Ruptured Giant Abdominal Aortic Aneurysms
Dragan Piljic¹*, Nail Sehic¹, Dilista Piljic¹, Fahrudin Sabanovic², Alen Hajdarevic¹, Ema Tahto¹, Haris Vukas², Hajrudin Kozarevic¹, Bozo Juric¹, Zijah Rifatbegovic¹, Esed Omerkic³ and Jus Ksela⁴
¹University of Tuzla, School of Medicine, University Clinical Center Tuzla, Tuzla, Bosnia and Herzegovina
²University Hospital Center Zenica, Zenica, Bosnia and Herzegovina
³University of Tuzla, School of Medicine, Dom Zdravlja Zivinice, Bosnia and Herzegovina
⁴University of Ljubljana, School of Medicine, University Clinical Center Ljubljana, Ljubljana, Slovenia
Received Date: 25/03/2024; Published Date: 14/08/2024
*Corresponding author: Dragan Piljic, MD, PhD, Department of Cardiovascular Surgery, University Clinical Center Tuzla, I. Pasic bb, Tuzla 75000, Bosnia and Herzegovina
Abstract
Giant abdominal aortic aneurysms (AAAs) are rare clinical entities. Giant aortic aneurysm is defined as aneurysm in the aorta greater than 10 cm in diameter. It is a rare finding since most patients will present with complications of dissection or rupture before the size of aneurysm reaches that magnitude. The risk of AAA rupture is closely associated with the maximum aneurysm diameter. This case series report describes five cases of giant ruptured AAAs presented with rupture. Open repair seems to be the treatment of choice for most giant aneurysms, both ruptured and unruptured.
Keywords: Giant; Aneurysm; Rupture; Open repair
Introduction
The risk of AAA rupture is closely associated with the maximum aneurysm diameter. The annual rupture risk exceeds 14% [1] for aneurysms >6 cm and reaches 30-50% for AAA's exceeding 8 cm in diameter [2]. Undoubtedly, the rupture risk of AAA is subject to considerable individual variability [3]. Apart from larger initial maximum aneurysm diameter, other factors such as female gender, current smoking status, lower forced expiratory volume in 1 second (FEV 1) as well as higher mean blood pressure are independently associated with the risk of AAA rupture [3]. It is extremely rare to encounter very large aneurysms exceeding 10 cm in diameter as it is expected that such large aneurysms would have been either previously ruptured or repaired. Notably, under some uncertain protective circumstances AAA may reach extreme diameters up to 26 cm of maximum transverse diameter [4].
The most important factor in the pathogenesis aortic aneurysms is elastin and collagen degeneration in the media layer. Aneurysm may be associated by collagen degeneration or autoimmune diseases such as Marfan syndrome, Takayasu’s arthritis, giant cell arthritis, temporal arthritis and Behçet’s disease [5].
The most serious complication of AAA is rupture. Mortality rates in aortic rupture reach up to 90% [6]. The risk of rupture is very high in aneurysms greater than 5 cm, aneurysms growing faster than 0.5 cm per year or in painful AAAs [7].
Open repair of giant AAA’s is often the only available treatment, though not always with good results [8].
Case 1
A 76-year-old male with a medical history of smoking and hypertension was admitted to our clinic with a ruptured abdominal aortic aneurysm diagnosed by a trans-abdominal ultrasound. He was immediately brought to the Emergency Room (ER). His blood pressure was 80/40 mm Hg, with an HTC of less than 0.17. Six years earlier, he had noticed a painless, enlarging abdominal mass. An emergency abdominal Computed Tomographic Angiography (CTA) with intravenous contrast showed a giant infrarenal AAA measuring 13x11 cm in diameter, with clear evidence of rupture and a large intra-abdominal hematoma (Figure 1). He was immediately brought to the Operating Theater (OT).
The classic median laparotomy was made. After we had opened the abdomen, we found a huge retroperitoneal hematoma was pushing the intra-abdominal organs almost to the edge of the rectal fascia. His blood pressure suddenly dropped to 45/25 mm Hg for the next several minutes. A continuous infusion of norepinephrine was administered (60 mcg/min), several doses of pure adrenalin (3 mg) and pure norepinephrine (1 mg) after what his blood pressure immediately rose up to the mean pressure of 80 mm Hg. During the surgery he was anuric. Autologous blood transfusion was made with cell saver. Additionally, he received several doses of blood, blood derivates (fresh frozen plasma, cryoprecipitate, platelets), and other intravenous solutions totaling approximately 8 liters. We replaced the ruptured AAA using a 20 mm polytetrafluoroethylene (PTFE) vascular graft. After surgery he was transferred to the intensive care unit (ICU) where the blood pressure rose, and diuresis was established (Figure 2).
