Varicocele as a Cause of Male Infertility
Daghdagh Y1,2,3, Tmiri A1,2,*, Elbadr M1,2, Kbirou A1,2,3, Moataz A1,2,3, Dakir M1,2, Debbagh A1,2 and Aboutaieb R1,2,3
1Urology Department, Ibn Rochd University Hospital Center, Casablanca, Morocco
2Faculty of Medicine and Pharmacy Casablanca, Morocco
3Sexual Health Laboratory, Faculty of Medicine and Pharmacy, Hassan II University, Casablanca, Morocco
Received Date: 03/03/2024; Published Date: 12/07/2024
*Corresponding author: Anas Tmiri, Department of Urology, Ibn Rochd University Hospital Center, Casablanca, Morocco
Summary
Varicocele is a common pathology that can affect different age groups and can cause male infertility. The origin of varicocele is multifactorial, the diagnosis is clinical coupled with scrotal Doppler ultrasound which remains the gold standard for the diagnosis of varicocele. However, its treatment is simple and often effective, hence the importance of knowing how to recognize and classify it.
We represent a series of cases of 29 patients treated for varicocele in the urology department of the IBN ROCHD CASABLANCA University Hospital during the period from January 1, 2022 to December 31, 2022, having one or more abnormalities on the spermogram.
Keywords: Varicocele; Male infertility; Spermogram; Surgical treatment
Introduction
Varicocele is defined by a dilation of the veins of the pampiniform plexus, it is a common pathology affecting approximately 15% of the male population, which can be responsible for testicular atrophy and infertility. It can be diagnosed clinically but, in some cases, a scrotal Doppler ultrasound may be necessary to confirm it [1,2].
Objective: Describe the impact of varicocele on male fertility in the urology department at the Ibn Rochd University Hospital in Casablanca.
Materials and Methods
- This is a retrospective study of 29 patients treated in the urology department of the IBN ROCHD CASABLANCA University Hospital during the period from January 1, 2022 to December 31, 2022.
- Our study involved a total of 29 patients operated on for varicocele with one or more abnormalities on the spermogram.
- Inclusion criteria: All patients in whom the clinical-radiological diagnosis of varicocele was made and treated surgically during the study period were included.
- Exclusion criteria: Patients lost to follow-up. Patients not treated surgically (Patients without repercussions clinical and/or biological: normal testicular volume, normal spermogram).
Results
- The average age of the patients was 30.36 years with extremes of 20 and 50 years. The most represented age groups were those 25-30 years old with (37.93%).
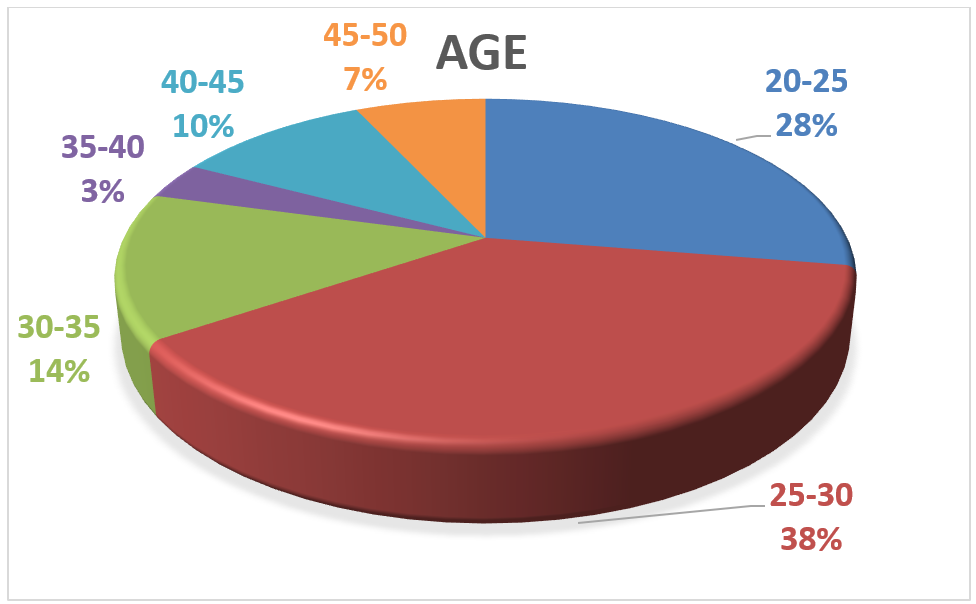
Figure 1: Distribution of patients according to age.
