“Neurodynamics in LBP: A Case Series”
Rebecca Story Dunbar, PT, DPT, MTC, Cert. DN* and Jeananne Elkins, PT, PhD, DPT, MPH
College of Professional Studies, Northeastern University, USA
Received Date: 29/05/2023; Published Date: 28/09/2023
*Corresponding author: Rebecca Story Dunbar, College of Professional Studies, Northeastern University, USA
Introduction
Acute Low Back Pain (LBP), the number one cause of disability in the world, often resolves in weeks to months, however, about one third of people with LBP experience ongoing pain and dysfunction [1]. Providers are often unable to agree on the best approach to treat LBP. Many treatments and interventions including injections, medications, physical therapy, chiropractic, massage, and acupuncture have been and are used to treat LBP although most are not effective. Systematic reviews, meta-analysis and Cochrane reviews have identified education, anti-inflammatories, and manual therapy as the most effective treatments for LBP [2].
While manual therapy has demonstrated effectiveness in the treatment of LBP in numerous peer-reviewed publications, implementation of a standardized program of manual therapy in the clinical setting may not be as effective. In part, this is due to the lack of standardization of manual therapy in research studies, the lack of inter-rater and intra-rater reliability and the neglect of the neurological components of LBP [2]. Additionally, manual therapy treatments may reproduce a patient’s symptoms and, therefore, affect patient tolerance and adherence to physical therapy treatment. However, neurodynamics and neural mobilization is a well-tolerated type of manual therapy as it is performed below the patient’s pain threshold.
Neurodynamics and neural mobilization, a form of manual therapy, is a suitable treatment approach for patients who have dysfunctions of their nervous system including neural tensioning. Neural mobilization addresses the mechanical aspect of nervous system pathologies, whereas, neurodynamics addresses both the mechanical and physiological aspects of the nervous system [3]. Shacklock and colleagues studied mechanical components of neurodynamics and reported decreased stretch sensation on the ipsilateral (IL) side with extension of the contralateral (CL) knee while using the slump test (ST) [4]. This occurs because as the CL lower extremity is moved an additional force is put on the CL nerve root, resulting in a downward movement of the spinal cord. This movement reduces tension on the IL nerve root, and therefore symptoms from it [5].
The specific neurodynamic techniques used in this approach have been explored in the published literature, but the actual patient clinical outcomes of neurodynamic treatments have not been explored in depth. This case series will explore the use of clinical neurodynamics for LBP in an outpatient clinic by using neurodynamic treatment progressions of unloading the nerve root with foramen opening and CL nerve root techniques, followed by loading the nerve root with foramen closing and IL neural tensioners.
Methods
Four patients with lumbosacral radiculopathy were treated at an outpatient physical therapy office from 2019 to 2021 by the author. These patients were selected as they had a history of LBP and signs and symptoms of lumbosacral radiculopathy. Patients with diagnoses involving the central nervous were excluded, as well as patients with a previous history of low back surgery or epidural steroid injections. Patient treatments included, but were not limited to, clinical neurodynamic techniques [5]. Patients whose cases were used were consented for use of their medical records for this case series. Data obtained from the medical record included patient’s subjective reports of pain and dysfunction, patient’s lower extremity deep tendon reflexes, manual muscle testing of bilateral lower extremities for possible myotomal weakness, and standard neurodynamic testing including the ST and SLR as seen in Figure 1.
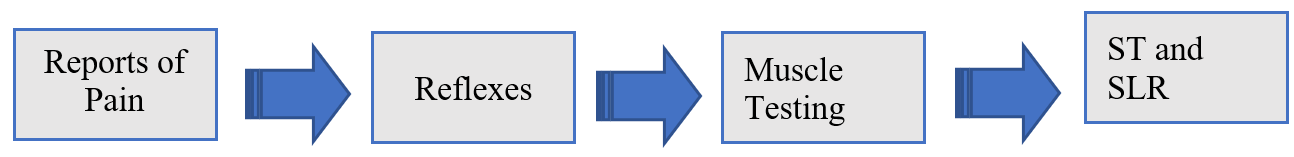
Figure 1: ST and SLR box off center.
