MRI Aspects of ACL Mucoid Degeneration Through a 5 Cases Series
Jidal M*, Mesbah O, Saouab R and El Fenni J
Radiology department, Children’s hospital, Mohammed V university, Rabat, Morocco
Received Date: 26/12/2023; Published Date: 13/05/2024
*Corresponding author: Manal JIDAL, Radiologydepartment, Children’s hospital, Mohammed V University of Rabat, Morocco
Introduction
Anterior Cruciate Ligament (ACL) mucoid degeneration is a rare process that has been described in a few reports. The pathogenesis of this condition remains controversial. There are no fixed clusters of symptoms that are pathognomonic. They could be asymptomatic and discovered incidentally while exploring other pathologies of the knee, and when symptomatic, the patients usually report chronic knee pain and restriction in the range of motion. They do not complain of knee instability, and the Lachman test is typically negative [1]. Magnetic resonance imaging is the mainstay of diagnostic imaging.
Case Reports
We report 5 cases of patients with mucoid degeneration of the anterior cruciate ligament, mainly women (4 women and a man). The average age was 43 years old, with extremes ranging from 35 to 65 years old. The duration of symptoms varied between 6 months to a year. None of the patients had a history of trauma. The main symptom was knee pain: mostly posterior for 4 of our patients, and postero-medial in one case; as well as difficulty in knee flexion, while extension remained unaffected. No positive sign or symptoms of knee instability are noted, and the Lachman test was negative. Knee MRIs showed imaging criteria for mucoid degeneration, including a bulky and thickened ACL (Figure 1) that maintained its normal orientation and continuity of its fibers, increased intensity (Figure 2 and 4) on all sequences, and celery stalk appearance. Associated moderate joint effusion was noted in 3 cases. One patient had osteoarthritic changes in the medial compartment as well as a meniscal tear (Figure 3). And one patient had an ACL ganglion cyst associated with the mucoid degeneration of the ACL (Figure 5).
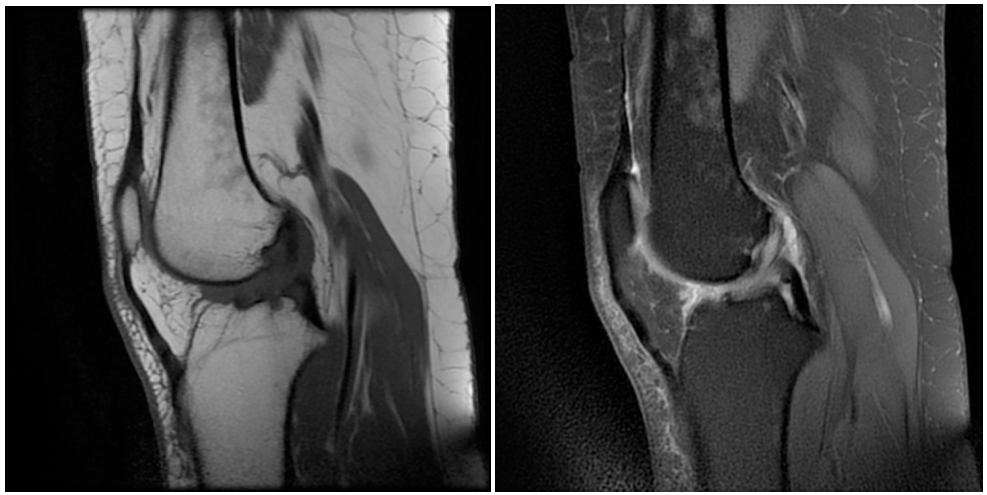
Figure 1 : a) Mucoid degeneration of ACL. b) The sagittal proton density weighted T1 and FS T2 showing a bulky ill defined ACL.
