Electroconvulsive Therapy: Safety and Efficacy in the Treatment of Neuropsychiatric Disorders in Epilepsy
Mondragon Ariadna1,*, Arellano Josue1, Janssen Reinhard1, Colin P Ricardo1, Crail-Melendez Daniel1, Galíndez - Juan Pablo1, Ruiz-Chow Angel1,2,3
1Department of Psychiatry, National Institute of Neurology and Neurosurgery “Manuel Velasco Suarez”, México
2Centro Médico ABC Vasco de Quiroga 154, Contadero, Cuajimalpa de Morelos, 05348 Ciudad de Mexico
3Insurgentes sur 3877, Colonia La Fama, Alcaldía Tlalpan, Code Zip, 14269, Ciudad de México, Mexico
Received Date: 11/05/2023; Published Date: 30/08/2023
*Corresponding author: Mondragon Ariadna, Department of Psychiatry, National Institute of Neurology and Neurosurgery “Manuel Velasco Suarez”, Mexico
Abstract
Objective: The present study aims to report the use, clinical characteristics of patients who received Electroconvulsive Therapy (ECT) who were hospitalized in the department of psychiatry to optimize treatment, resulting in the indication to use ECT.
Methods: We retrospectively analyzed files from 2011 to 2019, all treated with ECT with diagnosis of Epilepsy and psychiatric comorbidity that merits electroconvulsive therapy and were hospitalized in the neuropsychiatry area from January 2011 to December 2019.
Results: We included 33 patients. The most frequent admission diagnoses were major depressive disorder (MDD) 42.4% and psychosis 30.0%; the most frequent psychiatric disorders were: psychosis 66.7%, depression 54.5%, delusions 51.5%, hallucinations 51.5%, aggression 48.5%, suicidal behavior or ideation 33.3% and anxiety 24.2%.
Conclusions: We consider that ECT treatment could be recommended in patients with epilepsy and neuropsychiatric symptoms, since all patients benefited in the resolution of affective and psychotic symptoms and there was also an increase in the MMSE score.
Key words: Epilepsy; ECT; Psychosis; MDD; Bipolar Disorder
Introduction
Epilepsy affects 50 million people worldwide; epidemiologic studies have shown that 1 in 3 people with epilepsy have a lifetime diagnosis of any psychiatric disorder, and 1 in 4 patients have a current psychiatric problem [1].
In addition to the independent association between epilepsy and neuropsychiatric disorders, many ASMs cause psychiatric adverse effects, including depression, anxiety, irritability, and more rarely suicidality, aggressive behavior, and psychosis. In large open-label studies, 15% to 20% of all PWE taking ASMs experience psychiatric side effects and 7% to 14% find these adverse effects intolerable [3,4].
Neuropsychiatric disorders should be treated in the same way as epilepsy, with specific treatments, mainly so we choose psychotropic drugs that do not lower the seizure threshold, likewise once detected alterations in cognitive function we will try to use Antiepileptic drugs (AEDs) that do not decrease the functioning of attention, memory and speed of cognitive processes.
Initiated treatment with psychotropic drugs at the appropriate doses for the appropriate time, a group of approximately 30% of patients who initiated the drugs will not respond adequately and will go on to severe mental disorder.
Electroconvulsive therapy (ECT) is effective in treating refractory mood disorders (including major depressive disorder, bipolar depression, and mania), and refractory psychosis (including schizophrenia, schizoaffective disorder, and organic psychosis); also, has been used in case series as a treatment for psychiatric disorders in patients with epilepsy.
According to studies, ECT has shown an anticonvulsant effect, based on the observation of the need for increased doses of electrical stimulus throughout each session of ECT [1,2], regardless of the mental disorder that is undergoing treatment, in reports of its use in epilepsy this has not been the exception, there are also reports aimed at using ECT as an adjunct to FAES in refractory epilepsy and status epilepticus [3-5].
During the ictal phase of the seizure induced by ECT there is an increase in blood pressure as a result of which the blood-brain barrier permeability may be facilitated, during this process certain neurochemicals increase in the circulation to the brain parenchyma bringing specific changes such as increase in brain-derived neurotrophic factor, angiogenesis and neurogenesis [6]. ECT causes neuroplastic changes in synapses (synaptogenesis), neurons (neurogenesis), dendrites (dendrogenesis), vascular (angiogenesis) as well as glial cells (gliogenesis) appearing as soon as after a single stimulus [7], positron emission tomography studies have observed increased metabolic rate producing a state of hypermetabolism [8]. Electroencephalographic (EEG) events have also been studied as a measure of brain changes and post ictal bioelectrical suppression associated with clinical response to ECT; the degree of post ictal suppression, or decrease in EEG amplitude, as well as the development of slow wave (delta) frequencies over the prefrontal cortex during and after the course of ECT, both suggest reductions in neuronal activity that have been associated with clinical improvement independent of specific technical aspects of treatment, including electrode placement and stimulus intensity [9,10].