Deep tendon reflexes
Deep tendon reflexes were assessed for the lower extremities including the patellar (L4) and ankle reflex (S1). Grading of reflexes is from 0-4. A reflex of 0 is absent, 1 is diminished, 2 is normal, 3 is hyper-reflexive, and 4 is associated with clonus [6].
Manual muscle testing
Manual muscle testing was performed using the Medical Research Council Manual Muscle Testing scale. In this method the muscles are tested in the extremities using a 0-5 rating scale with 0 indicating no muscle activity, 1 being trace muscle activity, 2 muscle activity in a gravity eliminated position but with full range of motion, 3 muscle activity with gravity and full range of motion, 4 muscle activity with some resistance and full range of motion, and 5 muscle activity against full resistance and full range of motion [7].
Neurodynamic testing
Neurodynamic testing was performed including the ST and SLR, and patient response was noted. Structural differentiation was performed to determine if a neurodynamic component was involved. An example included if the therapist performed a SLR test and the patient described feeling low back pain with passive dorsiflexion of the patient’s foot. If the patient did not have a change with the passive dorsiflexion, the low back pain was determined to be musculoskeletal in nature [8].
The following was similar for a ST, whereas, in this example the patient was sitting with thoracic and lumbar flexion and their chin to chest. The therapist then passively extended one of the patient’s knees. The patient was then asked to raise their chin off their chest. If the patient’s low back pain was unchanged despite head position the patient’s pain was deemed to be musculoskeletal in origin. If the patient’s low back changed with head position, the patient’s low back pain was determined to have a neurodynamic component [8].
Abnormal responses
The next step was to determine if the patient had a normal or abnormal response to neurodynamic testing. Abnormal responses were broken down into overt abnormal or covert abnormal responses. Overt responses reproduced the patient’s symptoms, whereas, covert responses did not, but the patient’s range of motion in the IL lower extremity was asymmetrical to their CL lower extremity. If a SLR test was performed and the patient had a reproduction of their LBP that increased with ankle dorsiflexion, this was called an overt abnormal response. Conversely, if a SLR test was performed and the patient did not have a reproduction of their LBP, but the IL side had a reduction in its’ range of motion compared to the CL side this was considered a covert abnormal response [8].
Neurodynamic treatments
Neural tensioning dysfunctions were treated with a 5-step progression starting with the CL or asymptomatic lower extremity and progressing to the IL lower extremity or symptomatic side. Tension is taken out of the IL by putting tension on the CL, followed by gradually adding tension to the IL lower extremity.
The following is an example in supine for a neural tensioning dysfunction.
- Position: CL hip flexion with knee extension. Position: IL hip and knee extension.
- Move: CL hip into flexion with knee extension. Position: IL hip and knee extension.
- Move: CL hip into flexion with knee extension. Position: add IL ankle dorsiflexion.
- Move: IL hip into flexion with knee extension. Position: add CL ankle dorsiflexion.
- Move: IL hip into flexion with knee extension. Position: CL hip and knee extension [8].
Patients that were more acute were treated with openers to take compression off the nerve root. This was accomplished by having the patient in side lying with the IL lower extremity up and the patient’s lower extremities off the side of the plinth table. The patient’s IL iliac crest was then pulled caudally towards the foot of the plinth which resulted in increased opening of the lumbar foramen on the IL or symptomatic side.8 This was often followed by tensioner progressions using the CL nerve root as seen in Figure 2.
Patients who were less symptomatic or who had covert responses to neurodynamic testing were treated with closers. Patients who did not have a reproduction of their symptoms with closing of their lumbar foramen were pushed into this barrier. This was accomplished by having the patient in side lying with the IL lower extremity down and the patient’s lower extremities off the side of the plinth table. The patient’s CL iliac crest was then pulled caudally towards the foot of the plinth which resulted in increased closing of the lumbar foramen on the IL or symptomatic side [8].
This was often followed by loading the nerve root with IL neural tensioners as seen in Figure 2.
