Subcutaneous Extravasation of Solutions: Moroccan Series
Hamraoui Hafsa*, Baybaye Hanane, Soughi Meryem, Douhi Zakia, Elloudi Sara and Mernissi Fatima Zahra
Department of Dermatology, Hassan II University Hospital Center of Fez, Morocco
Received Date: 27/03/2024; Published Date: 12/08/2024
*Corresponding author: Hamraoui Hafsa, Department of Dermatology - Hassan II University Hospital Center of Fez, Morocco
Abstract
Introduction: Extravasation is described by the Infusion Nurses Society (INS) as the unintentional administration of a vesicant solution or drug into the tissues surrounding the infusion. These perfusion accidents often occur in a peripheral venous line.
Objectives: Describe the epidemiological-clinical profile of patients and evaluate the results of early management of solute extravasations to the upper limb.
Methods: Prospective study at the CHU Hassan II dermatology department level, spanning a period of 6 months, bringing together all patients for whom a dermatological opinion was requested in the face of extravasation of a subcutaneous treatment.
Results: Fourteen patients were collected, the average age was 53 years, all our patients were immunocompromised followed for a neoplasm and under chemotherapy. 11 for extravasation of chemotherapy products at the anterior surface of the forearm, 3 at the dorsal surface of the hand, including one having the extravasation of contrast product and an Aciclovir, and the 3rd the amoxicillin protected. The treatment consisted, according to the established protocol, of infiltration of the area with physiological serum and aspiration-washing at the expense of the subcutaneous tissues carried out on a patient. Mobility of the upper limb was assessed, as well as aesthetic after-effects. A Doppler ultrasound was performed on a patient eliminating venous and arterial thrombosis in her, for the other patients the opinion was requested late, with a duration ranging from one week to 15 days after extravasation, the patients were placed under care premises with good development.
Conclusion: Extravasations of cytotoxic solutes to the upper limb are a medico-surgical emergency. Early treatment helps limit functional and aesthetic after-effects. Prevention remains the best treatment.
Keywords: Extravasation; Solutes; Subcutaneous
Introduction
Extravasation is described by the Infusion Nurses Society (INS) as the involuntary administration of a vesicant solution or drug into the tissues surrounding the infusion [1] and represents 23 to 78% of infusion-related complications. peripheral venous veins, in the absence of treatment these complications can be extremely serious they can lead to constant functional deficiencies, considerably worsening the quality of life of patients [3]. The aim of this study is to describe the epidemiological-clinical profile of patients and evaluate the results of the management of solute extravasations to the upper limb.
Methods
Prospective study at the CHU Hassan II dermatology department level, spanning a period of one year from January 2022 to January 2023, bringing together all patients for whom a dermatological opinion was requested in the face of extravasation of a treatment subcutaneously.
Results
Fourteen patients were collected, the average age is 53 years, all our patients were immunocompromised followed for a neoplasm and under chemotherapy. 11 for extravasation of chemotherapy products at the anterior surface of the forearm, 3 at the dorsal surface of the hand, including one having the extravasation of contrast product and an Aciclovir, and the 3rd the amoxicillin protected. The treatment consisted, according to the established protocol, of infiltration of the area with physiological serum and aspiration-washing at the expense of the subcutaneous tissues carried out on a patient. Mobility of the upper limb was assessed, as well as aesthetic after-effects. A Doppler ultrasound was carried out in a patient eliminating venous and arterial thrombosis in her, for the other patients the opinion was requested late, with a duration ranging from one week to 15 days after extravasation, the patients were placed under care premises with good development.

Figure1: Watch out technique in a patient after contrast medium extravasation.