- The reason for consultation in our study was:
- Scrotal pain increased or triggered by exercise, the intensity of which varies in 33% of cases.
- Scrotal heaviness in 25% of cases.
- Primary infertility in 20% of cases.
- The large bursa and testicular swelling in 9% of cases.
- Secondary infertility and accidental discovery in 2% of cases.
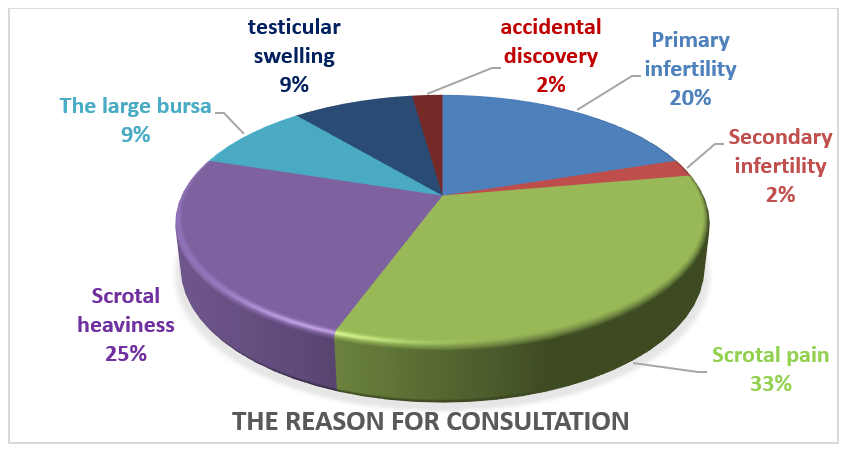
Figure 2: Distribution of patients according to reason for consultation.
- Left varicocele in 96.55% of cases (n=28).
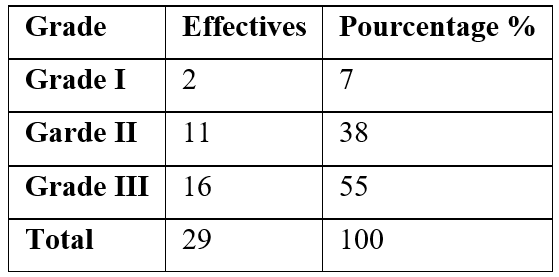
- According to the classification of Dubin and Amelar, the following grades were noted Grade 3: 55% (n = 16); Grade 2: 38% (n = 11) and Grade 1: 7% (n = 2).
Table 1 : Varicocele grade.
