Efficacy of Aripiprazole for the Management of Antipsychotic-Induced Hyperprolactinemia: A Retrospective Case Series
Fareena Soomro, Divya Periasamy*, Oleg Isakov, Andres Aguilar-Henriquez and Sahar Abzakh
Department of Psychiatry, Brookdale University Hospital and Medical Center, USA
Received Date: 29/05/2024; Published Date: 02/10/2024
*Corresponding author: Divya Periasamy, Department of Psychiatry, Brookdale University Hospital and Medical Center, USA
Abstract
Introduction: In psychiatry hyperprolactinemia is an adverse reaction that occurs due to antipsychotics and some antidepressants. Clinicians are tasked with the challenge of managing hyperprolactinemia, as patients might decompensate if the offending agent is discontinued or modified. Alternate treatment approaches were needed to ensure the hyperprolactinemia is resolved without psychiatric decompensation of the patient.
Objective: To assess the effectiveness of aripiprazole in the management of hyperprolactinemia induced by antipsychotic medications.
Methods: A retrospective chart review done at a mental health outpatient clinic. Charts from Dec 2021 to Aug 2023 were reviewed. A group of patients who developed hyperprolactinemia while they were being treated with an antipsychotic were identified. 10 patients out of the group were symptomatic and noted to have coinciding high prolactin levels. These patients were either switched to Aripiprazole, a partial D2 agonist or it was added to their treatment regimen.
Results: Switching to or adding aripiprazole to their treatment plan has been observed to lead to a significant decrease in their serum prolactin levels, coupled with noticeable amelioration of their symptoms.
Conclusion: In conclusion, this retrospective case series highlights the efficacy of aripiprazole in the management of antipsychotic-induced hyperprolactinemia. This study, conducted over two years, showed that adding aripiprazole or swapping aripiprazole with antipsychotic treatment led to a significant reduction in serum prolactin levels in all 10 patients. These findings underscore the potential of aripiprazole as an effective therapeutic option for addressing hyperprolactinemia associated with antipsychotic medication, offering clinicians a valuable tool to mitigate this common side effect. Further research may be warranted to establish more precise dosing guidelines of aripiprazole in this context. Nonetheless, the results presented here contribute to the evidence supporting aripiprazole for the management of antipsychotic-induced hyperprolactinemia.
Introduction
Hyperprolactinemia is a common and often underestimated side effect of antipsychotic drugs (APDs). Prolactin is released from lactotroph cells and is regulated by the hypothalamic-pituitary system. In psychiatry hyperprolactinemia is an adverse reaction that occurs due to antipsychotics and some antidepressants. 48%-98% perimenopausal women and 42-47% of men report symptoms related to hyperprolactinemia secondary to antipsychotic use [1].
Multiple factors like stress, sex, and food could alter prolactin levels, but some medications also contribute to altering prolactin levels. Normal prolactin levels in males < 20 ng/ml and in women it is <25 ng/ml. Antipsychotics are the most common drugs that increase prolactin levels. This elevation of prolactin occurs from the blockade of dopamine-2 (D2) receptors, particularly in the tuberoinfundibular tract [2]
Hyperprolactinemia usually presents with acute symptoms like changes in libido, acne, hirsutism, amenorrhea, galactorrhea and gynecomastia [3,4]. Long term complications were classified into 7 categories according to a study - breast/lactation disorder, female genital system disorders, hair and skin abnormalities, infertility, menstrual cycle disorders, sexual dysfunction, and other clinical presentation. Based on their analysis it was concluded that breast/lactation disorder, sexual dysfunction and menstrual cycle disorders were the most reported [3,5].
Patients presenting with above mentioned symptoms are usually subjected to blood work and tests to conclude, drug induced hyperprolactinemia. Blood levels for prolactin levels are drawn. Pregnancy, hypothyroidism, PCOS are ruled out. Liver and kidney dysfunctions are ruled out. MRI of the brain could be done to rule out sellar/parasellar tumors [6].