On the first postoperative day, he was woken up without neurological deficits. Six days after surgery we performed a control CT angiography that showed normal findings on the abdominal iliac and leg vessels. Recovery was uneventful and he was discharged from hospital on postoperative day 10.
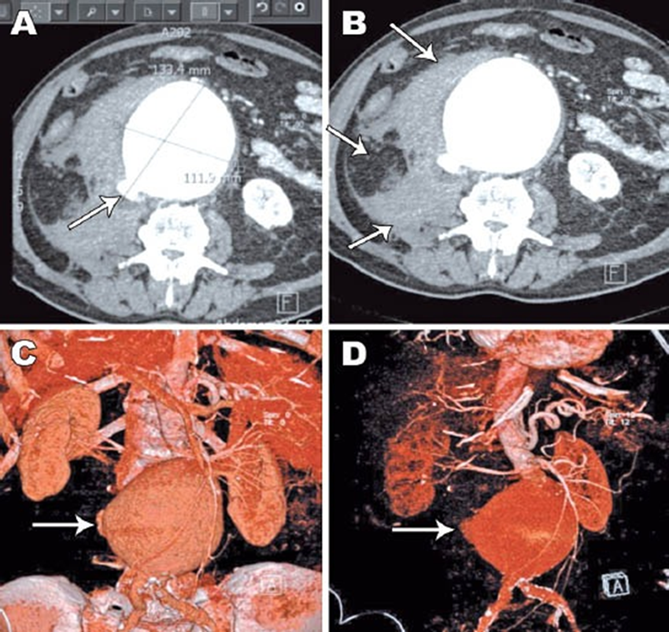
Figure 1: Abdominal computed tomographic angiography with contrast showing: A) a ruptured giant abdominal aortic aneurysm (AAA), measuring 13x11 cm with B) a large intra-abdominal hematoma, that compresses the intra-abdominal organs. C) and D) showing a ruptured giant infrarenal AAA.
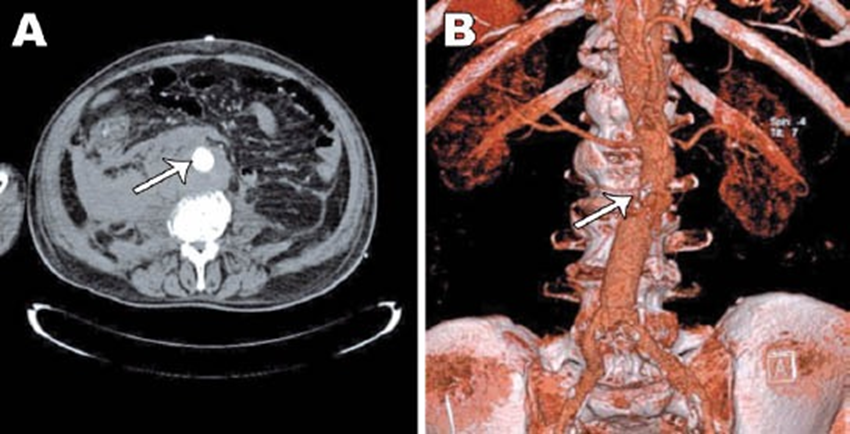
Figure 2: Postoperative Computed Tomographic Angiography (CTA) with contrast showing: A) complete sealing of the aneurysm and no endoleak detected. B) Abdominal CTA with contrast showing patency of the graft.
Case 2
A 78-year-old man with a history of smoking tobacco, hyperlipidemia and hypertension, was admitted to our department with ruptured abdominal aortic aneurysm diagnosed by ultrasonography of the abdomen. The blood pressure was 60/20 mm Hg. An emergent computed tomography scan of the abdomen revealed a rupture of a giant infrarenal AAA of 16 cm in diameter with extensive intraluminal thrombus, evidence of rupture and large intraabdominal hematoma (Figure 1). Abdominal computed tomography angiography with contrast showed a ruptured giant infrarenal AAA measuring 16x11 cm with a large mural thrombus and intra-abdominal hematoma compressing intra-abdominal organs (Figure 3).
