Epidemioclinical and Dermoscopic Aspects of Darier Disease
Rym Zmiti*, Anissa Zaouak, Amal Chamli, Samy Fenniche and Houda Hammami
Dermatology department, Habib Thameur Hospital, Tunisia
Received Date: 15/02/2024; Published Date: 03/07/2024
*Corresponding author: Rym Zmiti, Dermatology department, Habib Thameur Hospital, Tunis, Tunisia
Abstract
Introduction: Darier's Disease (DD) is an autosomal dominant genodermatosis. We report the dermoscopic aspects in 5 patients.
Materials and Methods: Prospective study conducted at the dermatology department of Habib Thameur Hospital from January to March 2022, including 5 patients followed for DD for whom we performed a dermoscopic examination using the manual DermLite DL4 dermoscope.
Results: We included 5 patients followed for DD. The mean age was 33 years with extreme ages ranging from [18-48 years]. The male-to-female ratio was 0.25 (1 male and 4 females). The most common dermoscopic characteristic of keratotic papules was a central yellowish/brownish area, surrounded by a more or less wide area of thin whitish halo located in seborrheic areas. The yellowish/brownish central area had a polygonal shape in two patients and a star morphology in the other two. Dotted and linear vessels were also observed. The found ungual dermoscopic aspects included distal onycholysis in roller coaster pattern, erythronychia, distal V, and sugar cane aspect. Trichoscopic aspects found included rosette appearance in a patient with hyperkeratotic Darier's disease with severe alopecia. Keratotic plugs, significant erythema, hemorrhagic crusts, broken hairs, and flame hairs were also observed.
Conclusion: Dermoscopy can be considered a useful complementary support to distinguish DD from its other main clinical differential diagnoses. The rosette appearance in a four-leaf clover seen in our patient with severe alopecia would be correlated with severe forms of DD.
Keywords: Darier disease, Epidemioclinical ,dermoscopic aspects
Introduction
Darier Disease (DD) is an autosomal dominant genodermatosis. It is an acantholytic and dyskeratotic dermatosis linked to intrinsic lesions of the interkeratinocyte adhesion systems.
Clinically, it manifests as papulokeratotic lesions predominating in seborrheic areas and acral involvement with nail lesions. We report on the dermoscopic aspects of 5 patients treated for Darier's disease in our department.
Materials and Methods
Prospective study conducted in the dermatology department of Habib Thameur Hospital, colligeant 5 patients followed for DD for whom Both polarized and non-polarized dermoscopy were used. DermLite DL4 dermatoscope was employed. Pictures were taken using Canon SX710HS digital camera.
Results
We collected 5 patients followed for DD. Mean age was 33 years with extremes [18-48 years]. Sex ratio M/F =0.25 (1 man and 4 women). Four patients were from consanguineous marriages. A family history of DD was present in 3 patients. Clinical appearance ranged from multiple confluent brownish and grayish keratotic papules in placards to patchy erosive yellowish papuloverrucous lesions. These lesions were located on the face, lateral sides of the neck, axillary folds, inguinal folds and sub- and intermammary folds, and palmoplantar pits were present in 2 patients. Nail striations with alternating white and red longitudinal stripes, notches on the distal free edges of fingernails and toenails, and a scaly, keratotic shell on the scalp. Alopecia was noted in two patients, and was severe in one.
The most frequent dermoscopic feature (all patients) was a yellowish/brownish central zone, corresponding histopathologically to hyperparakeratosis, surrounded by a more or less wide zone of thin whitish halo. The yellowish/brown central zone was polygonal in shape in two patients and star-shaped in the other two. A rosette-like appearance was observed in two patients. Dotted and linear vessels were also observed.
Trichoscopic findings: keratotic plugs, severe erythema, haemorrhagic crust, broken hair, flaming hair.
Onychoscopic findings: distal roller-coaster onycholysis was observed in 3 patients , erythronychia and distal V was found in 4 cases, and sugar-cane appearance found in 2 patients.