First line treatment for hyperprolactinemia is usually dopamine agonists like cabergoline, bromocriptine, quinagolide or discontinuing the offending medication. However, dopamine agonists have adverse reactions like nausea, vomiting, postural hypotension, digital Raynaud type syndrome, leg cramps, flushing and nasal congestion [6]. Discontinuing or lowering doses of medications poses the risk of psychotic relapse. To prevent this aripiprazole, a partial dopamine agonist with a strong affinity for D2 receptors, is presented as a novel approach. It has the potential to displace high-potency antipsychotics, especially long-acting injectables, providing relief from hyperprolactinemia without worsening psychosis [7-9].
This study is a retrospective case series highlighting the efficacy of aripiprazole in managing hyperprolactinemia induced by other antipsychotics.
Materials and Methods
A retrospective case series was conducted on 10 patients receiving mental health outpatient treatment from December 2021 to August 2023. The study focused on mental health patients diagnosed with schizophrenia, schizoaffective disorder, delusional disorder, and bipolar disorder according to DSM 5, utilizing both First- Generation Antipsychotics (FGA) and Second-Generation Antipsychotics (SGA).
The Inclusion criteria was, patients with symptoms of hyperprolactinemia like amenorrhea, galactorrhea, gynecomastia and sexual disturbances. elevated prolactin levels within the range of 16.8 to 245. Patients who were treated with aripiprazole for hyperprolactinemia The Exclusion criteria was patients who did not undergo follow-up blood work after initiating aripiprazole to monitor prolactin levels and patients with prolactin levels exceeding 300 and on whom imaging studies could not be conducted to rule out pituitary causes. A literature review was performed using Pubmed, google scholar and uptodate, 25 articles were reviewed. Out of the 25, articles that depicted hyperprolactinemia due to medical conditions were eliminated and remaining 16 articles were included in this study.
Results
Cases
Patient 1: A 65-year-old male with a diagnosis of schizophrenia, treated with long-acting injections of Haldol decanoate for more than 10 years. He developed gynecomastia 2 years back. The prolactin level was measured and was 18.1. To address the issue, aripiprazole was introduced at a dose of 5 mg. 3 months later the prolactin level was repeated, and it had dropped to 8.1, which was within the normal range. This also halted the progression of gynecomastia.
Patient 2: A 31-year-old female was diagnosed with bipolar disorder and was treated with long-acting injection Invega Sustenna (Paliperidone Palmitate) 156 mg IM for a year. She developed amenorrhea. Pregnancy was ruled out and prolactin levels were obtained which was 245. Paliperidone was discontinued and aripiprazole 5 mg was initiated and was titrated up to 10 mg. The patient was also followed by endocrinology and prolactin levels were drawn monthly. It reduced from 245 to 103 to 77.4 and after 5 months it normalized to 11. Menstrual irregularities resolved and the patient continued aripiprazole 10 mg QD.
Patient 3: A 47-year-old female diagnosed with schizoaffective disorder; bipolar type was on Haldol decanoate 200 mg long-acting injection for several years. She developed galactorrhea and upon workup was found to have a prolactin level of 65.3.
Aripiprazole was introduced at 10 mg and was then titrated to 20 mg. This effectively lowered prolactin levels to 5.9, leading to the alleviation of galactorrhea. Patient continues to receive Haldol decanoate 200 mg IM 4 weeks once along with aripiprazole 20 mg once daily.
Patient 4: A 32-year-old female diagnosed with schizoaffective disorder, undergoing treatment with paliperidone 234 mg IM 4 weeks once for 4 years had reported amenorrhea. Prolactin levels were checked which was 94. Aripiprazole 5 mg PO QD was added to her treatment regimen, following which prolactin levels decreased to 11 and the amenorrhea resolved. The patient was continued on Paliperidone long-acting injection 234 mg IM as well as aripiprazole 5 mg oral medication.
Patient 5: A 22-year-old female with delusional disorder was on Risperdal 3 mg oral medication once daily for a year. She developed amenorrhea and was referred to her psychiatrist for medication management. Upon lab work, prolactin levels were 197. Aripiprazole of 5 mg oral once a day was initiated and Risperdal was decreased to 1.5 mg at bedtime for 2 weeks. The Risperdal was then discontinued, and the aripiprazole was increased to 10 mg. Prolactin levels were repeated 2 months later and the level had dropped to 17.9. 7 months later it was 10.7.