The patient underwent a successful open surgical repair with placement of a Dacron tube graft 18 mm. Postoperative CTA with contrast showed complete sealing of the aneurysm with no endoleak detected (Figure 4). The patient was transferred to the intensive care unit following successful surgical repair. Patient was transferred to the department of cardiovascular surgery on postoperative day 2. Postoperative recovery resulted in hospital discharge at postoperative day 12.
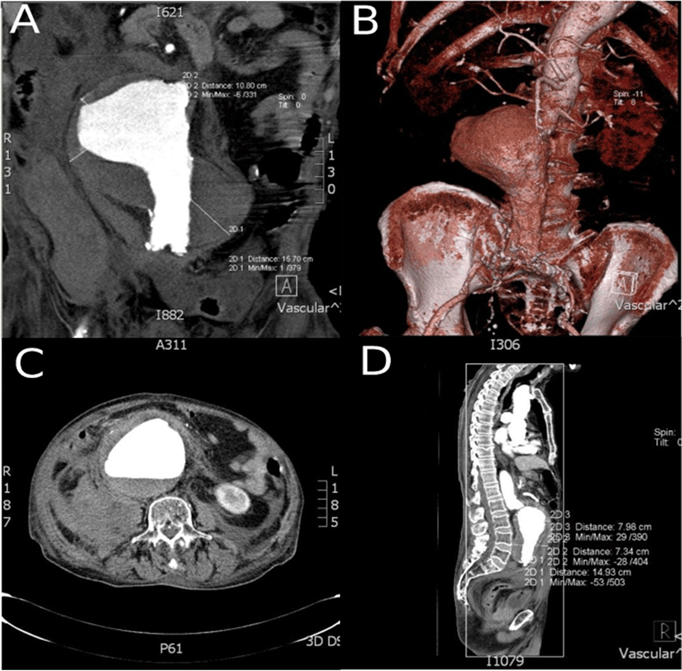
Figure 3: Rupture and large intraabdominal hematoma.
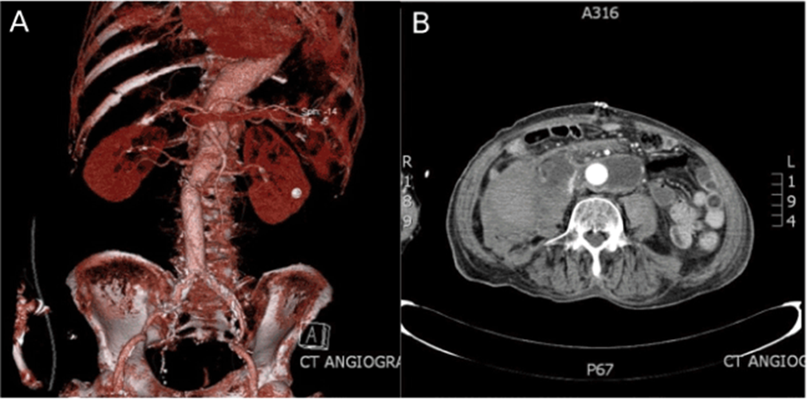
Figure 4: Dacron tube graft.
Case 3
An 84-year-old male with traces of blood in the stool complaining of severe abdominal pain since the night before was transferred to our Clinic as an emergency. His medical history included hypertension and a chronic disorder of the mental processes caused by dementia. Seventeen years earlier, the patient had a stroke. The patient's physical examination revealed a firm pulsatile abdominal mass in the mesogastrium. The patient's vital signs were as follows: blood pressure, 90/51 mm Hg; heart rate, 90 bpm; respiratory rate, 22 breaths per minute; and oxygen saturation on room air, 92%.
Emergency contrast-enhanced computed tomographic angiograms confirmed the diagnosis of a giant ruptured infrarenal AAA, demonstrating a maximum diameter of 13 cm and a large amount of intramural thrombus (Figure 5).
The patient was transferred to the ICU to prepare for surgery.
However, before entering an operating room, the patient's general clinical condition was worsened, followed by cardiorespiratory arrest, so the patient died in the ICU just before surgery. Autopsy findings showed massive bleeding into the colon, which speaks in favour of an additional rupture of the aorta with bleeding into the colon.