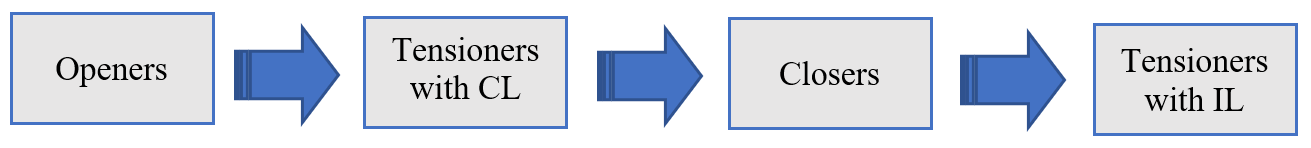
Figure 2
Patients were evaluated again post treatments to include DTRs, MMT, and neurodynamic testing. Patient treatments included, but were not limited to neural mobilization. Patient treatments often included dry needling, joint mobilization, stabilization, and/or strength training.
Results
There were 4 patients in this case series and their demographics are presented in Table 1. The patients in this case series all had a diagnosis of a lumbosacral radiculopathy. Their age range was between 44 and 62 years of age, with an average age of 53 years old. Two of the patients were male, and two were female. The left lower extremity was the affected or IL side in three patients and the right lower extremity in one. Two of the patients were seen a total of 5 visits over a span of 2-3 weeks, one patient was seen for 10 visits over a 12-week period, and one for 7 visits over a 4-week period.
Table 1: Case Series Demographics n=4.

The DTRs of the left (L) and right (R) lower extremities of both the patellar and Achilles’ tendons are shown in Table 2. The patellar tendon is innervated by the L4 nerve root and the Achilles tendon by the S1 nerve root [6]. All patients presented with a normal, or grade 2, patellar tendon reflex at initial evaluation, progress note, and discharge. Patients with an abnormal reflex presented with it to their Achilles tendons, and it was graded as a 1 or diminished. One patient who did not have a progress note presented at both the initial evaluation and discharge with normal or grade 2 DTRs. Two patients presented with a grade 1 or diminished reflex to their L Achilles tendon at the initial evaluation, but was normal or grade 2 at both the progress note and discharge. One patient presented at both the initial evaluation and progress note with a grade 1 or diminished R Achilles tendon reflex, which was normal or grade 2 at discharge.
Table 2: DTRS of the Left (L) and Right (R) Patellar (L4) and Achilles Tendons (S1).

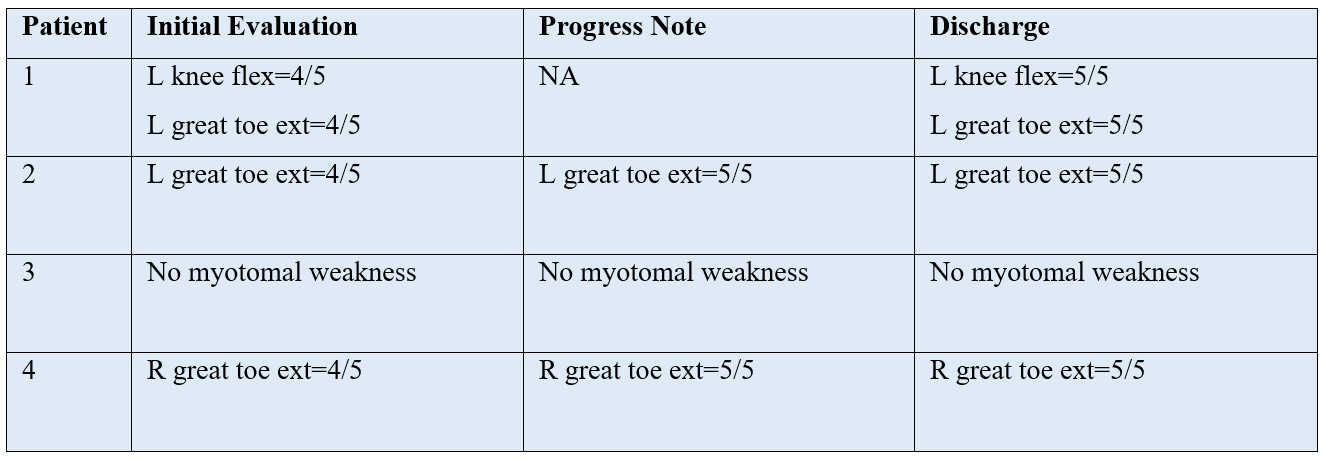
Myotomal weakness found with MMT of the bilateral lower extremities are shown in Table 3. MMT included bilateral hip flexion (L1/L2), knee extension (L3/L4), knee flexion (L5/S1), ankle dorsiflexion (L4/L5), ankle plantarflexion (S1/S2) ankle inversion (L4), ankle eversion (L5/S1), and great toe extension (L5) [9]. Any myotomal weakness found with MMT involved the L5 or S1 nerve roots. One patient did not present with any myotomal weakness at the initial evaluation, progress note, or discharge. Another patient had weakness with both L knee flexion and L great toe extension equal to 4/5 indicating involvement of both his L5 and S1 nerve roots that resolved by discharge. Two patients had weakness with great toe extension equal to 4/5 at initial evaluation that was normal or equal to 5/5 by the following progress note, and remained normal at discharge.