The present study aims to report the use, clinical characteristics of patients who received ECT in a national neurological referral center in Mexico who have the diagnosis of epilepsy with psychiatric comorbidities who were hospitalized in the neuropsychiatric unit to optimize treatment, resulting in the indication to use ECT.
Materials and Methods
We carry out a Descriptive, Retrospective, case series study which files were analyzed from 2011 to 2019, all treated with ECT in the Department of psychiatry of the Instituto Nacional de Neurología y Neurocirugía "Manuel Velasco Suarez" México (INNN) This hospital has a specialized area in neuropsychiatric cases, for this study patients were selected according to the following inclusion criteria; Age: 18 to 65 years, Diagnosis of Epilepsy, who is a patient of INNN, Psychiatric comorbidity that merits electroconvulsive therapy (according to diagnostic criteria of DSM IV and 5) and who were hospitalized in the neuropsychiatry area from January 2011 to December 2019, the exclusion criteria were; Patients in which there is doubt of the diagnosis of epilepsy and patients in which all the information in the clinical record is not found. All patients were treated with the Thymatron System IV ECT machine from Somatics, Inc.©. All patients received ECT using the anesthetic procedure with thiopental and succinylcholine provided by a neuroanesthesiologist. At the time of initiation of ECT, patients had signed informed consent to receive the treatment. The data collected in the file are the following: age, sex, marital status, DEIH, year and month in which the patient was hospitalized, admission diagnosis and discharge diagnosis, type of epilepsy, age of onset of epilepsy, laterality of the epileptic focus, type of seizure (focal or generalized), seizure frequency, associated psychiatric comorbidity, treatment (antiepileptic, antipsychotic, antidepressant, anxiolytic), number of ECT sessions received, percentage of stimulation, CGI at the beginning of hospitalization and at the end, the duration of the sessions were monitored according to the electroencephalographic and electromyographic recordings. In the present study the main outcome measure consisted of the patients' subjective change in clinical symptoms throughout the ECT treatment (psychosis, depression, suicidal ideation, CGI at onset and termination), the approval of the study was obtained through the ethics committee of the INNN.
Summary measures of clinical characteristics and indications for ECT use were calculated for sessions 1, 4, 6 and 9. Percentages on the CGI scale at baseline and at the end of ECT were described, scores were compared using Wilcoxon sign test for difference of medians. From 2011 to 2019, the registry of 33 patients with epilepsy undergoing ECT for the adjuvant treatment of neuropsychiatric symptomatology was performed at the INNN (Figure 1, 2).

Figure 1: Relationship to the dose of the stimulus and duration of the EEG, EMG recording in sessions 1, 4, 6 and 9.
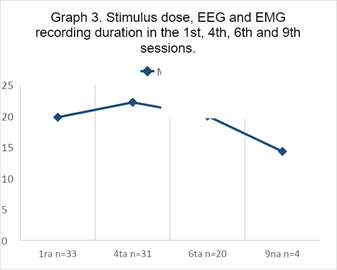
Figure 2
Results
We included 33 patients, 60.6% were women, with a mean age of 33.7±11.1 years, ranging from 18 to 52 years; 81.8% were single, 12.1% separated and 6.1% were living in a common-law relationship. The most frequent admission diagnoses were Major Depressive Disorder (MDD) 42.4% and psychosis 30.0%; the most frequent psychiatric disorders were: psychosis 66.7%, depression 54.5%, delusions 51.5%, hallucinations 51.5%, aggression 48.5%, suicidal behavior or ideation 33.3% and anxiety 24.2%.
The most common reasons for admission were consequences of MDD 39.4%, psychosis 33.3% and aggressiveness and impulsivity 18.2%. Regarding epileptic seizures, the age of onset of epilepsy was between six months of life and 42 years, with a mean of 15.4±13.8 years. Forty-eight-point five percent of seizures were generalized, 45.5% focal and 6.1% mixed. The epileptic focus was bilateral in 54.5%, right in 39.4%, left in 3% and undetermined in 3%. The 39.4% had no seizures in the last month, but 18.2% had 5 or more seizures in the same period (Table 1).
Table 1. Demographics.