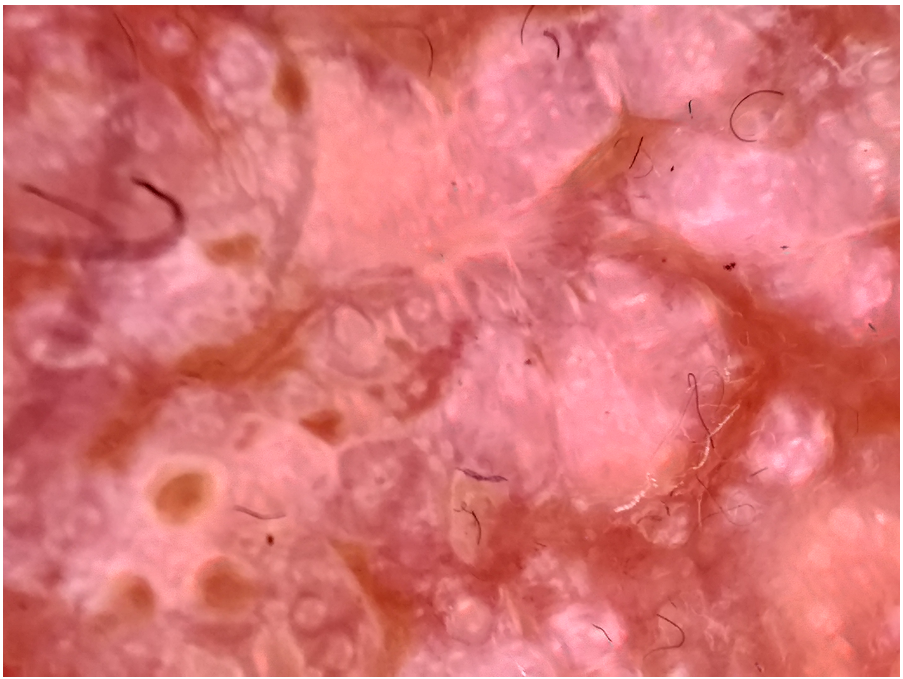
Figure1: Yellowish/brownish central zone, surrounded by a more or less wide zone of thin whitish halo.
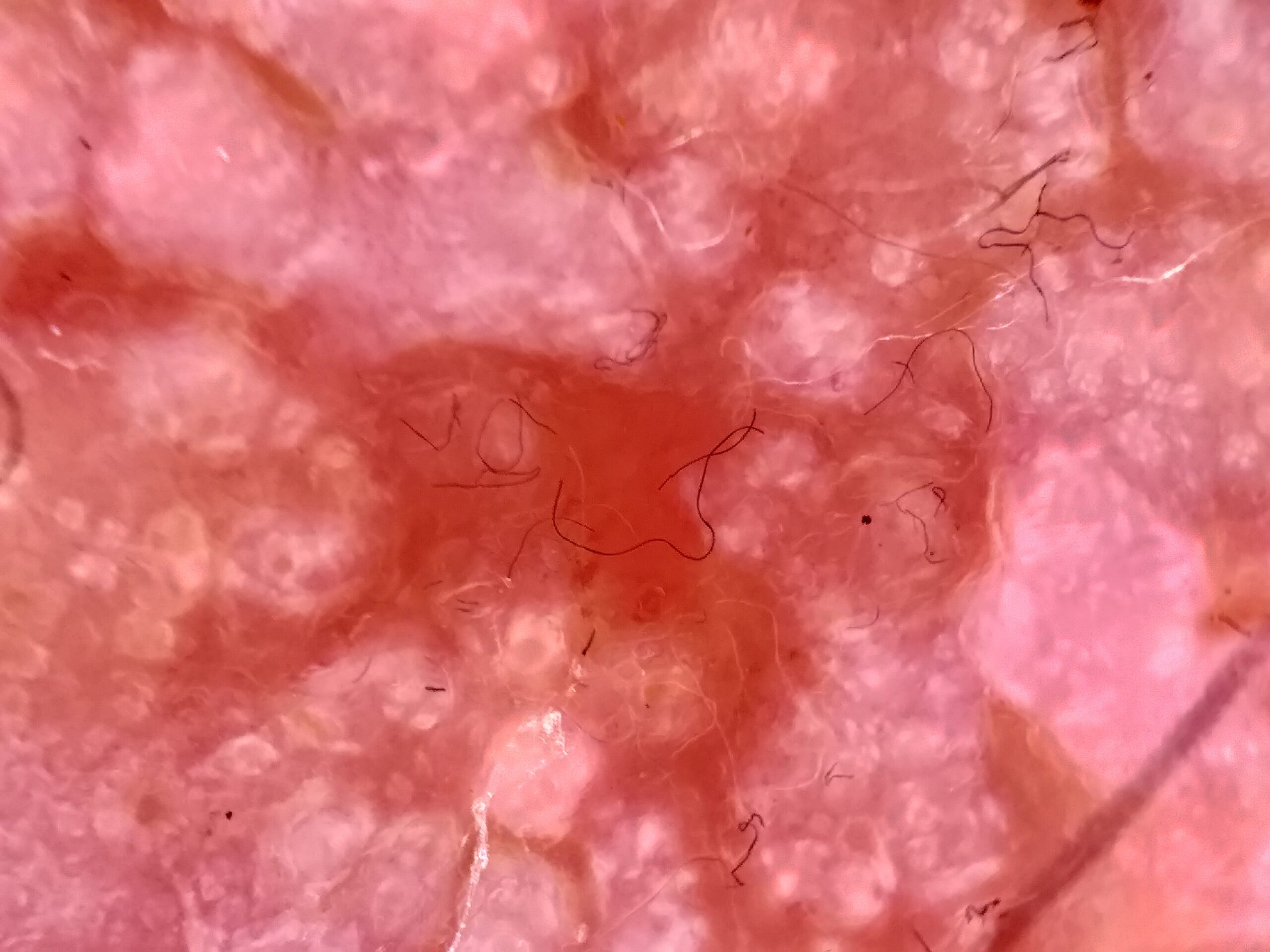
