Cardiac Manifestations After Acute Viral Gastroenteritis
May Thu Kyaw*
Heart and Vascular Center, Victoria hospital, Myanmar
Received Date: 28/02/2023; Published Date: 11/05/2023
*Corresponding author: May Thu Kyaw, Heart and Vascular Center, Victoria hospital, Yangon, Myanmar
Abstract
We describe a prospective case series of six patients who had different ECG patterns and features of heart failure after acute gastroenteritis. All of them initially presented with acute gastroenteritis. All have normal serum potassium levels. Examination of stool showed no pathogens, thus viral gastroenteritis-associated myocarditis was a presumed diagnosis. Resolution of ECG changes and improvement in left ventricular systolic function were observed after 3 months follow-up. This case series express the temporal relationship between the recent gastroenteritis and acute onset of cardiac symptoms in previously well patients without significant cardiovascular risks.
Keywords: Acute viral gastroenteritis; ECG; Myocarditis; Heart failure
Introduction
Acute viral Gastroenteritis is common in clinical practice and it is usually a self-limiting condition. The etiologies of acute gastroenteritis are infectious (viral, bacterial), drugs, and toxins. Enteroviruses can cause myocarditis by direct viral invasion or immune-mediated response.
Case Series
Herein, we describe six patients (age range 16 – 33 years) with different cardiac manifestations (Table 1). All patients initially presented with acute gastroenteritis. Examination of stool culture and salmonella serology showed no pathogens. Recent medications and toxins exposure that can cause acute diarrhea and travel history was negative. Thus, viral gastroenteritis was a presumed diagnosis. None of these patients have cardiovascular risk factors like hypertension, diabetes mellitus, dyslipidemia, age, smoking, alcohol, or illicit drug use. In all cases, there was no family history of cardiomyopathies, arrhythmia, and sudden cardiac death. All have normal serum electrolytes level including potassium thus ECG changes secondary to hypokalemia were excluded. In these cases, we suspect ECG changes and cardiac manifestations may be due to gastroenteritis-associated myocarditis which may be either obvious or subclinical.
Table 1: Clinical features and investigation results in patients with acute viral myocarditis.

Patient 1
A 33-year-old man complained of central constricting chest pain. ECG showed incomplete RBBB with ST depression and T inversion in V3-V6 (Figure 1). Troponin T was 915 pg/ml. Echocardiogram showed LVEF 74% with no features of LV hypertrophy. His symptoms, ECG features, and high troponins raised the high clinical suspicion of acute coronary syndrome with anterolateral subendocardial ischemia. However, a coronary angiogram showed normal major coronary arteries without flow limitation and myocardial bridging.

Figure 1: ECG showed incomplete RBBB with ST depression and T inversion in V3-V6.
Patient 2
A 27-year-old man presented with dyspnea on exertion. ECG showed marked sinus bradycardia with a heart rate of 40 beats per minute (Figure 2). Echocardiogram showed LVEF 45% with global hypokinesia with dilated IVC 2.4cm. Despite marked sinus bradycardia, he was clinically stable with blood pressure of 110/70mmHg and oxygen saturation 98% on air, without features of hemodynamic compromise. Therefore, he was kept under close cardiac monitoring and his heart rate began to increase gradually. He recovered well without chronotropic support (pharmacological or temporary pacing). On 3rd day of admission, his ECG showed normal sinus rhythm with a rate of 72 beats per minute.

Figure 2: ECG showed marked sinus bradycardia with a heart rate of 40 beats per minute.
Patient 3
A 22-year-old man noticed chest discomfort, palpitation, and dyspnea on exertion after gastroenteritis. ECG showed sinus tachycardia with non-specific ST/T changes (Figure 3). Troponin T was 16.39 pg/ml and NT pro-BNP was 8965 pg/mL. Echocardiogram showed severely reduced LVEF 21% with dilated LA and LV with global hypokinesia with septal akinesia. He recovered dramatically with anti-heart failure medications and was discharged on the 7th day. At that time, his LVEF was 42%.
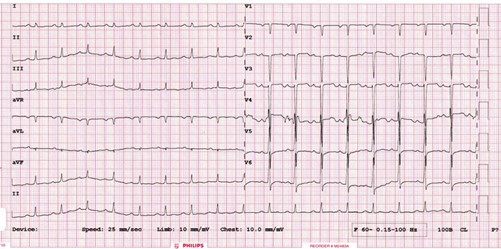
Figure 3: ECG showed sinus tachycardia with non-specific ST/T changes.
Patient 4
A 16-year-old boy complained of central chest pain, palpitation, and dyspnea on exertion, and his ECG showed diffuse ST elevation with upward concavity without reciprocal ST/T changes (Figure 4). Troponin T was 1573 pg/ml. Echocardiography showed LVEF 45% with dilated left ventricle. He was managed with a presumed diagnosis of post-gastroenteritis peri-myocarditis and respond well to medical treatment.