Discussion
Epilepsy is now defined as a disorder of the brain characterized not only by recurrent seizures but also by its neurobiological, cognitive, and psychosocial consequences. Psychiatric disorders are associated with a high risk of side effects of antiseizure medication whereas psychiatric comorbidities have been associated with 4 times the risk of drug resistance in focal and generalized epilepsies [18]. This is the second case series published on neuropsychiatric symptoms in epilepsy treated with ECT, the Lunde & Lee series was 43 patients, this is 33 patients corresponding to the patients reviewed from 2011 to date, there are several case reports with literature review that guide the use of this neuro modulation technique with safety and efficacy. For the present study we used the psychiatric symptom severity scale (CGI) at admission to the Neuropsychiatry Unit of the National Institute of Neurology and Neurosurgery (based on symptoms to examine the patient's changes he/she had throughout ECT) (Figure 3). The social limitations, the unpredictable nature of seizures, and the potential social embarrassment associated with them can lead to poor self-esteem, social withdrawal, isolation, and distress. At the same time, several biological factors contribute to the increased occurrence of psychiatric disorders. Psychiatric symptoms were more frequent in female sex, as well as single marital status, that speaks of functional systemic dysfunction of social relationships. Mood disorders and psychosis were the most comorbid clinical conditions and were the main reasons for admission to hospitalization, as well as the main reason for giving ECT, thirdly and very important to develop neuropsychiatric symptoms in epilepsy were with a difference of 15 years being the age of onset of epilepsy with an average of 15.4 years and the age that was given ECT with a mean of 33.7 years. Finally, in this case series all patients showed improvement in neuropsychiatric symptoms due to epilepsy after one course of ECT. Evidence suggests that the neuropsychiatric manifestations of epilepsy are multifactorial, including also the use of AEDs, there are neurochemical and structural changes associated with the seizure disorder as there appear to be common pathophysiological pathways in epilepsy and psychiatric disorders [11,12]. Several studies have shown increased volume in the hippocampus, amygdala, striatum suggesting neuroplasticity following ECT [13,14], as well as increases in several hormones (prolactin, thyrotropin, oxytocin, vasopressin and glucocorticoids) [15]. ECT causes neuroplastic changes: synaptogenesis, neurogenesis, dendrogenesis, angiogenesis and gliogenesis appearing as soon as after a single stimulus [16]. If the previously reported improvements of ECT with neuropsychiatric manifestations we consider it necessary to conduct further research on the subject, in this study the decrease in neuropsychiatric symptoms could be because caused by ECT in the central nervous system previously described. It should be taken into account that, being a retrospective case series, the diagnostic criteria used were from the DSM-IV and 5, however, we focused on the scales of severity of onset and termination of ECT respectively, due to the changes already described that patient undergoing ECT present, more studies are needed in patients with epilepsy and analyze the improvements that could have in addition to the neuropsychiatric symptoms and thus reduce the use of AEDs. Although initially controversy the available evidence supports that there are pathophysiological differences between seizures from epileptogenic regions in which the irritative area usually produces an increase in neuronal death for example when we use biomarkers such as S100B and neuronal specific enolase, and on the other hand, seizures provoked with ECT there is no supported evidence that it produces neuronal death being the available evidence in the opposite direction [17], Polyakova M, Schroeter ML, Elzinga BM, et al [18], reported in a meta-analysis and systematic review that ECT increases BDNF, in animal and human models, the presence of new neurons in the hippocampal area has also been reported, although the immediate cognitive effect of ECT is a decrease in recent memory, there is evidence of long-term cognitive recovery in patients with depression, for example, as evidenced in a meta-analysis of Ong Y, Chan LG [19,20]. With these findings we consider it pertinent to initiate a prospective study of the use of ECT and epilepsy in neuropsychiatric comorbidities with the aim of observing and describing the frequency of seizures pre and post treatment with neuromodulation therapies. Also, a necessary objective to study is the possibility of reducing AEDs. We consider that ECT treatment could be recommended in patients with epilepsy and neuropsychiatric symptoms, since all patients benefited in the resolution of affective and psychotic symptoms and there was also an increase in the MMSE score, which means improvement in cognition and without presenting epilepsy complications.
ECT parameters: 94.6% of the sample completed 4 sessions of ECT, 66.8% completed at least 6 sessions. The average stimulus dose went from 131.7 mCoulombs (mC) in the first session to 232.7 mC in session 6, the Thymatron System IV equipment provides a stimulus from 0 to 100 Joules corresponding to 0 to 504 mC; the duration of the post-stimulus EEG recording from 28.7ms to 29.4ms and that of the EMG from 26.7ms to 23.5ms. The mean MMSE score went from 19.8 to 20.0, thiopental from 187.9mg to 197.7mg, and succinylcholine from 55.8mg to 57.5mg, all from the first to the sixth session (Table 2).