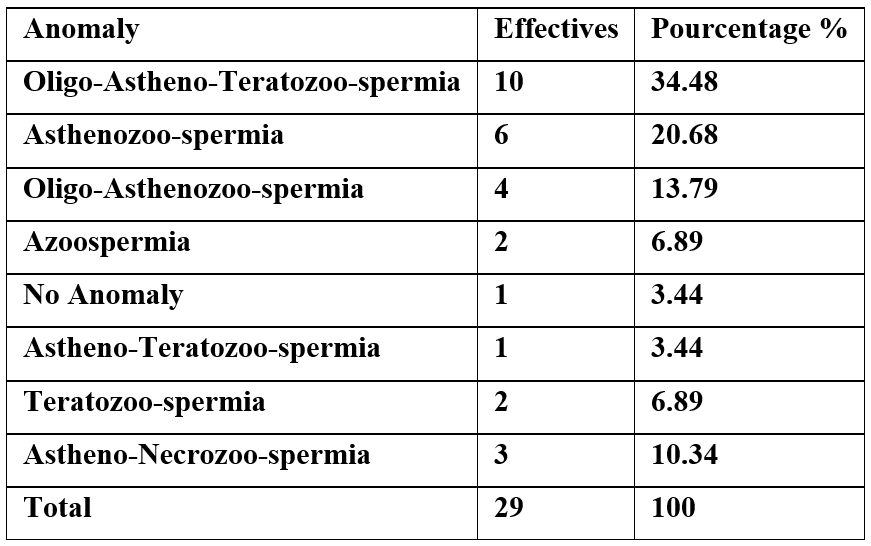
- Biologically, oligo-astheno-teratozoospermia with 34.48% (n = 10) of cases was the most common anomaly.
Table 2: Distribution of patients according to cytospermiological abnormalities.
- Testicular hypotrophy was demonstrated in 6 patients 20.68%, and this hypotrophy was more marked on the left than on the right.
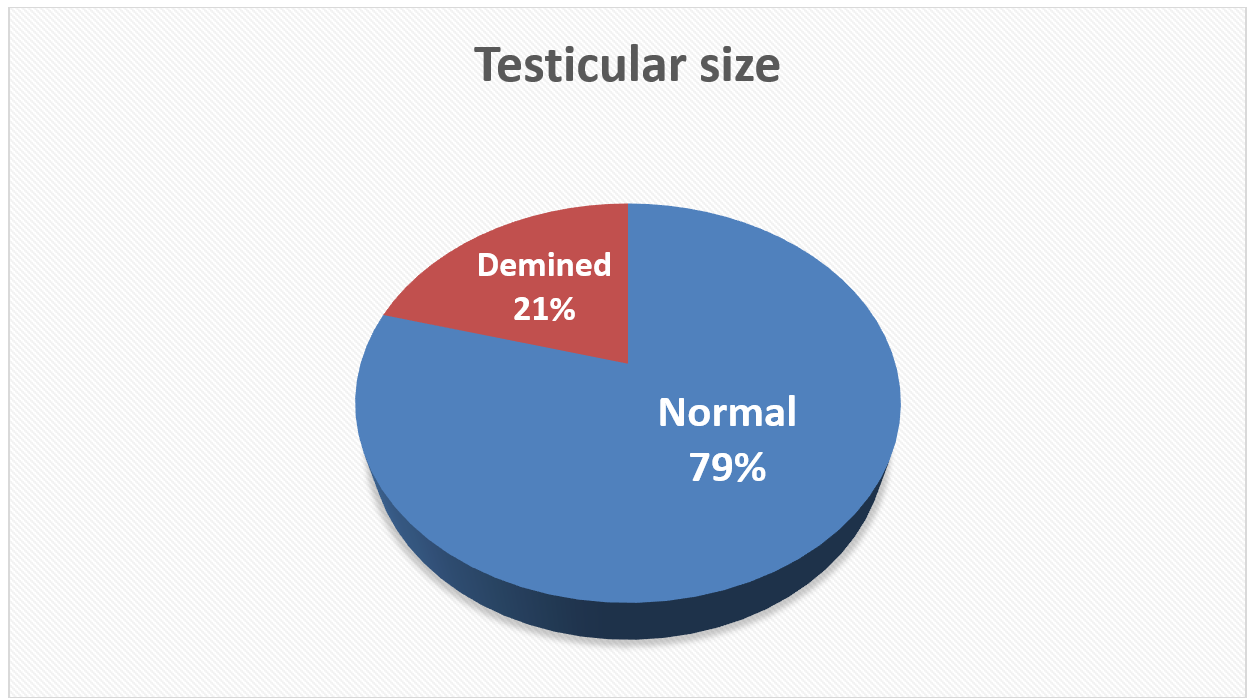
Figure 3 : Testicular size.