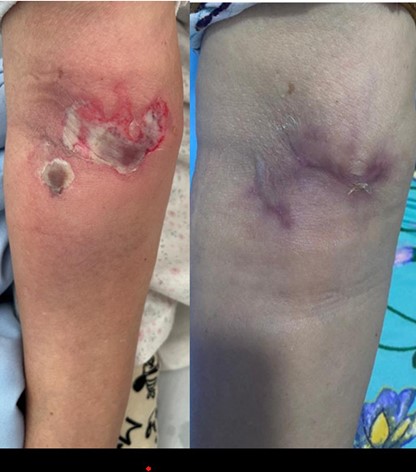
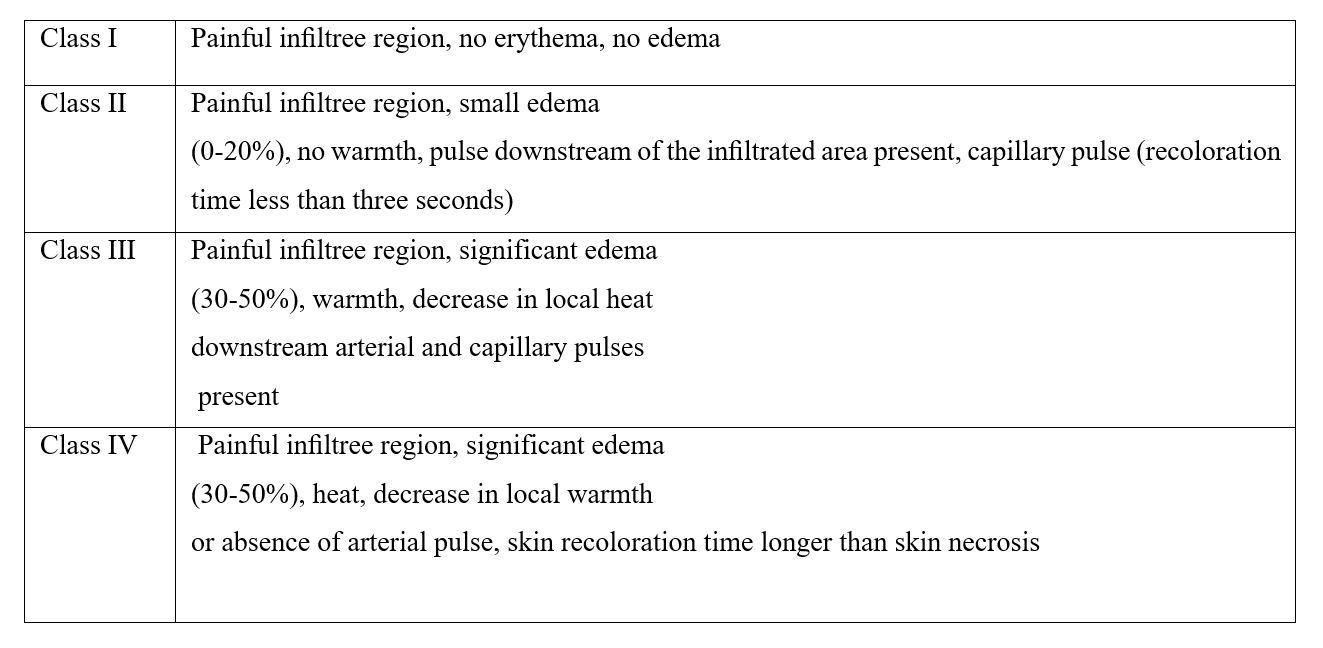
Figure 2: Left: Clinical photo of skin necrosis following extravasation of Acilovir, right: control photo after directed healing.
Table 1: Classification de Millam 1998.
Discussion
Extravasation is the process by which a solution prepared by surgical expertise infiltrates into surrounding tissues intravenously [4]. It can cause excessive tissue necrosis. Its occurrence rate in children ranges from 5 to 58%; according to research, it is reported that approximately 0.4% of cases progress to skin necrosis. An Anglo-Saxon study reports a prevalence of 38 per 1,000, with a necrosis rate of 3.8%.[5]. Good knowledge of risk factors makes it possible to better target the population at risk and prevent these accidents. These risk factors are of 3 types: factors linked to the patient (premature, elderly), local factors (catheter not in place due to lack of fixation or excess mobility), factors linked to the product administered (the nature of the product administered, its osmolarity and its cytotoxicity) [6] in our patients we objectified factors linked to the patients (immunocompromised and elderly patients and factors linked to the product administered (most of our patients presented extravasation of chemotherapy molecules.
Extravasation of the solute into the subcutaneous tissues initially manifests clinically as pain, local erythema followed by edema, the importance of which increases with the volume administered and the nature of the product, then pallor may develop, reflecting a local tissue ischemia. If no treatment is instituted, it can lead to an area of tissue necrosis which will become demarcated in around two weeks in the form of a blackish plaque, Millam in 1998 proposed a classification see table 2 [7] in our series only 2 patients were seen at the stage of erythema and edema the other patients were seen at the stage of necrosis because the dermatological opinion was requested late and the delay in reporting the incident.
the pathophysiological mechanism of this damage would include direct cellular toxicity of the drug, vasoconstriction which leads to ischemic necrosis, osmotic damage, the ischemic effect of extrinsic mechanical compression of large volumes of extravasated solutions, and all factors causing the infections overlapping and skin defects [8].
The management of these incidents still remains controversial. The initial symptomatology in no way presumes the future evolution and is often underestimated by medical personnel, hence the delay in reporting the incident and in providing treatment can be wrongly taken as lymphangitis, the evolution and extension are unpredictable, making diagnostic and therapeutic management sometimes difficult.