Figure 3: In relation to the scale distribution, initial and final Clinical Global Impression (CGI), all patients showed a decrease in at least one category of severity (p<0.001).
Table 2. Description of stimulus dose, recording duration, cognitive score, thiopental and succinylcholine dose in the 1st, 4th, 6th and 9th sessions.

The authors have no conflicts of interest or financial disclosures to report
References
- Mula M, Kanner AM, Jetté N, Sander JW. Psychiatric comorbidities in people with epilepsy. Neurol Clin Pract, 2021; 11(2): 112-120. doi:10.1212/CPJ.0000000000000874
- Perera TD, Luber B, Nobler MS, et al. Seizure expression during electroconvulsive therapy: Relationships with clinical outcome and cognitive side effects. Neuropsychopharmacology, 2004; 29: 318-325.
- Perera TD, Lisanby SH. Neurogenesis and depression. J Psychiatr Pract, 2000; 6(6): 322-333. doi:10.1097/00131746-200011000-00003
- Sackeim HA, Devanand DP, Nobler MS. Electroconvulsive therapy. In: Bloom F, Kupfer D. editors. Psychopharmacology: The fourth generation of progress. New York: Raven, 1995; p. 1123-1142.
- Nobler MS, Sackeim HA. Recent developments in electroconvulsive therapy. Psychiatr Clin North Am: Annals of Drug Therapy, 2001; 8: 1-30.
- Mirás Veiga A, Moreno DC, Menéndez AI, et al. Effectiveness of Electroconvulsive Therapy for Refractory Status Epilepticus in Febrile Infection-Related Epilepsy Syndrome. Neuropediatrics, 2017; 48(1): 45-48. doi:10.1055/s-0036-1584939
- Nobler MS, Sackeim HA. Recent developments in electroconvulsive therapy. Psychiatr Clin North Am: Annals of Drug Therapy, 2001; 8: 1-30.
- Andrade C, Bolwig TG. Electroconvulsive therapy, hypertensive surge, blood-brain barrier breach, and amnesia: exploring the evidence for a connection. J ECT, 2014; 30: 160-164.
- Weiner RD, Rogers HJ, Davidson JR, et al. Effects of stimulus parameters on cognitive side effects. Ann N Y Acad Sci, 1986; 462: 50-55.
- Perera TD, Coplan JD, Lisanby SH, et al. Antidepressant-induced neurogenesis in the hippocampus of adult nonhuman primates. J Neurosci, 2007; 27: 4894-4901.
- Nordanskog P, Dahlstrand U, Larsson MR, Larsson EM, Knutsson L, Johanson A. Increase in hippocampal volume after electroconvulsive therapy in patients with depression: a volumetric magnetic resonance imaging study. J ECT, 2010; 26(1): 62-67. doi: 10.1097/YCT.0b013e3181a95da8
- Mula M, Trimble MR, Yuen A, Liu RS, Sander JW. Psychiatric adverse events during levetiracetam therapy. Neurology, 2003; 61: 704-706.
- Johannessen Landmark C. Antiepileptic drugs in non-epilepsy disorders: relations between mechanisms of action and clinical efficacy. CNS Drugs, 2008; 22: 27-47.
- Szabo K, Hirsch JG, Krause M, et al. Diffusion weighted MRI in the early phase after electroconvulsive therapy. Neurol Res, 2007; 29(3): 256-259. doi:10.1179/174313206X153842
- Lyden H, Espinoza RT, Pirnia T, et al. Electroconvulsive therapy mediates neuroplasticity of white matter microstructure in major depression. Transl Psychiatry, 2014; 4(4): e380. doi:10.1038/tp.2014.21
- Abrams R. Electroconvulsive therapy. third. New York: Oxford University Press, 2002.
- Andrade C, Bolwig TG. Electroconvulsive therapy, hypertensive surge, blood-brain barrier breach, and amnesia: exploring the evidence for a connection. J ECT, 2014; 30: 160-164.
- Polyakova M, Schroeter ML, Elzinga BM, et al. Brain-Derived Neurotrophic Factor and Antidepressive Effect of Electroconvulsive Therapy: Systematic Review and Meta-Analyses of the Preclinical and Clinical Literature. PLoS One, 2015; 10(11): e0141564. doi: 10.1371/journal.pone.0141564
- Ong Y, Chan LG. A Systematic Review on Cognitive Effects of Electroconvulsive Therapy in Asian Patients. Clin Psychopharmacol Neurosci, 2022; 20(1): 1-16. doi:10.9758/cpn.2022.20.1.1
- Mula M, Coleman H, Wilson SJ. Neuropsychiatric and Cognitive Comorbidities in Epilepsy. Continuum (Minneap Minn), 2022; 28(2): 457-482.

