Navigating the Gastric Erosion as Long-Term Complications of Laparoscopic Adjustable Gastric Banding: A Case Study
Donovan Desir1,2, Muresuk Mena2, Joey Jackson2, Martin D Tanhaei2,3,4,* and Frederick Tiesenga5
1Biomedical Science, Elms College, Chicopee, MA, USA
2School of Medicine, St. George's University, True Blue, GRD
3Biomedical Engineering, University of California, Irvine, CA, USA
4Biomedical Engineering, Johns Hopkins University, Baltimore, MD, USA
5Community First Medical Center, Chicago, IL, USA
Received Date: 18/08/2024; Published Date: 24/10/2024
*Corresponding author: Martin D Tanhaei, School of Medicine, St. George's University, True Blue, GRD; Biomedical Engineering, University of California, Irvine, CA, USA; Biomedical Engineering, Johns Hopkins University, Baltimore, MD, USA
Abstract
Obesity represents a critical public health crisis in the United States, with over 42.4% of adults affected. As obesity-related health complications continue to rise, bariatric surgery offers a viable treatment pathway, particularly Laparoscopic Adjustable Gastric Banding (LAGB), known for its minimal invasiveness and low complication rates. Despite its benefits, LAGB can result in rare but serious complications, such as gastric band erosion, which occurs in less than 2% of cases. This paper delves into a comprehensive examination of the obesity epidemic, with a specific focus on the role of LAGB. Through the lens of a detailed case study of a 57-year-old female experiencing complications a decade post-LAGB, we explore the diagnostic and management challenges presented by gastric band erosion. The patient's extensive medical history and the multidisciplinary approach to her treatment underscore the complexity of postoperative care and the necessity for early detection, continuous patient education, and comprehensive management strategies. This case contributes to the broader understanding of LAGB's potential complications and highlights the importance of holistic care in achieving optimal outcomes for patients undergoing bariatric surgery. Our findings emphasize the critical need for vigilance in the postoperative period and suggest a framework for future research into improving patient outcomes post-LAGB.
Categories: General Surgery; Internal Medicine
Keywords: Obesity; Bariatric Surgery; Laparoscopic Adjustable Gastric Banding; LAGB; Gastric Band Erosion; Postoperative Complications; Multidisciplinary Care; Patient Education; Early Detection
Background
In the United States, obesity has reached epidemic proportions, affecting over 42.4% of adults, a situation highlighted by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) [1]. This pervasive health issue not only strains healthcare systems but also significantly impacts the quality of life of individuals, contributing to an increased risk of serious health complications, such as cardiovascular diseases, diabetes mellitus, osteoarthritis, and specific cancers. The complexity of obesity, marked by its multifaceted causes and consequences, calls for a multifaceted approach to management and treatment.
Bariatric surgery stands out as a cornerstone in the treatment of morbid obesity and its associated comorbidities, offering not just weight loss but also substantial improvements in obesity-related conditions for individuals with a BMI exceeding 30 kg/m^2 and significant comorbidities, or those with a BMI over 40 kg/m2. Among the surgical options, Laparoscopic Adjustable Gastric Banding (LAGB) has distinguished itself due to its less invasive nature, adjustability, and the unique benefit of reversibility. It boasts the lowest rates of perioperative and postoperative complications, alongside significantly low mortality rates [2]. However, despite its advantages, LAGB carries the risk of complications, such as gastric band erosion, which occurs in less than 2% of cases but presents significant management challenges [3].
This paper presents an in-depth examination of the obesity epidemic and explores the critical role of LAGB within this context [4]. By focusing on a detailed case study of a 57-year-old female who encountered complications a decade after undergoing LAGB, this discussion illuminates the intricate process of diagnosing and managing such complications. Her extensive medical and surgical history offers a poignant insight into the complexity of postoperative care, especially in managing rare complications like gastric band erosion. This case underlines the importance of early detection, continuous patient education, and a multidisciplinary care approach to optimize patient outcomes, thereby contributing valuable insights into the literature on LAGB and highlighting the ongoing challenges in combating obesity.
Case Report
A 57-year-old female with a complex medical history, including hypertension, generalized arthritis, past bilateral shoulder surgery, knee arthroscopy, and orthopedic repairs following a motor vehicle accident, presented with symptoms indicative of potential gastric complications from a LAGB placed 10 years prior. Notably, she also had a tracheostomy post-motor-vehicle-accident in 2006, adding to her surgical history's complexity. Upon presentation, she reported bilateral upper abdominal pain, nausea, and vomiting, prompting immediate concern for LAGB-related issues, specifically LAGB complication.