- Laparoscopy was the most used technique in almost all of our patients (76.93%).
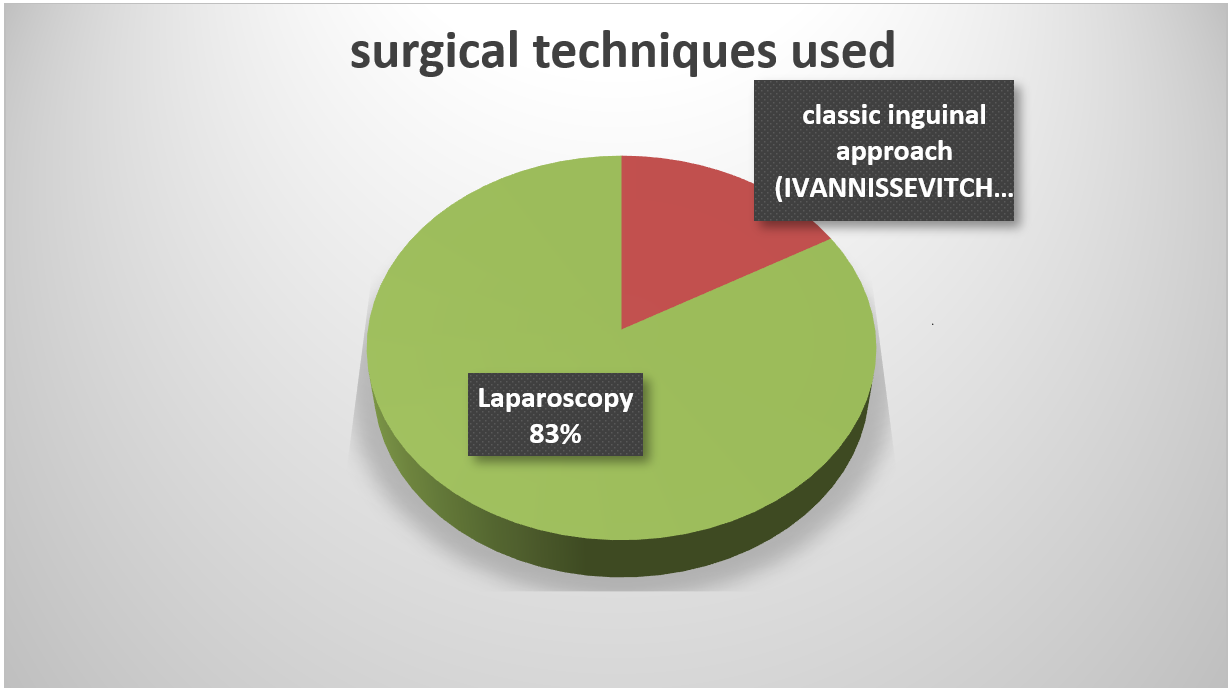
Figure 4: Surgical Techniques.
Discussion
The real impact of varicocele on fertility as well as the benefit of its treatment in the management of male infertility are subjects widely debated in the literature. Infertility is defined as the inability to conceive after one year of frequent unprotected sexual intercourse. It is called primary if the couple has never had a child, secondary if the patient already has one or more children, but cannot conceive a new child [3,4].
The origin of varicocele is multifactorial, the diagnosis is clinical coupled with scrotal Doppler ultrasound which proves to be the reference diagnostic tool, because it is a simple, non-invasive, reproducible and inexpensive examination. Several mechanisms have been proposed to explain infertility but none are really proven. Suggested mechanisms include hypoxia and stasis, testicular venous hypertension, increased temperature, and increased catecholamines in the spermatic vein as well as increased oxidative stress [3-5].
Histological lesions of the testicle in a patient with varicocele affect all cell types and compartments: degeneration and desquamation of germ cells in the lumen of the tubule, arrest of spermatogenesis at different stages, thickening of the basal membrane of the tubes seminiferous cells, vacuolation of Sertoli cells, hyperplasia or more rarely atrophy of Leydig cells, degenerative lesions of capillaries and venules (endothelial hypertrophy, luminal narrowing, thickening of the basement membrane) [6].