Figure 2: A rosette-like appearance.

Figure 3: Dotted and linear vessels.
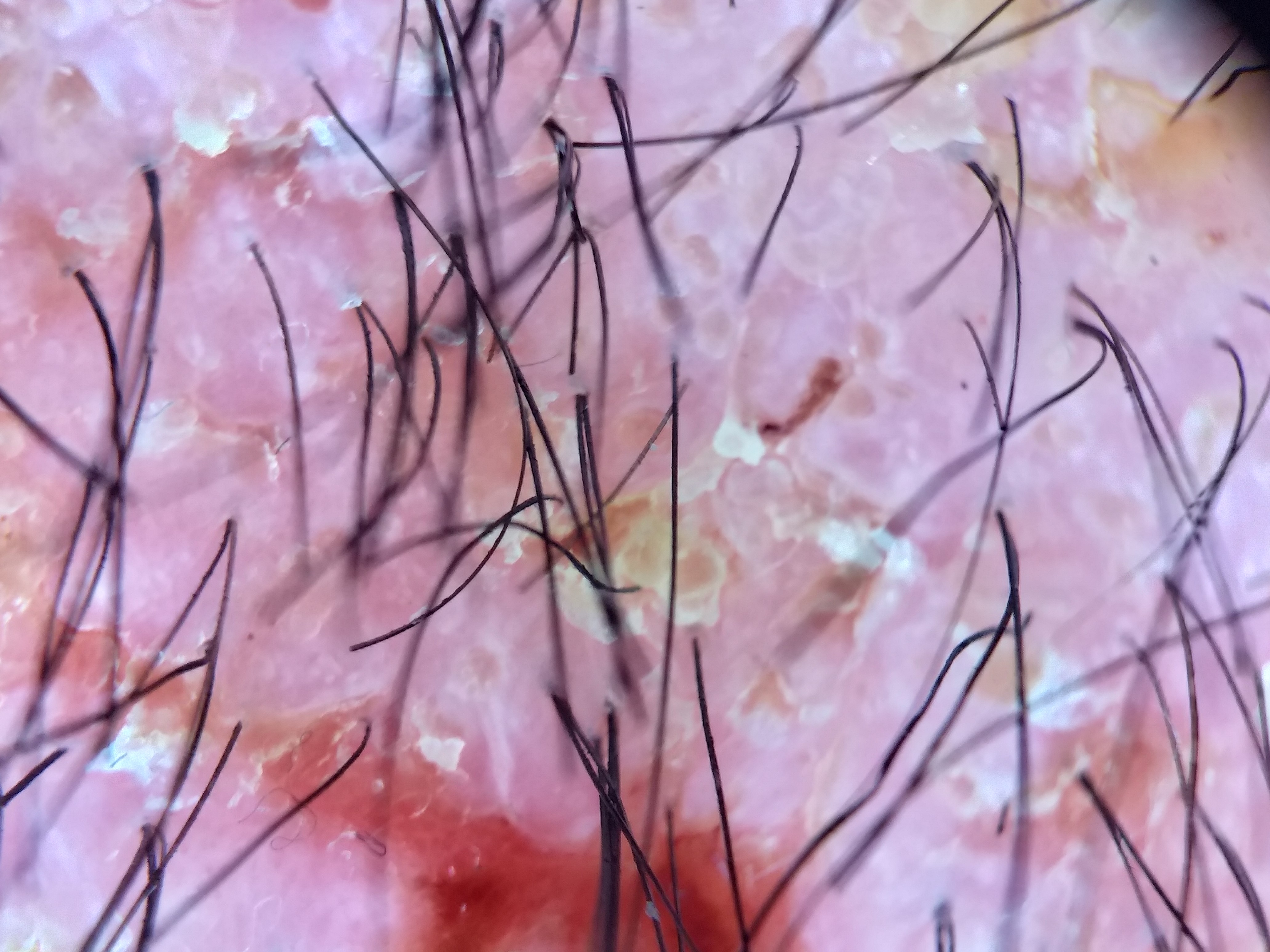
Figure 4: Keratotic plugs, severe erythema, haemorrhagic crust, broken hair, flaming hair.