Table 3: Myotomal Weakness with MMT of the Bilateral Lower Extremities.
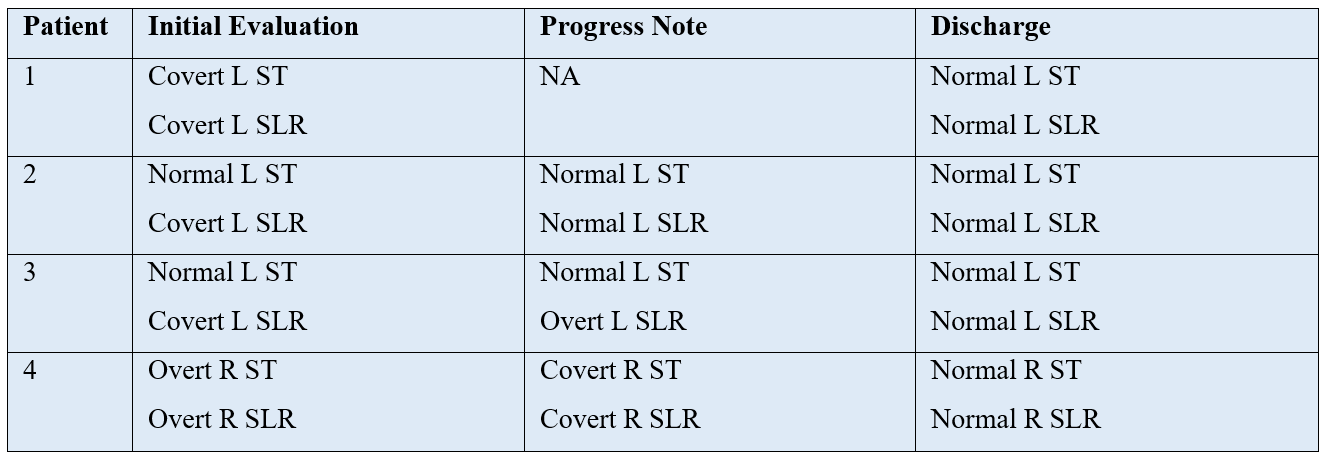
Neurodynamic responses to both the ST and SLR are shown in Table 4. Two of the patients presented with abnormal responses to the ST at the initial evaluation, one of which was covert and one overt. All four patients presented with abnormal responses to the SLR at the initial evaluation, three covert and one overt. One of the patients had both a normal ST and SLR at their progress note. One patient went from a covert to an overt response with SLR testing, and another went from overt responses with ST and SLR to covert responses. All patients had normal responses to both the ST and SLR upon their discharge.
Table 4: Neurodynamic Testing and Responses to ST and SLR.
Discussion
Four patients were assessed for DTRs, MMT, and neurodynamic responses to ST and SLR, and results indicated a normalization of all of the above. All cases who presented at the initial evaluation with diminished reflexes, myotomal weakness, or abnormal responses to neurodynamic testing were normal at discharge. These results indicate neurodynamic treatment progressions beginning with unloading a symptomatic nerve root with openers and CL neural tensioners, followed by loading a nerve root with closers and IL neural tensioners may restore normal functions of the nerve.
The changes seen in DTRs, MMT, and neurodynamic testing may be a result of the initial opening techniques of the lumbar foramen thereby taking compression off the nerve root and reducing its’ mechanosensitivity.5,10 Ongoing compression forces on a nerve root disrupt circulation to the nerve, which in turn causes impaired neural function as seen with diminished reflexes and myotomal weakness. It is for this reason that it is key that forces on a nerve are not greater than the amount the nerve can tolerate [11,12].