Testicular hypotrophy is one of the recognized consequences of varicocele in adolescents and adults. Measuring testicular volume to look for hypotrophy is an essential step in the care of an adolescent with a varicocele. The volume of a normal testicle before puberty is 1 to 2 ml. A volume greater than 3 ml indicates the start of puberty. During puberty, testicular volume increases. The frequency of testicular hypotrophy is variously appreciated from 29% to 87% [7].
In our study, the testicular hypotrophy was in 20.68%, and this hypotrophy was more marked on the left than on the right.
The biological assessment of a patient consulting for varicocele with infertility should include the spermogram which remains the first-line examination in the assessment of the infertile man associated with a dosage of pituitary stimuli (FSH/LH) and a dosage of testosterone serum. FSH regulates spermatogenesis and its level usually increases in secretory infertility. LH regulates the blood level of androgens and testosterone has a fundamental trophic and functional effect on the seminal pathway [8,9].
Semen analysis reveals oligozoospermia, generally with low motility of sperm (asthenozoospermia) and a lower than normal proportion of sperm with normal morphology (teratozoospermia) [10,11].
Oligo-astheno-teratozoospermia constituted the most common cytospermiological anomaly found in our series of cases, with 34.48% of cases.
The objective of treatment is to stop testicular suffering or to reverse the growth deficit of the testicle, especially during puberty and thus preserve the patient's fertility. Treatment of varicocele should only be offered if all of the following conditions are present: The varicocele is palpable, the couple's infertility is documented, there is no female infertility problem or it is potentially curable, there is at least one abnormality of sperm parameters in the spermogram. Improvement in the spermogram is seen in nearly 70% of operated patients. It is mainly mobility which is improved (70%) then concentration (51%) and in 44% of patients the morphology of the spermatozoa according to the literature [12,13].
Medical treatments are indicated above all to correct possible hormonal insufficiency. A period of supervision is almost always justified in adolescents. Not only does it belong to a given severity stage of the varicocele which guides the therapeutic decision, but also the evolutionary path. We must never forget that in the post-pubertal phase, a certain number of varicoceles stabilize or even partially regress. Medical treatment can be designed either in isolation or in association with surgical or percutaneous interruption of spermatic reflux [14].
Various therapeutic options are known for the treatment of a varicocele, both open surgical, microsurgical and radio-interventional. Each technique has its own advantages and disadvantages, and conflicting results have been obtained in different studies, but to date there has been no consensus as to which technique should be considered the gold standard for varicocele treatment [15,16].
A study conducted from January 2012 to January 2018 at Split University Hospital, Spinciceva in Croatia which compared open varicocele treatment versus laparoscopy demonstrated that the laparoscopic approach has a significantly lower rate of postoperative complications and recurrences. as well as a shorter operating time compared to the open approach. Faster recovery and shorter hospitalization are also noted after a laparoscopic approach, however no statistically significant difference between supra-inguinal, infra-inguinal or inguinal varicocele treatment regarding the total number and motility of spermatozoa in the spermogram and that all operating techniques led to a statistically significant improvement in the spermogram [16].
In our case series, the laparoscopic approach was the most used technique in almost all of our patients (76.93%).
Several studies have shown that men with grade 3 varicoceles have greater improvements in semen parameters than men with grades 1 and 2 varicoceles after varicocele repair [17].
Conclusion
Varicocele is a curable and reversible cause of male infertility. Its diagnosis is generally clinical. However, in certain cases where the diagnosis is not obvious, the use of imaging is necessary to confirm or refute its presence.
References
- Alsaikhan B, Alrabeeah K, Delouya G, Zini A. Epidemiology of varicocele. Asian J Androl, 2016; 18(2): 179-181. doi:10.4103/1008-682X.172640.