Figure 5: Sugar-cane appearance.

Figure 6: Distal roller-coaster onycholysis.

Figure 7: Erythronychia and distal V.
Discussion
Pseudocomedons", i.e. dilated oval openings with raised or flat margins and central brown or yellowish hyperkeratosis, are the dermoscopic features most frequently described in the literature in DD [1].
According to our study, and as in the study by E. Errichetti et al, the dermoscopy of MD should not be identified solely by the presence of pseudocomedons, but consists of a more complex pattern characterized by a central yellowish/brown polygonal star-shaped or oval area surrounded by a more or less fine whitish halo, overlying a homogeneous pinkish area without structure, with or without whitish scales and dotted and/or linear vessels presenting a whitish halo[2] . Several other dermoscopic aspects that may be present and should attract attention: Rosette appearance, distal roller-coaster onycholysis, erythronychia, distal V, sugar-cane appearance, keratotic plugs, severe erythema, hemorrhagic crust, broken hair and flaming hair.[3] The dermoscopic findings detected in our DD patients are similar to those of other acantholytic and dyskeratotic disorders, including acantholytic dyskeratotic acanthoma, dyskeratosis and Grover’s disease; such a finding is easily explained by their histopathological similitude.[4]
Dermoscopic nail findings included distal roller-coaster onycholysis, V-shaped notching of distal margin and sugar-cane appearance. Were reported in other studies associated to multinucleated giant cells present [5,6].
However, no study was interested in showing the trichoscopic aspects of darier’s disease.
Conclusion
Dermoscopy can be considered a useful complementary aid in distinguishing DD from its other main clinical differential diagnoses, including acne, which classically presents with pustules with an erythematous halo and comedones, infectious folliculitis, seborrheic dermatitis, confluent and reticulated papillomatosis, pityriasis rubra pilaris, chronic lichenoid pityriasis.
Author Contributions: All authors contributed to conceptualization, writing, and editing of this review. They have read and agreed to the published version of the manuscript.
Funding: No funding was utilized in writing this review.
Ethical statement: The patients gave their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki.
Conflicts of Interest: The authors declare no conflict of interest.
References
- Errichetti E, Stinco G, Lacarrubba F, Micali G. Dermoscopy of Darier’s disease. J Eur Acad Dermatol Venereol, 2016; 30(8): 1392‑1394.
- Errichetti E, Maione V, Pegolo E, Stinco G. Dermoscopy: a useful auxiliary tool in the diagnosis of type 1 segmental Darier’s disease. Dermatol Pract Concept, 2016; 6(2): 53‑55.
- Lacarrubba F, Verzì AE, Errichetti E, Stinco G, Micali G. Darier disease: Dermoscopy, confocal microscopy, and histologic correlations. J Am Acad Dermatol, 2015; 73(3): e97-99.
- Giacomel J, Zalaudek I, Argenziano G. Dermatoscopy of Grover’s disease and solitary acantholytic dyskeratoma shows a brown, star-like pattern. Australas J Dermatol, 2012; 53(4): 315‑316.
- Navarro L. Pattern diagnosis of onycholysis. JEADV Clinical Practice, 2023; 2(2): 213‑224.
- Habif’s Clinical Dermatology, 7th Edition - 9780323612692, 2023.