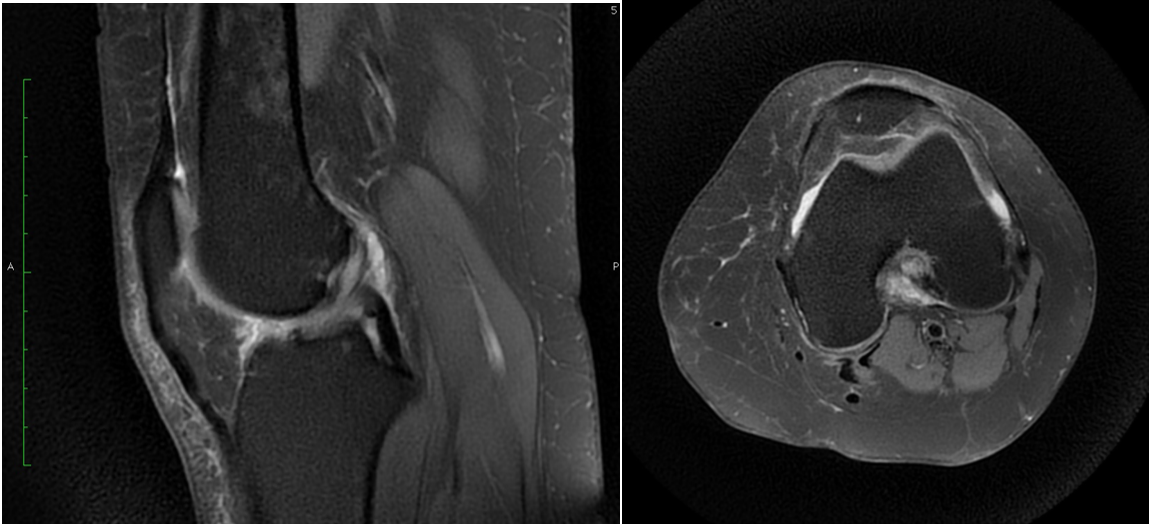
Figure 2 : Axial and sagittal T2 FS weighted images, showing the increased signal of a bulky ACL.
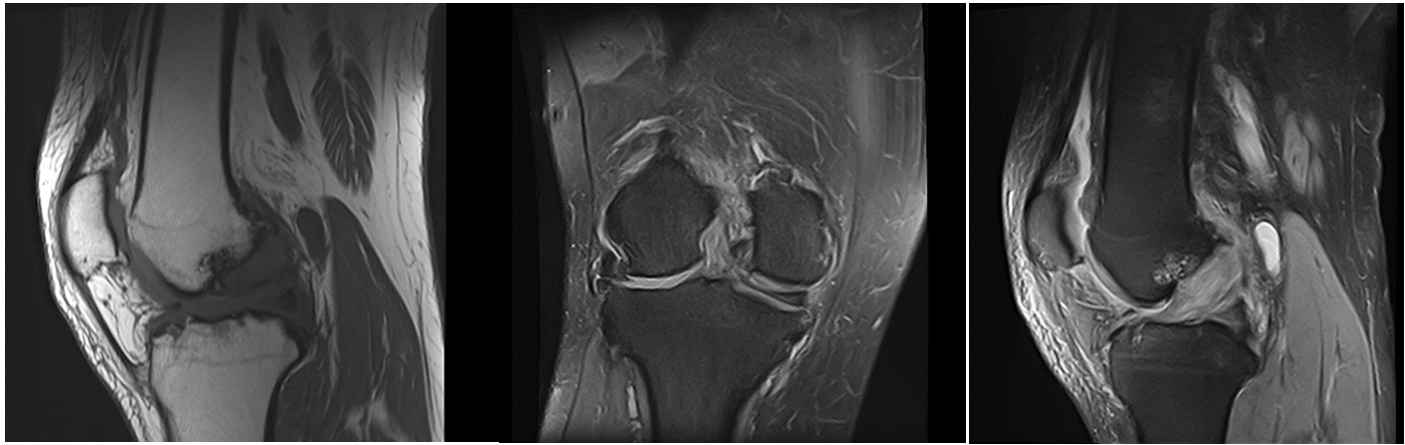
Figure 3: a) Sagittal T1W images showing a bulky and ill defined ACL associated with osteroarthritis changes. b) Sagittal and coronal proton density weighted images showing ACL mucoid degeneration associated with meniscal tear.
