical evaluation and management.
- Ronald S Swerdloff, Jason CM Ng. Gynecomastia: Etiology, Diagnosis, and Treatment.
- Ruth E Johnson and Hassan Murad M. Gynecomastia: Pathophysiology, Evaluation, and Management.
- Mett TR, Pfeiler PP, Luketina R, Bingöl AS, Krezdorn N, Vogt PM. Surgical treatment of gynaecomastia: a standard of care in plastic surgery. Eur J Plast Surg, 2020; 43(4): 389.
- Arindam Sarkar, Jayanta Bain, Debtanu Bhattacharya, Raghavendra Sawarappa, Kinkar Munian, Gouranga Dutta, et al. Role of Combined Circumareolar Skin Excision and Liposuction in Management of Highgrade Gynaecomastia.
- Dae Hwa Kim, Il Hwan Byun, Won Jai Lee, Dong Kyun Rah, Ji Ye Kim, Dong Won Lee. Surgical Management of Gynecomastia: Subcutaneous Mastectomy and Liposuction.
- Rahmani S, Turton P, Shaaban A, Dall B. Owerview of gynecomastia in the modern era and the Leeds Gynaecomastia Investigation algorithm. Breast J, 2011; 17: 246–255.
- Carlson HE. Approach to the patient with gynecomastia. J Clin Endocrinol Metab, 2011; 96: 15–21.
- Daniels IR, Layer GT. Gynaecomastia. Eur J Surg, 2001; 167: 885–892.
- Johnson RE, Murad MH. Gynecomastia: pathophysiology, evaluation, and management. Mayo Clin Proc, 2009; 84: 1010–1015.
- Bhasin S. Testicular Disorders. In: Kronenberg HM, Melmed S, Polonsky KS, Larsen PR, editors. Williams Textbook of Endocrinology. 11th ed. Philadelphia: Saunders Elsevier, 2008; pp. 669–674.
- Bembo SA, Carlson HE. Gynecomastia: Its features, and when and how to treat it. Cleve Clin J Med, 2004; 71: 511–517.
- Barros AC, Sampaio Mde C. Gynecomastia: Physiopathology, evaluation and treatment. Sao Paulo Med J, 2012; 130: 187–197.