Patient 6: A 26-year-old male was diagnosed with schizoaffective disorder and was referred from another clinic on Paliperidone oral meds 6 mg once a day. Since the patient continued hearing voices the paliperidone was increased to 9 mg once a day.
During routine lab work prolactin was noted to 19 and the patient did admit to history of gynecomastia without galactorrhea. Repeat Prolactin levels after 2 months showed further rise in levels 57.3. Aripiprazole was added at a low dose of 2 mg once a day as the patient had previously developed itching and akathisia on aripiprazole oral as well as long-acting injection. Prolactin levels after 8 months of treatment dropped down to 11.3.
Patient 7: A 44-year-old female diagnosed with schizoaffective disorder, was treated with quetiapine 200 mg at bedtime and was also receiving Paliperidone 156 mg IM long-acting injections 4 weeks once. 2 months into treatment, the patient reported amenorrhea and hair loss to her OBGYN and a workup was done. Prolactin levels showed 125, following which her psychiatrist added aripiprazole 5 mg once a day to her treatment regimen and titrated it to aripiprazole 10 mg once a day. 3 months later prolactin was repeated, and it had dropped to 31.6 and her amenorrhea had resolved. At the patient’s request paliperidone injection was discontinued and she was stabilized on oral aripiprazole 10 mg once a day only.
Patient 8: A 32-year-old female with a diagnosis of schizoaffective disorder, bipolar type was initiated on Paliperidone 156 mg IM during her inpatient hospitalization. She continued the same when she followed up at the outpatient clinic. 6 months into treatment, the patient reported galactorrhea. Upon work up she was noted to have prolactin levels of 129. Paliperidone was discontinued and aripiprazole 10 mg was initiated. It was titrated to 15 mg and then she was stabilized on aripiprazole’s long-acting injection. Repeat prolactin levels a month later was 84 and after 6 months was 22.1 and the patient was no longer experiencing symptoms of hyperprolactinemia.
Patient 9: A 38-year-old female diagnosed with schizoaffective disorder; Bipolar type was initiated on Paliperidone long-acting injection 156 mg while she was on the inpatient unit. She was treated with the same at the outpatient clinic and after 3 months the patient experienced amenorrhea. Her OBGYN obtained prolactin levels and it was 131. Paliperidone was discontinued and aripiprazole 5 mg was initiated which was titrated to 15 mg. Repeat prolactin levels in a month reduced to 20.3 resolving the amenorrhea.
Patient 10: A 38-year-old female patient with a diagnosis of chronic schizophrenia, was stabilized with a long-acting injection of Paliperidone 234 mg loading dose and given a paliperidone 156 mg IM maintenance dose on the inpatient unit and was discharged to follow up at our clinic. Patient continued to be stable on a maintenance dose of Paliperidone Palmitate 156 mg IM 4 weeks once. After 6-8 months of treatment, she reported amenorrhea for 3 months. Pregnancy was ruled out with blood work, but prolactin levels were as high as 183. She had no other symptoms of hyperprolactinemia, like gynecomastia or galactorrhea or decreased libido. 5 mg of aripiprazole was augmented to her treatment regimen. Within a month her amenorrhea resolved and repeat prolactin levels after a month showed 132. Further trending of prolactin levels was not done after this as the patient became pregnant and preferred to hold all medications.
Table 1: Summary of results.
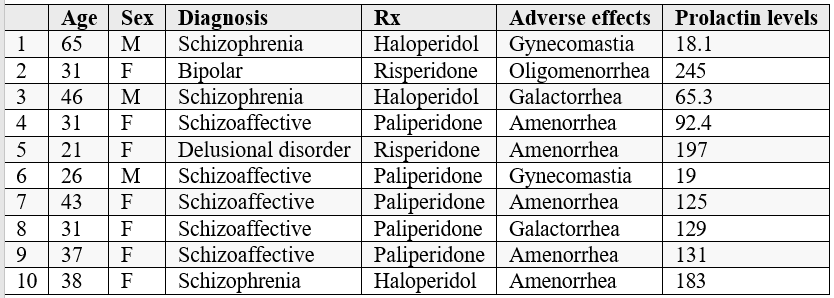
Based on the study it was determined that aripiprazole could be the management of antipsychotic-induced hyperprolactinemia among patients diagnosed with schizophrenia, schizoaffective disorder, delusional disorder, and bipolar disorder. The study, conducted over nearly two years, showed that the addition or augmentation of Aripiprazole in conjunction with antipsychotic treatment led to a significant reduction in serum prolactin levels in all 10 patients.