- Ghandehari-Alavijeh R, Tavalaee M, Zohrabi D, Foroozan-Broojeni S, Abbasi H, Nasr-Esfahani MH. Hypoxia pathway has more impact than inflammation pathway on etiology of infertile men with varicocele. Andrologia, 2019; 51(2): e13189. doi:10.1111/and.13189.
- Huyghe E, Methorst C, Faix A. Varicocèle et infertilité masculine. Progrès en Urologie, 2023; 33(13): 624-635. doi: 10.1016/j.purol.2023.09.003.
- Schlosser J, Nakib I, Carré-Pigeon F, Staerman F. Infertilité masculine: définition et physiopathologie. Annales d’Urologie, 2007; 41(3): 127-133. doi: 10.1016/j.anuro.2007.02.004.
- Wagner L, Tostain J. Varicocèle et infertilité masculine : Recommandations Comité Andrologie - AFU 2006. Progrès en Urologie, 2007; 17(1): 12-17. doi: 10.1016/S1166-7087(07)92219-8.
- Artyukhin AA. Anatomy and microanatomy of the venous system of scrotal organs and spermatic cord. Bull Exp Biol Med, 2007; 143(1): 99-104. doi: 10.1007/s10517-007-0027-9.
- Moldovan I, Popescu V. [Etiopathogenesis of varicocele and therapeutic conclusions]. J Chir (Paris), 1976; 111(3): 319-334.
- Kühn AL, Scortegagna E, Nowitzki KM, Kim YH. Ultrasonography of the scrotum in adults. Ultrasonography, 2016; 35(3): 180-197. doi: 10.14366/usg.15075.
- Middleton WD, Dahiya N, Naughton CK, Teefey SA, Siegel CA. High-resolution sonography of the normal extrapelvic vas deferens. J Ultrasound Med, 2009; 28(7): 839-846. doi: 10.7863/jum.2009.28.7.839.
- Vanlangenhove P, Dhondt E, Van Maele G, Van Waesberghe S, Delanghe E, Defreyne L. Internal Spermatic Vein Insufficiency in Varicoceles: A Different Entity in Adults and Adolescents? AJR Am J Roentgenol, 2015; 205(3): 667-675. doi: 10.2214/AJR.14.14085.
- Ahlberg NE, Bartley O, Chidekel N, Fritjofsson A. Phlebography in varicocele scroti. Acta Radiol Diagn (Stockh), 1966; 4(5): 517-528. doi: 10.1177/028418516600400506.
- Steeno O, Knops J, Declerck L, Adimoelja A, van de Voorde H. Prevention of fertility disorders by detection and treatment of varicocele at school and college age. Andrologia, 1976; 8(1): 47-53. doi: 10.1111/j.1439-0272.1976.tb01645.x.
- Sofikitis N, Dritsas K, Miyagawa I, Koutselinis A. Anatomical characteristics of the left testicular venous system in man. Arch Androl, 1993; 30(2): 79-85. doi: 10.3109/01485019308987738.
- Karmazyn B. Scrotal Ultrasound. Ultrasound Clinics, 2010; 5(1): 61-74. doi: 10.1016/j.cult.2009.11.009.
- Langenauer J, Schwab C. Die Varikozele – Wann und wie soll behandelt werden? Urol Prax, 2020; 22(2): 36-41. doi: 10.1007/s41973-020-00092-0.
- Jukic M, Todoric M, Todoric J, Susnjar T, Pogorelic Z. Laparoscopic Versus Open High Ligation for Adolescent Varicocele: A 6-year Single Center Study. Indian Pediatr, 2019; 56(8): 653-658.
- Lehner K, Ingram C, Bansal U, et al. Color Doppler ultrasound imaging in varicoceles: Is the difference in venous diameter encountered during Valsalva predictive of palpable varicocele grade? Asian J Urol, 2023; 10(1): 27-32. doi: 10.1016/j.ajur.2021.12.006.

