Cervico-Facial Odontogenic Cellulitis in People with Diabetes: About 19 Cases
Opango ADC1,*, Bennaoui Y2, Hattab MSK1, Maidam S1, El Bouihi M1 and Mansouri Hattab N1
1Department of Stomatology and Maxillofacial Surgery, CHU Mohammed VI Marrakech, Morocco
2Faculty of Medicine and Pharmacy of Marrakech, Caddi Ayyad University, Morocco
Received Date: 25/06/2024; Published Date: 09/10/2024
*Corresponding author: Alban Déo Christian Opango, Doctor, Department of Stomatology and maxillofacial surgery department, Mohammed VI University Hospital, Marrakech 40000, Morocco
Summary
Head and neck cellulitis is an infection of the fatty tissue of the face and neck. These are serious conditions. They generally occur in specific pathologies, notably diabetes. This work aims to objectify the clinical, bacteriological and therapeutic particularities of cervico-facial cellulitis in diabetic situations.
We conducted a descriptive and prospective study over 12 months that included 19 diabetic patients suffering from odontogenic cervico-facial cellulitis treated in the maxillofacial surgery department of the Mohammed VI University Hospital. The study parameters were epidemiological, clinical, paraclinical, therapeutic and evolutionary.
We noted a sex ratio = 1.4 with an average age of 41 years. The patients all presented with chronic glycemic imbalance and were followed irregularly with poor compliance with antidiabetic treatment. The clinical signs were dominated by jugal swelling. Paraclinically, an inflammatory syndrome was noted and bacteriology noted a polymicrobial origin. Therapeutic PEC combines medical treatment (for cellulite and diabetes), drainage of collections and treatment of the tooth in question. The evolution was favorable in the majority of cases.
Head and neck cellulitis is a serious condition, especially when it occurs in debilitated areas such as diabetes. Although diabetes is an area favoring the occurrence of CCF, they can be the cause of a profound acute glycemic imbalance (ketacidosis). Their management must be early and multidisciplinary in order to avoid the occurrence of serious complications.
Keywords: Cervico-facial cellulitis; Odontogenic; Diabetes; Treatment
Introduction
Head and neck cellulitis (CCF) is a serious infection of the soft tissues of the face and neck. Their etiologies are numerous, dominated by dental origin (odontogenic cellulitis). They sometimes occur in fragile situations such as diabetes or they are particularly serious. The aim of this work is to show the clinical, bacteriological and therapeutic particularities of head and neck cellulitis in diabetic pathologies in our context.
Material and Methods
This is a descriptive and prospective study, carried out between January and December 2022 within the stomatology and maxillofacial surgery department of the Mohammed VI University Hospital in Marrakech. We included 19 patients treated for odontogenic cervico-facial cellulitis in a diabetic context. The study parameters were epidemiological, clinical, paraclinical, therapeutic and evolutionary.
Results
The population studied was 19 patients including 11 men (57.9%) and 8 women (42.1%), i.e. a sex ratio of 1.4. The average age of our patients was 41.3 years.
All our patients were diabetic. 12 patients (63.2%) were type 2 diabetics and 8 patients (36.8%) were type 1 diabetics. A notion of self-medication with non-steroidal anti-inflammatory drugs was noted in 26.3% of cases. . The patients were all followed irregularly with poor compliance with antidiabetic treatment. The last medical check-up with the endocrinologist was more than a year ago in 63.1% of cases. The mean glycated hemoglobin (HbA1C) at the time of hospitalization was 12.3. The average consultation duration was 4.3 days.
All patients presented with inflammatory swelling on admission (Figure 1, 2). Trismus was noted in 9 patients (47.4%), dysphagia in 5 patients (26.3%), polypnea in 2 patients (10.5%).
Biologically, there was an inflammatory syndrome with a mean leukocytosis of 12778 WBC/mm3 and a mean CRP of 79.1 mg/l. The average blood glucose on admission was 2.54 g/l.
All patients had a head and neck scan which revealed soft tissue infiltration with or without sampling. Cellulite was serous in 68.4% of cases, collected in 31.6% of cases. We noted no cases of gangrenous cellulitis. Cellulite was localized: submandibular (47.4%), upper jugal (31.6%), submental (10.5%) and masseterine (10.5%).