DIscussion
Multiple medications can cause hyperprolactinemia, the more predominant medications are antipsychotics. Increased potency on the D2 receptors within the hypothalamic tuberoinfundibular tract increased the chances of hyperprolactinemia. Medications like Paliperidone, Risperidone, Haloperidol, Fluphenazine, Pimozide and thioridazine have the highest affinity to the D2 receptors (Table 2, 3) [10-11]. Common symptoms associated with hyperprolactinemia are menstrual disturbances, galactorrhea, and impotence.
Ruling out structural abnormalities is important prior to determining that hyperprolactinemia is drug induced.
Table 2: Second generation antipsychotics with affinity to dopamine receptors on the tuberoinfundibular tract [11].
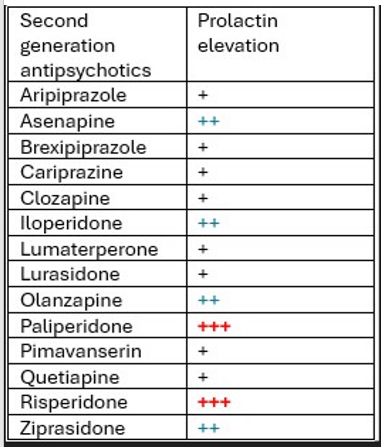
+++ High Affinity ; ++ Moderate Affinity; + Low Affinity
Table 3: First generation antipsychotics with high affinity for dopamine on the tuberoinfundibular tract [11].
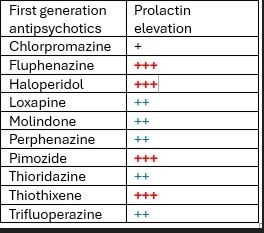
+++ High Affinity ; ++ Moderate Affinity; + Low Affinity
Various options are available to manage antipsychotic-induced hyperprolactinemia, including aripiprazole, cabergoline, bromocriptine, metformin, chamomile, bambusa vulgaris, momordica charanthia, Rauwolfia vomitoria, Ficus sur, Clerodendrum capitatum, Peony-Glycyrrhiza decoction and Shakuyaku-kanzo-to [12]. Cabergoline and bromocriptine caused headache and dizziness, asthenia, rhinitis and needed optimization of dose to achieve adequate results. Metformin caused flatulence, nausea, vomiting and the dose ranged between 750 mg - 3000 mg. Aripiprazole though had some side effects like akathisia, weight gain, fatigue and agitation the dose was small between 2 mg to 10 mg. Herbal alternative were not studied adequately or they had intolerable side effects. Aripiprazole has adequate studies, has minimal side effects and appears to have benefited most of the patients with drug induced hyperprolactinemia [13-17].
There were some limitations to this study. It was a small sample size and was a retrospective study. There was limited data available about the ideal dose of aripiprazole for drug induced hyperprolactinemia. There was also limited data if age and gender impact the prolactin levels. More studies are needed to elaborate on details at this time.
Conclusion
Aripiprazole exhibits potential efficacy in alleviating antipsychotic-induced hyperprolactinemia, with relatively lesser side effects. Hence, aripiprazole provides a viable solution for individuals grappling with heightened prolactin levels arising from antipsychotic treatments. What sets aripiprazole apart is its unique mechanism of action as a partial agonist on dopamine D2 receptors. The dosage choice should be personalized, considering an individual patient’s needs and responses to the medication. Based on our study, a low dose appears to be optimum in resolving hyperprolactinemia. Further research and larger-scale studies may be warranted Nonetheless, the results presented here contribute to the growing body of evidence supporting aripiprazole as a promising intervention for the management of antipsychotic-induced hyperprolactinemia.
References
- Zhao J, Song X, Ai X, et Adjunctive Aripiprazole Treatment for Risperidone-Induced Hyperprolactinemia: An 8-Week Randomized, Open-Label, Comparative Clinical Trial. PLoS One, 2015. 10.1371/journal.pone.0139717.
