Trichoscopy Findings of Frontal Fibrosing Alopecia on the Eyebrows
Fajri Zineb, Hanane Baybay, Meryem Soughi, Zakia Douhi, Sara Elloudi and Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II of Fez, Morocco
Received Date: 04/08/2024; Published Date: 25/10/2024
*Corresponding author: Fajri zineb, Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Abstract
Background: Frontal fibrosing alopecia (FFA) is a scarring alopecia with lymphocytic immunomodulated immune-mediated scarring alopecia characterized by progressing perifollicular inflammation and receding of the hair frontotemporal hairline 1. It is frequently preceded by lateral eyebrow loss.
Objective: The aim was to describe and characterize dermoscopic features of eyebrow Frontal fibrosing alopecia.
Methods: We performed a descriptive retro-prospective observational study that included all patients diagnosed with DM in dermatology department over 2 years from 2019 to 2021.
Results: The mean age of our patients was 47 years. Most commons trichoscopic features were Hair regrowth in different directions 82%, peripilar erythema 15%, dystrophic hair 71%, perifollicular pigmentation 15%, red dots 13%, white areas 11%, annular granular appearance 6%, Follicular plugs 66%, Fluffy hair 55%, Pili Torti 2%.
Conclusion: Recognition of dermoscopic features of eybrow FFA is very important and could help in early diagnosis.
Keywords: FFA; Trichoscopy; Eyebrow; Alopecia
Introduction
Frontal fibrosing alopecia (FFA) is a scarring alopecia with lymphocytic immunomodulated immune-mediated scarring alopecia characterized by progressing perifollicular inflammation and receding of the hair frontotemporal hairline 1 .It is frequently preceded by lateral eyebrow loss (39%), 2 The loss of eyebrows has a negative effect on quality of life Various conditions ranging from local dermatological disorders to systemic diseases including scarring and non-scarring alopecia trichoscopy appeared as a rapid and non-invasive tool to complete the physical examination in capillary disorders like AFF, rare series reports trichoscopic signs of eyebrow loss in this pathology.
Our objective is to describe the different trichoscopic characteristics of eyebrow loss in FFA, in order to establish an early diagnosis and start treatment of a pathology that can cause scarring alopecia.
Materials and Methods
The objective of our study is to describe the clinical and trichoscopic characteristics of eyebrow loss in AFF in our population. This is a retro-prospective study, conducted in 45 patients of the hair consultation for a period of 3 years. The included patients had fibrosing frontal alopecia, clinically suspected and histologically confirmed, associated with eyebrow loss. We analyzed dermoscopic images of 45 patients with a diagnosis of FFA, Patients were examined in our outpatient departments. All included patients were women with eyebrow and scalp hair loss. Patients with a history of eyebrow hair removal within the last month or with eyebrow tattooing/ microblading were excluded. All patients had clinical and dermoscopic images obtained with the portable DermLite IV connected to an iPhone. Although the instruments are different, they have comparable image resolution, and both provide high quality images.
Results
The mean age of our patients was 47 years. All patients were female and 66% were menopausal. The duration of the disease varied from 1 to 4 years.
According to clinical history, eyebrow loss preceded scalp hair loss frontal hair loss in 37 patients (82%). Severity of eyebrow loss was estimated to exceed 90% in 8 patients progressing for more than 3 years, 20 patients had loss eyebrow between 50% and 90% and 17 patients had localised loss at the tails of the eyebrows.