Figure 4: ECG showed diffuse ST elevation with upward concavity without reciprocal ST/T changes.
Patient 5
A 27-year-old lady presented with dyspnea and palpitation. Her ECG showed atrial fibrillation with a rapid ventricular response (rate 155 bpm) (Figure 5). Troponin T was 17.21 pg/ml and NT pro-BNP was 6248 pg/ml. LVEF was 50%. Pharmacological cardioversion was done with intravenous amiodarone, her ECG returned to normal sinus rhythm.

Figure 5: ECG showed atrial fibrillation with a rapid ventricular response.
Patient 6
An ECG was done on a 25-year-old lady after a one-day history of gastroenteritis, which showed a significant prolonged QT interval. (QTc 511 ms) (Figure 6). Unfortunately, there was no prior ECG to compare. There was no history of palpitation, syncope, or family history of sudden cardiac death. Serum electrolytes (corrected calcium, magnesium, and potassium levels) were within normal range. She was not on any medications that can prolong QT interval. She was discharged on the 5th day of admission. At that time, her ECG showed normal sinus rhythm with a heart rate 65 beats per minute and QTc 410ms.
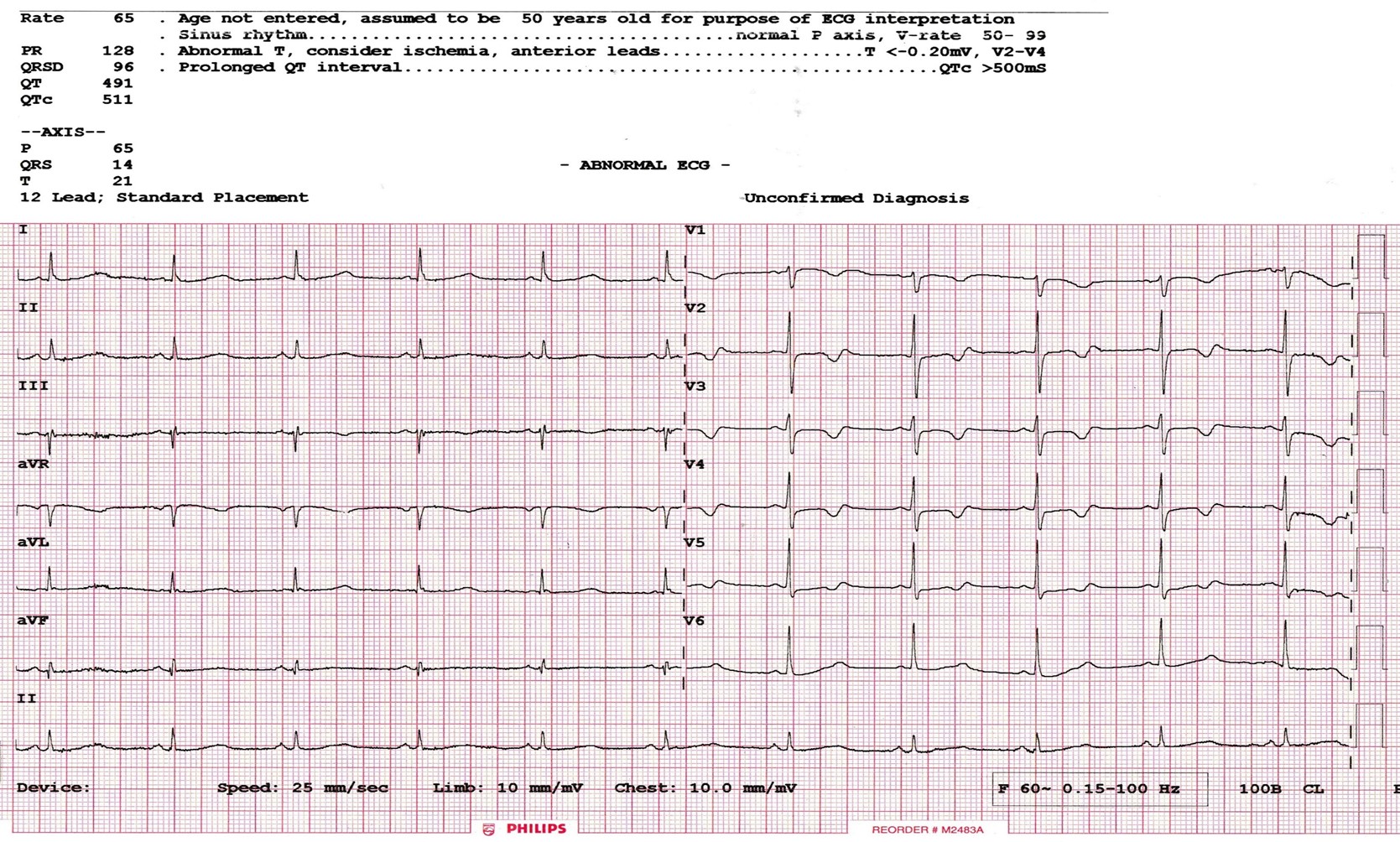
Figure 6: ECG showed a significant prolonged QT interval. (QTc 511 ms).
All patients were treated with rehydration therapy (oral and intravenous) with monitoring fluid balance. Antibiotics, antidiarrheal and anti-emetics agents were used in none of these patients due to the self-limiting nature of gastroenteritis and medication-induced arrhythmogenic potential. Patients presenting with heart failure (case 2,3,4,5) were managed with anti-heart failure therapy (ACEI angiotensin-converting enzyme inhibitors, diuretics, beta-blockers). None of these patients required circulatory support (either pharmacological or mechanical). Presenting with chest pain, high cardiac isoenzymes (troponins), and ST segment changes, co-existence myocardial ischemia (may be MINOCA, myocardial infarction with non-obstructed coronary arteries) cannot be excluded and thus, anti-coagulations were added to case 1 and case 4. After 3 months and 6 months follow-up, all patients showed resolution of ECG abnormalities and improvement in left ventricular ejection fraction.