Given her symptoms and past medical and surgical history, the clinical team proceeded with a diagnostic evaluation, including an X-ray of the chest during the emergency room visit before surgical intervention (Figure 1). This preoperative diagnostic step was crucial for assessing the LAGB's condition and planning the appropriate surgical approach. The negative X-ray result and sign of active peritonitis results guided the surgical team's decision-making process, leading to a diagnostic laparoscopy. During the laparoscopy, the team identified and confirmed the erosion of the LAGB into the stomach, necessitating the careful removal of the eroded band. Figure 2 demonstrates an extracted eroded LABG post-operatively. Adhesiolysis and suture repair of the eroded areas were meticulously performed, underscoring the surgery's delicate and precise nature. Additionally, a Jackson-Pratt (JP) drain was strategically placed to monitor any postoperative leakage, further illustrating the careful consideration given to potential complications.
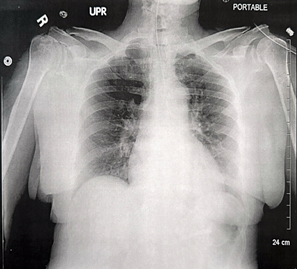
Figure 1: Portable Anteroposterior Chest Radiograph Findings.
The X-ray demonstrates the nasogastric tube positioned below the diaphragm without any signs of acute abnormalities. It reveals no acute pulmonary conditions such as consolidation, pneumothorax, pleural effusion, or air beneath the diaphragm. Additionally, the heart size is within normal ranges, the trachea is centrally located, and the pulmonary vasculature appears normal, showing no evidence of focal airspace consolidation, pneumothorax, or pleural effusion.

Figure 2: Postoperative View of Eroded Adjustable Gastric Band.
The presence of blood suggests that the adjustable gastric band has eroded into the stomach.
The postoperative care plan was comprehensive, addressing pain management, infection prophylaxis, and the patient's chronic conditions. Pain was managed effectively with hydromorphone 0.3 mg IV. Prophylactic measures also included enoxaparin sodium 40 mg subcutaneously for DVT prevention. Attention to her hypertension was maintained by adjusting her medication regimen to include amlodipine 5 mg orally, alongside her ongoing metoprolol treatment. After the surgery, she was placed on a nil per os (NPO) status. On postoperative day 5, she underwent an evaluation for potential leakage, as detailed in Figure 3. The Upper Gastrointestinal (GI) series revealed no signs of leakage, indicating a successful surgical outcome. Consequently, we proceeded with the removal of the nasogastric tube. The postoperative care strategy focused on addressing immediate recovery concerns, including pain management and the prevention of potential infections. Additionally, it underscored the importance of promoting mobility, enhancing lung function via incentive spirometry, and providing nutritional support. Initially, this involved the introduction of clear liquids, gradually progressing to soft foods as tolerated.

Figure 3: Upper GI Series (A-C) Demonstrating Absence of Leakage on Postoperative Day 5.
The Upper GI series, tracing the contrast flow from images A through C, was performed and confirmed the absence of any leakage. This finding indicates that the patient is prepared to initiate a clear liquid diet and allows for the removal of the nasogastric tube.
Discussion
Post-LAGB stomach erosion, while uncommon, is a serious complication that necessitates vigilant monitoring, prompt recognition of early symptoms, and timely intervention to optimize outcomes. Despite its rarity, LAGB is favored for its minimally invasive nature and comparatively low mortality rates. Erosion associated with gastric bands can emerge either early or late post-operation, with this particular case falling into the latter category due to its occurrence over a decade after the procedure. Typically, early erosion is linked to factors like adhesion, whereas late erosions have been attributed to undiagnosed perforations or initial infections. This patient's symptoms initially suggested a possible Adjustable Gastric Band slippage—a condition more commonly associated with late erosions. However, the concurrent presence of adhesion raised the possibility of early erosion characteristics, underscoring the diagnostic and management challenges associated with LAGB complications [5].
Ensuring the Adjustable Gastric Band is securely placed is essential to prevent slippage and to guarantee free rotation around the superior stomach, highlighting the importance of meticulous surgical techniques during band placement [6-8]. The timing and nature of this patient's symptoms, alongside surgical findings of adhesion, present an atypical instance of late erosion displaying features generally associated with early erosion cases. Such nuances emphasize the intricacy of categorizing and addressing erosion incidents following LAGB, necessitating a comprehensive approach in patient management [8,9].