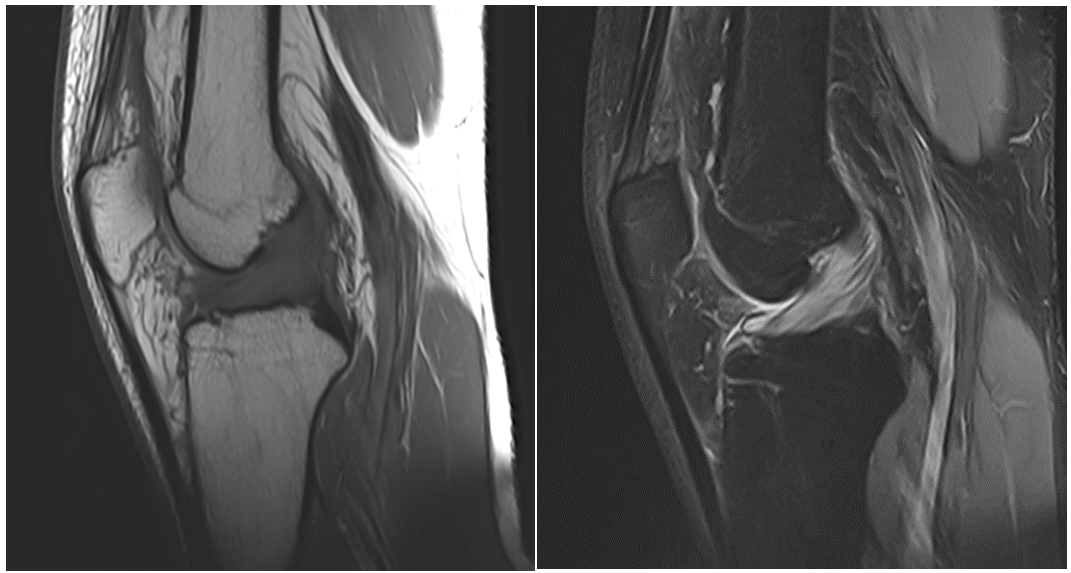
Figure 4: Sagittal T1 and T2 FS weighted imaging showing a bulky and ill defined ACL, with an increase of its intensity on both sequences.
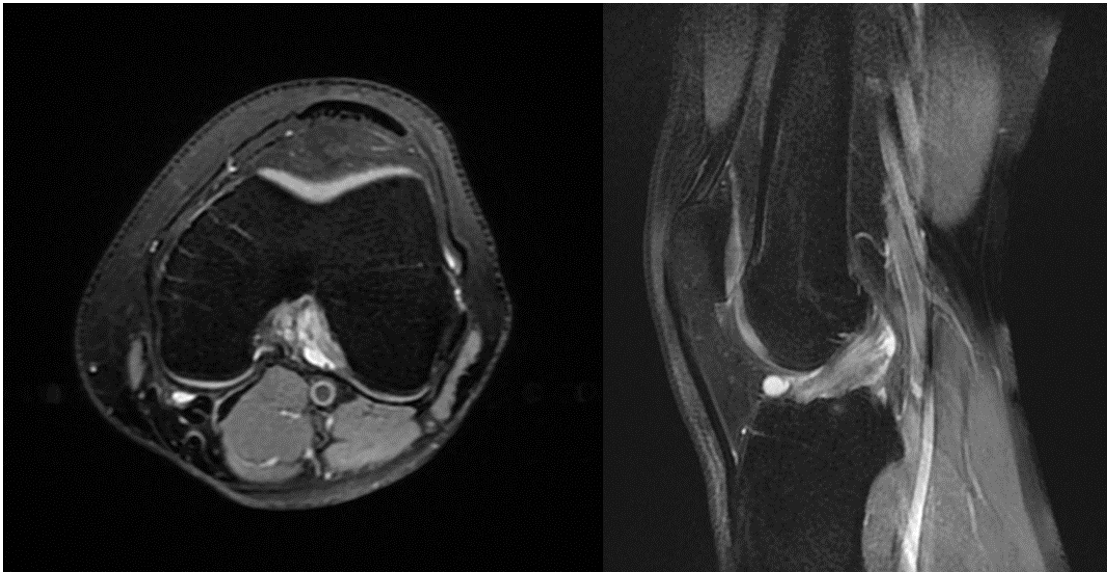
Figure 5: a) Mucoid degeneration associated with ganglio cyst. b) Axial and sagittal proton density weighted images showing a mucoid degeneration of the ACL associated with a ganglio cyst of the ACL.
Discussion
Mucoid degeneration of the ACL was first described by Caan in 1924 in his anatomopathological studies for ACL tears. It remains a rare pathology, often misinterpreted as a rupture of the ACL on MRI in current practice. It is mostly a pathology of young adults, responsible for posterior knee pain and restriction in the range of motion [2].
Many theories have been put forth to explain the pathological disorganization in the collagen fibers of the Anterior Cruciate Ligament [3]. Some suggest that it may be caused by the accumulation of synovial fluid inside the substance of ACL in a herniated pouch of synovium, known as the synovial theory. The traumatic theory postulates the accumulation of the mucin substance secreted by fibroblasts within the ACL, post-injury; or that multiple micro traumas result in the formation of microcysts which eventually merge into large mucoid formations. The degenerative theory suggests that mucoid degeneration could simply occur due to aging. Finally, the ectopic theory stipulates that ectopic synovial tissue could exist inside ACL substance leading to microcyst formation [3].