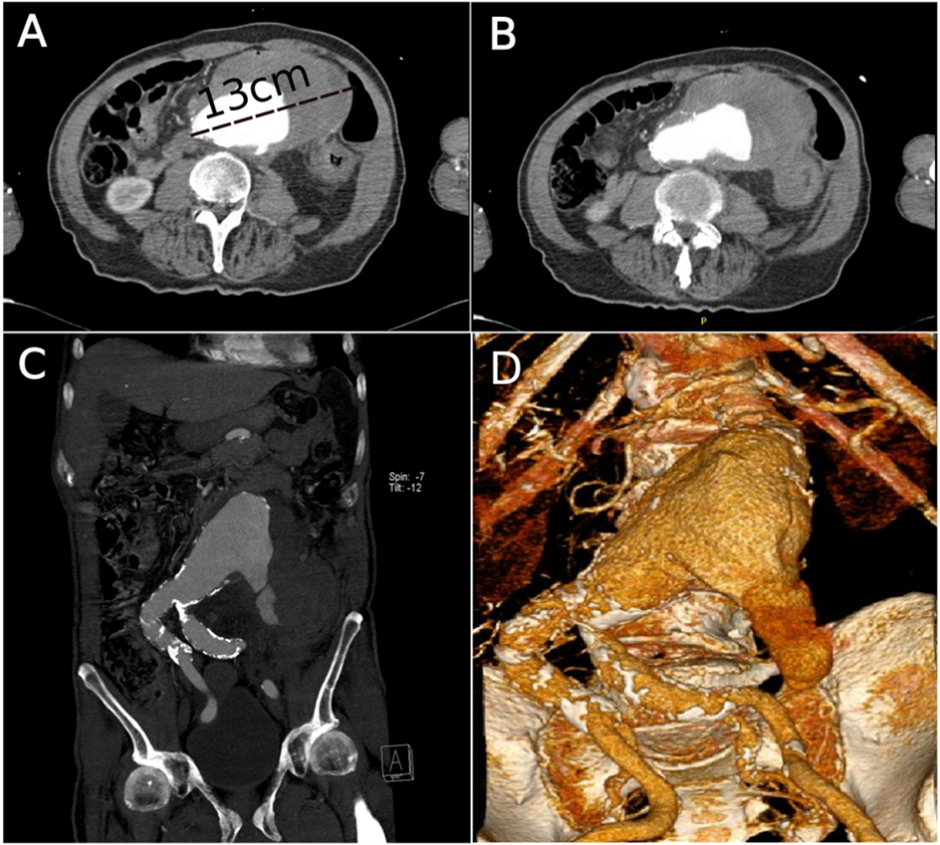
Figure 5: (A) A transverse imaging study demonstrates a maximum diameter of 13 cm and a large amount of intramural thrombus. (B) imaging study demonstrating a large intra-abdominal hematoma that compresses the intra-abdominal organs. C) coronal section CT images of the ruptured abdominal aortic aneurysm, (D) Anterolateral view of computed tomography angiogram with three-dimensional reconstruction with massive bleeding into the colon.
Case 4
The patient was admitted to our hospital because of the abdominal pain. Previously, an abdominal ultrasound where dissection of the abdominal aortic aneurysm was suspected and referred to our Clinic. We had ordered a CT angiography, and the findings verified a retroperitoneal hematoma as part of ruptured abdominal aortic aneurysms; the abdominal aorta was measured with thrombotic masses of 12.6 cm x 9.84 cm with the active lumen of 7.64 cm x 6.84 cm (Figure 6).
Emergency surgery was done because of the hemodynamic instability of the patient (hypovolemic shock), and an approach through the front abdominal wall by median laparotomy was made to the abdominal aorta. After inspecting the aorta, the ruptured site was marked, and a clamp was placed superiorly to the rupture but below renal arteries. After the incision on the aorta, a proximal suture of a Dacron tube graft 22 mm was made so as a distal suture. Moreover, after closing the aortic sac, peritoneum and front abdominal wall, the patient was hemodynamically stable and transferred to the ICU.
The patient was transferred to the cardiovascular surgery department on postoperative day 1. Postoperative recovery resulted in hospital discharge on postoperative day 5.