This case emphasizes the critical role of early detection and management of post-LAGB complications, facilitated by patient education on symptom awareness and the importance of follow-up consultations. Successful management and recovery in this patient's scenario were achieved through a multidisciplinary approach, focusing on pain management, nutritional support, and prevention of common postoperative complications such as atelectasis and DVT [10]. The multidisciplinary care extended beyond surgery, addressing comorbidities and ensuring ongoing support for the patient's long-term health and well-being. This case illustrates the necessity of thorough preoperative assessments and the value of a detailed discharge plan that includes dietary guidelines and monitoring for potential complications, underscoring the holistic approach required for optimal outcomes in complex bariatric cases.
Conclusion
The obesity epidemic in the United States underscores the need for effective and multifaceted treatment approaches, including bariatric surgery options like Laparoscopic Adjustable Gastric Banding (LAGB). Despite its proven efficacy in weight loss and low complication rates, LAGB is not without risks, as highlighted by the case study of a 57-year-old female experiencing gastric band erosion a decade post-operation. This case exemplifies the complexities inherent in managing long-term complications of bariatric surgery, emphasizing the importance of early detection, patient education, and a multidisciplinary approach to care.
The successful management of this patient's complications underscores the necessity of vigilance and comprehensive care in the postoperative period. It highlights the importance of ongoing monitoring for potential complications, even years after the surgery, and the need for patients to remain informed about their health. Furthermore, it demonstrates the value of a multidisciplinary team in addressing the multifactorial aspects of recovery, ensuring that both the physical and psychological needs of the patient are met.
In conclusion, while LAGB remains a valuable tool in the fight against obesity, its potential complications require careful consideration. The healthcare community must prioritize research into optimizing surgical outcomes and developing robust postoperative care protocols. By fostering an environment of continuous patient education and interdisciplinary collaboration, we can improve the long-term success of bariatric surgery and enhance the quality of life for individuals living with obesity. This case study contributes valuable insights into the complexities of post-LAGB care and serves as a reminder of the ongoing challenges in managing the obesity epidemic.
Author Contributions: All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Concept and design: Martin D Tanhaei, Muresuk Mena Frederick Tiesenga
Acquisition, analysis, or interpretation of data: Donovan Desir, Muresuk Mena, Martin D Tanhaei
Drafting of the manuscript: Donovan Desir, Martin D Tanhaei, Muresuk Mena, Joey Jackson, Fredrick Tiesenga
Critical review of the manuscript for important intellectual content: Martin D Tanhaei, Muresuk Mena, Frederick Tiesenga
Supervision: Donovan Desir, Frederick Tiesenga, Martin D. Tanhaei
Disclosures
Disclosures Human subjects: Consent was obtained or waived by all participants in this study. Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following: Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work. Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work. Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Acknowledgements: Special thanks to the dedicated work of general surgeons, Frederick M Tiesenga, MD, Juaquito M Jorge, MD (on-call surgeon), and Deepa Patel, MD (on-call surgeon), whose expertise was fundamental in this case.
References
- Overweight & Obesity Statistics. National Institute of Diabetes and Digestive and Kidney Diseases, U.S. Department of Health and Human Services, 2021.
- Furbetta N, Cervelli R, Furbetta F. Laparoscopic adjustable gastric banding, the past, the present and the future. Ann Transl Med, 2020; 8(Suppl 1): S4. doi: 10.21037/atm.2019.09.17.
- Yun GY, Kim WS, Kim HJ, Kang SH, Moon HS, Sung JK, et al. Asymptomatic gastric band erosion detected during routine gastroduodenoscopy. Clin Endosc, 2016; 49(3): 294-297. doi: 10.5946/ce.2016.001.
- Seeras K, Acho RJ, Prakash S. Laparoscopic gastric band placement. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023.
- Tabibian N, Swehli E, Boyd A, Umbreen A, Tabibian JH. Abdominal adhesions: A practical review of an often-overlooked entity. Ann Med Surg (Lond), 2017; 15: 9-13. doi: 10.1016/j.amsu.2017.01.021.
- Herndon LK, Stead TG, Ganti L, Jasper T, Lebowitz D. Laparoscopic adjustable gastric band slippage presenting as chest pain. Cureus, 2019; 11(7): e5069. doi: 10.7759/cureus.5069.
- Ma IT, Madura JA. Gastrointestinal complications after bariatric surgery. Gastroenterol Hepatol (N Y), 2015; 11(8): 526-535.
- Management of long-term complications of gastric banding and gastric balloon. Bariatric Times, 2024.
- Furbetta N, Gragnani F, Cervelli R, et al. Technical details and result of a minimally invasive management of gastric band erosions: a series of 47 patients. Obes Surg, 2019; 29: 3754–3761. doi: 10.1007/s11695-019-04170-2.
- Prevention and management of complications after bariatric surgery. BC Med J, 2021; 63(3): 170-178.