The most common and consistent symptom is an insidious onset chronic knee pain, mostly posterior. Symptoms may also include discomfort during mobilization, a meniscus pain point, or limitation in the range of motion, directing the diagnosis to another intra-articular lesion such as a meniscus lesion, cartilage lesion, or a foreign body [4]. The duration of symptoms may vary from weeks to months. Most patients have no history of trauma, and when present, it is usually trivial [2]. Symptoms such as pain and limitation in the range of motion are hypothetically due to an increase in tension and volume of the ACL, mechanical impingement on the PCL and posterior capsule, causing bone erosion, or, as mentioned in some studies, due to disturbance in nociceptive properties [2,3].
The Lachman test, anterior drawer test, and pivot shift test are most of the time negative. Joint line tenderness and limitation of movement during clinical examination might be the only findings. Indeed, all our patients complained of posterior knee pain increasing with knee flexion, and none of them reported knee instability or extension block.
These clinical features are not pathognomonic and do not respond to treatment with NSAIDs and physiotherapy. However, they should raise suspicion and the need for further evaluation with MRI [2].
Conventional x-rays might reveal osteoarthritic changes but are not helpful for the diagnosis, whereas the gold standard imaging is MRI [4].
A few features found on MRIs are suggestive of ACL mucoid degeneration [4,5]:
A thickened, ill-defined, and bulky ACL maintaining its normal orientation and the continuity of its fibers.
An increased intra-ligamentous signal on all sequences as it shows an intermediate signal on T1-weighted images and high signal on T2-weighted images and proton density-weighted images.
The celery stalk sign consisting of subtle linear low signal intensity fibers parallel to the long axis of the otherwise hyperintense ligament (celery stalk sign).
ACL Mucoid degeneration might coexist with an ACL ganglion cyst and is many times associated with meniscal tears, chondral damage, or intraosseous cysts [5].
The most frequent error is mistaking mucoid degeneration for a tear of the ACL, which is the main differential diagnosis. But clinical correlation is crucial and can help rule out a ligamentous tear when patients neither have a history of trauma or instability, nor do they present a secondary stigma of a ruptured ACL such as bone bruises or anterior tibial subluxation [5].
Arthroscopic debridement of the mucoid degeneration of the ACL is the main treatment and is considered safe and effective [6].
Conclusion
Mucoid degeneration of the anterior cruciate ligament is a rare non-traumatic lesion that remains little known and is often mistaken for an ACL tear. It should be suspected in the face of unexplained posterior pain of the knee. This pathology has a very characteristic appearance on MRI, which is the gold standard for radiological diagnosis.
References
- Vaishya R, Esin Issa A, Agarwal A, et al. Anterior Cruciate Ligament Ganglion Cyst and Mucoid Degeneration: A Review. Cureus, 2017; 9(9): e1682. doi:10.7759/cureus.1682
- Demey G, Servien E, Aït Si Selmi T, Neyret P. Les kystes du ligament croisé antérieur: à propos de 24 cas. Journal de Traumatologie Du Sport, 2007; 24(1): 11–17. doi:10.1016/j.jts.2007.01.006
- Pandey V, Suman C, Sharma S, Rao S, Kiran Acharya K, et al. Mucoid degeneration of the anterior cruciate ligament: Management and outcome. Indian Journal of Orthopaedics, 2014; 48(2): 197.doi:10.4103/0019-5413.128765
- Lintz F, Pujol N, Boisrenoult P, Bargoin K, Beaufils P, Dejour D. Anterior cruciate ligament mucoid degeneration: a review of the literature and management guidelines. Knee Surgery, Sports Traumatology, Arthroscopy, 2011; 19(8): 1326–1333. doi:10.1007/s00167-011-1433-0
- Matrawy KA, El-Nekeidy A E-A M, Al-Dawody A. Mucoid degeneration of the anterior cruciate ligament: frequently under-diagnosed entity in MRI. The Egyptian Journal of Radiology and Nuclear Medicine, 2012; 43(2): 227–233.doi:10.1016/j.ejrnm.2012.03.002
- Hsu C-J, Wang S-C, Fong Y-C, Huang C-Y, Chiang I-P, Hsu H-C. Mucoid Degeneration of the Anterior Cruciate Ligament. Journal of the Chinese Medical Association, 2006; 69(9): 449–452. doi:10.1016/s1726-4901(09)70290-4