A cytobacteriological examination was carried out on a sample of cellulite pus collected (6 cases). It made it possible to isolate Staphylococcus aureus in one case. In 4 cases, the sample was polymicrobial. In one case, no germs were found.
The entry point was dental, all patients underwent an orthopantomogram (Figure 3, 4). These were dental caries in 73.7%, advanced periodontitis in 21.1% and post-dental extraction cellulitis in 1 case (5.2%).
All patients were treated in hospital. The treatment consisted of 3 parts. Systematic medical treatment combining rehydration protocol and insulin therapy in close collaboration with the metabolic diseases and endocrinology department, systematic dual therapy combining amoxicillin, clavulanic acid (80 mg/kg/day) and metronidazole (50 mg/kg/day) in 84 .2% of cases, and ceftriaxone (100mg/kg/day) and metronidazole in 15.8% of cases. The 2nd part was the surgical treatment of the collected cellulite. This involved emptying the collection with installation of a Delbet blade and twice-daily washing. Drainage was performed intraorally in 4 cases and transcutaneously in 2 cases, under local anesthesia in 83.3% and under general anesthesia in 16.7% of cases. The 3rd part was the treatment of the portal of entry, the extraction of the causal tooth was carried out in 73.7% of cases, an alveolar revision for a residual apical granuloma in 5.2% and oral care for periodontitis in 21.1% of cases.
The evolution has been favorable for all our patients. There was a clinical improvement, a normalization of the glycemic figures, a negative assessment of the infection, and above all no transfer to intensive care was noted. The average length of hospitalization was 10.9 days.

Figure 1, 2: Patient with cellulite in the lower right part of the cheek (front view); Patient with cellulitis in the lower right part of the cheek (lateral view).
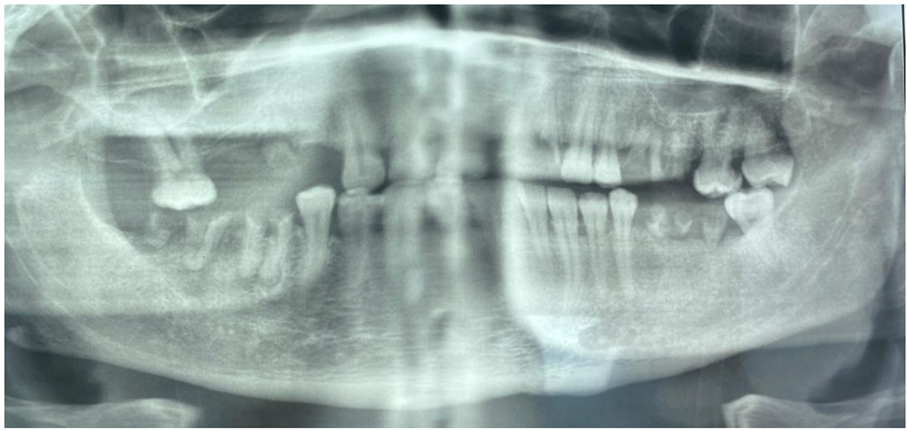
Figure 3: Orthopantomogram of the patient revealing numerous dental roots with apical granulomas.

Figure 4: Good clinical progress of the patient.
Discussion
Head and neck cellulitis is a serious pathology and constitutes a public health problem [1,2]. Many contributing factors have been described in the literature, including fragile diseases such as diabetes [3,4]. Indeed, diabetes due to its chronic glycemic imbalance (average HbA1C = 12.3 in our series) is responsible for immunosuppression. This is explained by an alteration in the phagocytic functions of leukocytes [5]. Other contributing factors are also described in the literature: retroviral infection, malnutrition, alcohol, tobacco, heart, spleen or kidney transplant sites [6-8]. A male predominance and a mean age of around 40 years were found in our series, which is consistent with certain series [9,10].
The prevalence of dental origin of cervico-facial cellulitis in diabetics is estimated between 66 and 88% in the literature [6,8,9,11]. In our series this represented 100% of cases, this is explained by the fact that we are a stomatology and maxillofacial surgery department, therefore with a bias in the admission of patients.