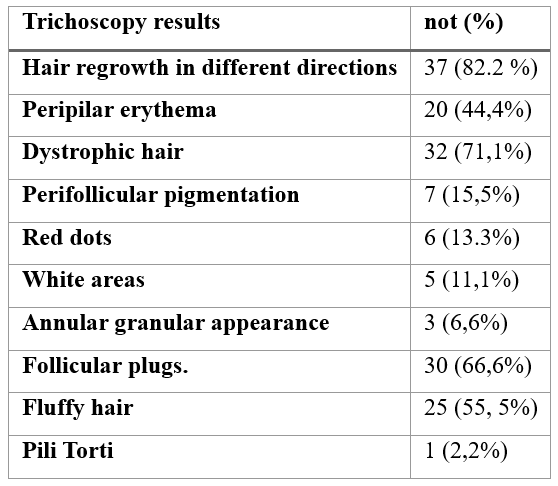
Trichoscopy images were taken at different sites on both eyebrows and the trichoscopic signs, which have been objectified (Table 1, Figure 1). Hair regrowth in different directions 82.2%, peripilar erythema 44,4%, dystrophic hair 44,4%, perifollicular pigmentation 15.5, red dots 13.3, white areas (11,1%), annular granular appearance (6.6%), Follicular plugs 66.6, Fluffy hair 55.5 % pilis tortis 2.2%.

Figure 1: Trichoscopy of the eyebrow.
Table 1: Trichoscopic findings of eyebrow loss in patients with frontal fibrosing alopecia.
Discussion
Vascular malformations are congenital dysmorphic vessels that are present at birth but may not become clinically apparent until later in life. They may worsen in severity with age and persist if untreated [1]. The updated International Society for the Study of Vascular Anomalies classification divides vascular malformations into four types: simple, combined, major named vessel(s), and associated with other anomalies [2]. Vascular malformations can also be subdivided accordingay be responsible for both venous and lymphatic malformations. These vascular malformations are congenital and are due to sporadic somatic mutations in 2 genes. To date, 60% of venous malformations have an activating mutation in the TEK (TIE2) gene, which encodes the TIE2 receptor tyrosine kinase on endothelial cells, and 20% of venous malformations have a mutation in the PIK3CA gene, which results in excessive activation of phosphoinositol 3-kinase (PI3K). These two mutations induce excessive activation of intracellular signaling cascades and in particular the PI3K/AKT/mammalian target of rapamycin (mTOR) pathway), leading to uncontrolled endothelial cell proliferation and disruption of pericyte coverage. These mutations lead to hyperactivation of the PI3K pathway, resulting in abnormal tissue growth, including epithelial and mesenchymal cells. The resulting proliferative syndromes often include slow-flow vascular malformations: lymphatic and venous and vascular malformations, which explains the efficacy of treatment with specific therapies, in particular sirolimus [5].
Figure 2: (A)The clinical manifestation multiple Bluish distension along the vvenous line. (B) Echodoppler image: lagune veineuse compressible.
Conclusion
Congenital vascular malformations are a heterogeneous group of lesions likely to cause significant morbidity in patients. They remain a constant diagnostic challenge, based on a radio-clinical comparison in which the dermatologist plays a very important role, guiding the radiologist based on distinctive clinical criteria to choose the right examination and look for distinctive radiological criteria. Echo-Doppler is the first-line examination for confirming certain clinical criteria.
IRM is the examination of choice, enabling visualization of the entire malformation. Their management requires a multidisciplinary approach dermatologist, pediatricians, radiologists, geneticists, surgeons.
References
- Colletti G, Ierardi AM. Understanding venous malformations of the head and neck: A comprehensive insight. Med Oncol, 2017. http://dx.doi.org/10.1007/s12032-017-0896-3.
- Gemmete JJ, Pandey AS, Kasten SJ, et al. Endovascular methods for the treatment of vascular anomalies. Neuroimaging Clin N Am, 2013; 23: 703-728.
- Seront E, Vikkula M, Boon LM. Venous malformations of the head and neck. Otolaryngol Clin North Am, 2018; 51: 173-184.
- Neil M Kalwani, Stanley G Rockson.Management of lymphatic vascular malformations: A systematic review of the literature. Journal of Vascular Surgery: Venous and Lymphatic Disorders, 2021; 9(4): 1077-1082. doi: 10.1016/j.jvsv.2021.01.013
- Sirolimus Harbers VEM, Rongen GAPJM, van der Vleuten CJM, Ver- hoeven BH, de Laat PCJ, van der Horst CMAM, et al. Patients with Congenital Low- Flow Vascular Malformation Treated with Low Dose Sirolimus. Adv Ther, 2021; 38(6): 3465–3482. https://doi.org/10.1007/ s12325-021-01758-y.