- Milano Walter, Walter D'Acunto, Cosimo De Rosa, Michele Festa, Michela Milano, et al. Recent Clinical Aspects of Hyperprolactinemia Induced Antipsychotics,Reviews on Recent Clinical Trials, 2011; 6(1): 52-64. 1574: 8871/1876. doi: 2174/157488711793980138
- Mah PM, Webster Hyperprolactinemia: etiology, diagnosis, and management. Semin Reprod Med, 2002; 20: 365-374.
- Bun-Hee Lee, Yong-Ku Kim, Sun-Hwa Using aripiprazole to resolve antipsychotic-induced symptomatic hyperprolactinemia: A pilot study.
- Jolene R Bostwick, Sally K Guthrie, Vicki L Antipsychotic-Induced Hyperprolactinemia.
- Junqueira DR, Bennett D, Huh SY, Casañas I, Comabella C. Clinical Presentations of Drug-Induced Hyperprolactinaemia: A Literature Pharmaceut Med, 2023; 37: 153-166.
- Samperi I, Lithgow K, Karavitaki Hyperprolactinaemia. J Clin Med, 2019; 13: 2203.
- Kazuo Mihara, Goyo Nagai, Akifumi Nakamura, Yasuhide Fukuji, Takeshi Suzuki, Tsuyoshi Kondo. Improvement in antipsychotic-induced hyperprolactinemia with the addition of aripiprazole in schizophrenic patients. Clinical Neuropsychopharmacology and Therapeutics, 2010; 1: 1-5. doi: 5234/cnpt.1.1.
- Paraskevi Kotorki, Parthena Pelka, Christina Leotsakou, Aikaterini Kalogeropoulou, Markella Fiste, Georgios Vagionis, et al. Reversal of symptomatic antipsychotic-induced hyperprolactinemia with addition of Annals of General Psychiatry, 2010; 9(Suppl 1): S164.
- Byerly Matthew, Suppes Trisha, Tran Quynh-Van, Baker Ross A. Clinical Implications of Antipsychotic-Induced
- Hyperprolactinemia in Patients with Schizophrenia Spectrum or Bipolar Spectrum Disorders Recent Developments and Current Perspectives. Journal of Clinical Psyhcopharmacology, 2007; 27(6): 639-661.
- https://www.uptodate.com/contents/search?search=antipsychotic%20induced%20hyperprolactinemia&sp=4&searchType=GRAPHICS....
- Rusgis MM, Alabbasi AY, Nelson Guidance on the treatment of antipsychotic- induced hyperprolactinemia when switching the antipsychotic is not an option. Am J Health Syst Pharm, 2021; 78(10): 862-871.
- Brigitta E Miyamoto, Martha Galecki, Dimitry Guidelines for Antipsychotic-Induced Hyperprolactinemia, Psychiatric Annals, 2015; 45(5): 266–272.
- Baybars Veznedaroglu, Nesrin Dilbaz, Ozcan Uzun, Erdal TARC: Turkish aripiprazole consensus report- Aripiprazole use and switching from other antipsychotics to aripiprazoleconsensus recommendations by a Turkish multidisciplinary panel. TARC: Turkish aripiprazole consensus report- Aripiprazole use and switching from other antipsychotics to aripiprazoleconsensus recommendations by a Turkish multidisciplinary panel, 2018; 8(10): 271-285.
- Mong-Liang Lu, Winston W Shen, Chun-Hsin Chen. Time course of the changes in antipsychotic-induced hyperprolactinemia following the switch to aripiprazole. Prog Neuropsychopharmacol Biol Psychiatry, 2008; 32(8): 1978-1981.
- Meiling Meng, Wei Li, Shaowei Zhang, Hongyan Wang, Jianhua Sheng, Jijun Wang, et al. Using aripiprazole to reduce antipsychotic-induced hyperprolactinemia: meta-analysis of currently available randomized controlled Shanghai Archives of Psychiatry, 2015; 27(1): 4-17.
- Treatment of Antipsychotic-Induced Hyperprolactinemia: An Update on the Role of the Dopaminergic Receptors D2 Partial Agonist Aripiprazole. Recent Patents on Endocrine, Metabolic & Immune Drug Discovery, 2014; 8(1): 30-37.