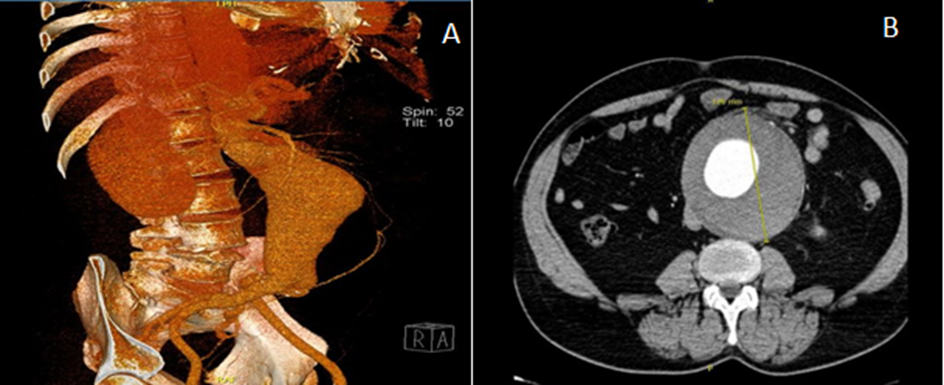
Figure 6: Preoperative computed tomography angiograms demonstrating a ruptured abdominal aortic aneurysm. (A) Lateral view of preoperative CTA with 3D reconstruction. (B) Axial imaging study demonstrates a maximum diameter of 12.6 cm and a large circular intramural thrombus.
Case 5
Few days after surgery. The male patient had dilatated the abdominal aorta for many years at an unknown time of diagnosis. He was on anticoagulant Vitamin K Antagonists therapy for a year because of thrombotic masses in the aorta. Also, suffer from elevated blood pressure with no intake of therapy. For a long time, he had had pain in his back, and the morning before coming to our Clinic, he suffered a strong pain in the back because of what was examined in the ER; an ultrasound verified an aneurysm of the abdominal aorta.
CT angiography was made to confirm the diagnosis and showed infrarenal dilatated abdominal aorta in a maximal wide section of 12.6 cm, with a sign of the ruptured aneurysmatic wall (Figure 7).
Emergency surgery was made, and the operative area was adequately prepared after positioning the patient. A median laparotomy was approached retroperitoneal space and abdominal aorta. A ruptured aorta was dissected and replaced with Dacron vascular graft No 20. Hemostasis was made, and the abdominal wall was closed by layers. The patient has been transferred to the ICU and is hemodynamically stable.
The patient was transferred to the Department of Cardiovascular Surgery on postoperative day 4. The patient recovered well postoperatively and was discharged nine days after operation.
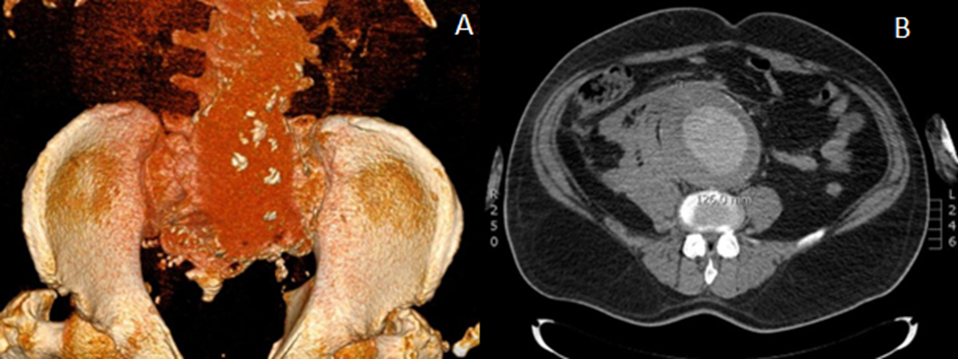
Figure 7: Ruptured abdominal aortic aneurysm. (A). Anteroposterior view of preoperative CTA with three-dimensional reconstruction. (B). CTA demonstrating a 12.6-cm abdominal aortic aneurysm with rupture and large intraabdominal hematoma.