The germs responsible for odontogenic cervico-facial cellulitis in diabetics are variable, but dominated by saprophytic germs from the oral cavity, notably anaerobic germs [12,13].
Although head and neck cellulitis in diabetic patients is recognized as serious [14], we observed no cases of transfer to intensive care or death in our series. This could be explained by the rapid consultation of patients (4.3 days on average), rapid and multidisciplinary care, and the selection of patients on admission, with serious cases being directly admitted to intensive care. The literature reports a mortality rate of between 20 and 40% [15].
Prevention remains the real solution to this serious pathology. This requires good education of diabetic patients in terms of oral hygiene, diagnosis and early management of caries and periodontal pathologies in diabetic patients. For this, good collaboration between diabetologists, dental surgeons and maxillofacial surgeons is a prerequisite.
Conclusion
Cellulite of the head and neck is particularly serious in diabetics. Indeed, diabetes promotes the occurrence of these CCFs, but they can seriously decompensate the diabetes, endangering the vital prognosis. Early and multidisciplinary treatment is the only guarantee of a good result. Prevention remains the best weapon.
References
- Miloundja J, Assini Eyogho SF, Mandiji Lawson JM, Ondounda M, Koumba JS. Diffuse cervico-facial cellulitis: 32 cases observed in Libreville. Health. July-September, 2011; 21(3): 153-157.
- Dubernard C, Bellanger S, Chambon G, Léon H, Torres JH, Lozza J. cellulitis of dental origin with a life-threatening prognosis: about a case. Oral and oral surgery, 2009; 15: 119-125.
- Flanagan CE, Daramola OO, Maisel RH, et al. Surgical debridement and adjunctive hyperbaric oxygen in cervical necrotizing fasciitis. Otolaryngol Head and Neck Surgery, 2009; 140: 730-734.
- Leyva P, Herrero M, Eslava JM, Acero J. Cervical necrotizing fasciitis and diabetic ketoacidosis: literature review and case report. Int J Oral Maxillofac Surg, 2013; 42: 1592-1595.
- Oh Dédjan NE, Haraj S, El Aziz A. Chadli. Cellulitis of the head and neck in diabetics. Metabolic Disease Medicine, 2016; 10(4).
- El Ayoubi A, El Ayoubi F, Mas E, et al. Diffuse cervico-facial cellulitis of dental origin: approximately 60 cases. Med Buccale Chir Buccale, 2009; 15: 127-135.
- Rouadi S, Ouassi L, El Khiati R, et al. Cervico-facial cellulitis in 130 cases. Pan Afr Med J, 2013; 14: 88.
- Rakotoarison RA, Ramarozatovo NP, Rakoto FA, Rakotovao FJ. Head and neck cellulitis: about 41 cases. Med Buccale Chir Buccale, 2008; 14: 35-39.
- Bahu SJ, Shibuya TY, Meleca RJ, et al. Craniocervical necrotizing fasciitis: an 11-year experience. Otolaryngol Head and Neck Surgery, 2001; 125: 245-252.
- Mohammedi I, Ceruse P, Duperret S, et al Cervical necrotizing fasciitis: 10 years of experience in a single institution. Intensive Care Med 1999; 25:829-34.
- Kpemissi E. Cervico-facial cellulitis of oral and dental origin. Study of 26 cases at Lomé University Hospital. Rev Laryngol Oto-Rhinol, 1995; 116: 195-197.
- Pignat JC, Haguenauer JP, Navailles B. Spontaneous to anaerobic diffuse cervical cellulitis. Rev Laryngol, 1989; 110: 141-144.
- Ennouri A, Bouzouita N, Hajri H, et al. Cervico-facial cellulitis in 20 cases. Medical Tunisia, 1991; 69: 459-462.
- Wong TY. A national survey of deaths due to oral and maxillofacial infections: the Taiwanese experience. J Oral Maxillofac Surg, 1999; 57(11): 1297-1299.
- Romain Schmidt P, Hannion X, et al. Gangrenous cervico-facial cellulitis of dental origin: about 11 cases. Rev Stomatol Chir Maxillo-Fac, 1989; 6: 428-437.