Forces on the nerve root can further be unloaded by taking tension off the IL nerve root by putting tension on the CL nerve root. Cadaver studies found that manual tension to the L5 nerve root resulted in a loosening of the opposite nerve root. This is due to the orientation of the lumbar nerve roots in relation to the lumbar foramen and spinal cord, whereas, tension on one nerve root results in a downward movement of the spinal cord, thereby putting the opposite nerve root on slack [4].
Conversely, it is normal for a nerve root to have a certain degree of tension, therefore, gradual loading of the IL nerve root is necessary to regain normal neural mechanics. Neural mobilization where gradual tension is added to IL nerve root intermittently may not only reduce the patient’s subjective complaints of pain, but may restore the normal physiology and mechanical function of the nerve.
Limitations
This case series is limited in its small sample size and lack of quantitative data to include but not limited to lumbar range of motion, SLR measurements, and outcome measures. Measurements of DTRs, MMT, and neurodynamic testing including ST and SLR were performed manually vs by goniometer, dynamometer, or software.
Conclusions
This case series may help physical therapists make clinical decisions in regards to neural mobilization progressions. The concept of unloading and reducing compressive forces on the nerve root is not new, but standardization for progressions of treatment has not been established. Use of CL neural tensioners to reduce tension on the IL or symptomatic nerve root is comfortable for the patient and may increase compliance for treatment. Loading of a nerve root through compression and IL neural tensioning is implemented when the patient does not have a reproduction of their symptoms, and helps restore normal neural function. Further studies are necessary to determine effectiveness in live subjects.
References
- National Guideline C. National Institute for Health and Care Excellence: Guidelines. Low Back Pain and Sciatica in Over 16s: Assessment and Management. National Institute for Health and Care Excellence (NICE) Copyright © NICE, 2016; 2016.
- Wong JJ, Côté P, Sutton DA, et al. Clinical practice guidelines for the noninvasive management of low back pain: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur J Pain, 2017; 21(2): 201-216. doi:10.1002/ejp.931.
- Ellis RF, Hing WA. Neural mobilization: a systematic review of randomized controlled trials with an analysis of therapeutic efficacy. J Man Manip Ther, 2008; 16(1): 8-22. doi:10.1179/106698108790818594
- Shacklock M, Yee B, Van Hoof T, et al. Slump Test: Effect of Contralateral Knee Extension on Response Sensations in Asymptomatic Subjects and Cadaver Study. Spine (Phila Pa 1976), 2016; 41(4): E205-E210. doi:10.1097/brs.0000000000001218
- Shacklock M. Clinical Neurodynamics: A New System of Musculoskeletal Treatment. . Edinburgh: Elsevier Butterworth Heinemann, 2005: 3.
- Rodriguez-Beato FY, De Jesus O. Physiology, Deep Tendon Reflexes. StatPearls. StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC; 2022.
- Naqvi U, Sherman AL. Muscle Strength Grading. StatPearls. StatPearls Publishing, Copyright © 2022, StatPearls Publishing LLC, 2022.
- Shacklock M. Neurodynamic Solutions Lower Quarter 1 Course. Denver, Colorado, United States, 2008.
- Keim HA, Kirkaldy-Willis WH. Low Back Pain (Clinical Symposia). 1st ed. vol 32. Ciba Pharmaceutical Co, 1980: 1.
- Elvey RL. Treatment of arm pain associated with abnormal brachial plexus tension. Aust J Physiother. 1986; 32(4): 225-230. doi:10.1016/s0004-9514(14)60655-3
- Efstathiou MA, Stefanakis M, Savva C, Giakas G. Effectiveness of neural mobilization in patients with spinal radiculopathy: a critical review. J Bodyw Mov Ther, 2015; 19(2): 205-212. doi:10.1016/j.jbmt.2014.08.006
- Topp KS, Boyd BS. Structure and biomechanics of peripheral nerves: nerve responses to physical stresses and implications for physical therapist practice. Phys Ther, 2006; 86(1): 92-109. doi:10.1093/ptj/86.1.92