The first actions to be carried out urgently in the event of extravasation are [9,1]:
- stop the infusion
- notification of the concentration and quantity of remaining medication.
- documentation in the patient's medical record: date and time, digital photographs, type and size of peripheral access device, technique of chemotherapy administration, symptoms reported by the patient and type of chemotherapy.
-if pain systemic analgesics.
-infiltration of sterile saline solution at the subcutaneous level inside and around the lesion.
-It is then necessary to assess the severity of local clinical signs by referring to the Millam classification. All authors agree on the need for early treatment but there is no consensus on the nature of treatment.
-For class 1 and 2 lesions, conservative local treatment with application of hot or cold compresses depending on the nature of the extravasated molecules.
It should be noted that cold compresses are contraindicated in vasoconstrictor agents such as vinca alkaloids (vincristine, etoposide, vinblastine, teniposide) and catecholamines (dopamine, dobutamine, epinephrine, norepinephrine, phenylephrine), so hot compresses should be applied in such agents [10].
Some authors advocate the use of antidotes. In the pharmacological management of extravasation injuries, several medications have proven to be ineffective, including antihistamines, heparin, sodium bicarbonate, hydrocortisone and glucocorticoids [11] There are a recent experimental study showing satisfactory results of the combination as an antidote to Photobiomodulation (660 nm laser) and hyaluronidases [12].
For class 3 and 4 lesions, surgical advice is necessary. In our patients we proceeded with a conservative treatment consisting of directed healing, antidotes were not available in most cases. only 2 patients benefited from surgical treatment.
Extravasations of solutes to the upper limb are a medico-surgical emergency. Early treatment helps limit functional and aesthetic after-effects in immunocompromised patients, the consequences of which can be serious. Prevention remains the best treatment. For this reason, it is important that the entire medical and paramedical team works in close collaboration from the first signs of extravasation with the aim of rapid and effective treatment of the lesions, hence the need for continuing training of nursing staff regarding theoretical knowledge and appropriate good practices.
Conclusion
This work is the largest series concerning the subject of extravasation of solutes in adults, most of the articles published to date are case reports or reviews of the literature, the large series are published in children or in the neonatology environment, this article aims to highlight this subject for which international standard recommendations are necessary.
Source of Support: Nil
Conflict of Interest: The authors declare that they have no conflicts of interest.
References
- PLANCQ MC. Wounds related to care in pediatric settings. Rev francoph cicatr, 2019; 3(3): 26-31.
- Plushnig U, Haslik W, Bartsch R, Mader RM. Extravasation emergencies: state-of-the-art management and progress in clinical research. Memo, 2016; 9(4): 226–230.
- de Wit M, Ortner P, Lipp HP, et al. Management of cytotoxic extravasation – ASORS expert opinion for diagnosis, prevention and treatment. Onkology, 2013; 36(3): 127–135.
- Fırat C, Erbatur S, Hamdi Aytekin A. Management of extravasation injuries: A retrospective study. J Plast Surg Hand Surg, 2012; 1–6.
- Kostogloudis N, Demiri E, Tsimponis A, et al. Severe extravasation injuries in neonates: a report of 34 cases. Pediatr Dermatol, 2015; 32(6): 830–835.
- Keritam O, Juhasz V, Schöfer C, Thallinger C, Aretin MB, Schabbauer G, et al. Determination of Extravasation Effects of Nal-Iri and Trabectedin and Evaluation of Treatment Options for Trabectedin Extravasation in a Preclinical Animal Model. Front Pharmacol, 2022; 13: 875695.
- Millam DA. Managing complications of IV therapy. Nursing, 1998; 18: 34–43.
- D’Andrea F, Onesti MG, Nicoletti GF, et al. Surgical treatment of ulcers caused by extravasation of cytotoxic drugs. Scand J Plast Reconstr Surg Hand Surg, 2004; 38: 288–292.
- Onesti MG, Carella S, Fioramonti P, Scuderi N. Chemotherapy Extravasation Management: 21-Year Experience. Ann. Surg, 2017; 79: 450–457. doi: 10.1097/SAP.0000000000001248.
- Langstein HN, Duman H, Seelig D. Retrospective study of chemotherapeutic extravasation injury management. Ann Plast Surg, 2002; 49: 369-374.
- Hosnuter M, Babuccu O, Kargı E, et al. A medical trauma which occurs frequently in old patients: extravasation injuries classification and treatment approaches. Turk Geriatri Derg, 2005; 8: 101–106.
- Freitas KABDS, Minicucci EM, Silva VFBD, Menozzi BD, Langoni H, Popim RC. Effects of photobiomodulation (660 nm laser) on anthracycline extravasation: An experimental study. Rev Lat Am Enfermagem, 2022; 30: e3693.