Discussion
Aneurysm size is the most critical factor related to the likelihood of rupture, and the risk increases substantially in large aneurysms. The annual rupture risk for AAAs>8 cm is 30-50% [9]. Symptomatic aneurysms present with back, abdominal, buttock, groin, testicular, or leg pain and require urgent surgical attention. Rupture of an AAA involves complete loss of aortic wall integrity and is a surgical emergency requiring immediate repair [10]. The sheer size of the aneurysm, the short length of the neck, and the dislodgment of abdominal organs that may be densely adhered to its surface with fistula formation make surgery of this entity very challenging. Open repair of giant AAAs is often the only available treatment, though not always with good results [8].
The rupture of AAA is a catastrophic event associated with a high mortality rate. The majority of patients die without getting to the operating room. Even if they reach the operating room alive and undergo surgical repair, only 50% of those survive beyond 30 days [3]. The open surgical repair of the ruptured giant AAA presents a challenge due to numerous significant technical difficulties that complement the huge size of the aneurysm, such as the short length of the neck and the dislodgement of abdominal organs that may be densely adhered to the aneurysm surface sometimes resulting even in fistula formation [8].
The repair of these giant aneurysms presents a challenge during surgery. Ruptured giant AAAs present a significant additional surgical and anesthetic challenge [11].
Conclusion
Despite being associated with numerous technical difficulties and often hampered with bad outcomes, open surgical repair of ruptured giant AAA is sometimes the only available treatment, which, if performed promptly, results in eventful recovery, as in most of our cases.
Authors' contributions:
Concept and design of study: DP('guarantor'), NS, DiP, ZR, EO, JK
Acquisition of data or analysis and interpretation of data: DP, AH, ET, HV, HK, BJ, ZR, JK
Drafting the article or revising it critically for important intellectual content: DP, NS, DiP, FS, JK
Final approval of the version to be published: DP, Ns, DiP, FS, AH, ET, HV, HK, BJ, ZR, EO, JK
Informed consent: The patient provided written informed consent for publication of the figures.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This work received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Brown PM, Zelt DT, Sobolev B. The risk of rupture in untreated aneurysms: the impact of size, gender, and expansion rate. J Vasc Surg, 2003; 37: 280-284.
- Brewster DC, Cronenwett JL, Hallet JW Jr, Johnston KW, Krupski WC, et al. Guidelines for the treatment of abdominal aortic aneurysms. Report of a subcommittee of the Joint Council of the American Association for Vascular Surgery and Society for Vascular Surgery. J Vasc Surg, 2003; 37: 1106-1117.
- Brown LC, Powell JT. Risk factors for aneurysm rupture in patients kept under ultrasound surveillance. UK Small Aneurysm Trial Participants. Ann Surg, 1999; 230: 289-296.
- Rodrigues H, Bastos Gonçalves F, Ferreira ME. Giant aneurysm of the abdominal aorta. J Vasc Surg, 2014; 59: 826-827.
- Svensson LG, Crawford ES. Aortic dissection and aortic aneurysm surgery: clinical observations, experimental investigations and statistical analyses. Part III. Curr Probl Surg, 1993; 30: 1–163.
- Cleveland Clinic.
- Yiğit G, Çetinkaya F, Aytekin B, Türkçü AM, Ozen F, Sarıtaş F. Open surgical repair of a giant abdominal aortic aneurysm. Kardiochir Torakochir Pol, 2019; 16 (3): 144-146. DOI: https://doi.org/10.5114/kitp.2019.88607
- Maras D, Lioupis C, Moulakakis KG, Sfyroeras G, Pavlidis P, Bountouris I, et al. Giant abdominal aortic aneurysms: clinical and technical considerations. Acta Chir Belg, 2009; 109: 376–380.
- Brewster DC, Cronenwett JL, Hallett JW Jr, Johnston KW, Krupski WC, Matsumura JS, et al. Guidelines for the treatment of abdominal aortic aneurysms. Report of a subcommittee of the Joint Council of the American Association for Vascular Surgery and Society for Vascular Surgery. J Vasc Surg, 2003; 37: 1106–1117.
- Upchurch GR, Jr, Schaub TA. Abdominal aortic aneurysm. Am Fam Physician, 2006; 73: 1198–1204.
- Piljic D, Tabakovic M, Kusturica A, Piljic D, Hajdarevic A, Klokocovnik T. Giant ruptured abdominal aortic aneurysm. Saudi Med J, 2014; 35 (10): 1283-1284.