Discussion
Acute gastroenteritis is one of the most common infectious diseases worldwide. Its incidence is underestimated because not everyone with acute gastroenteritis seeks medical attention due to its self-limiting nature. Viruses (rotavirus, norovirus, enteroviruses) account for most cases of acute gastroenteritis. The other causes are bacteria (1-6%), medications, and toxins [1]. It usually presents with nausea, vomiting, watery diarrhea, abdominal pain, and fever, and usually resolves within 1 to 2 weeks.
Viral gastroenteritis can be associated with viral myocarditis. Direct invasion and replication of the virus itself and subsequent activation of immune response cause cytokines release, which results in myocyte inflammation and necrosis [2]. Cardiac electrical instability due to myocyte death, Viral-related ion channel impairment, and abnormal automaticity are supposed mechanisms for arrhythmogenicity in acute viral myocarditis [3]. Clinical features of acute myocarditis are variable: mild asymptomatic, chest pain mimicking myocardial infarction, palpitation due to brady-tachy arrhythmia, dyspnea, and in most severe forms, can present with life-threatening arrhythmia, acute heart failure, and sudden cardiac death [4].
The standard 12-lead ECG is the initial investigation although its sensitivity is low (47%) [5]. Sinus tachycardia with non-specific ST-T wave changes is the most common ECG finding. Conduction system disturbance can lead to various forms of brady-tachy arrhythmia. The most common bradyarrhythmias in acute myocarditis are sinus arrest, sick sinus syndrome, and AV blocks [6]. Apart from sinus tachycardia, acute myocarditis can also present with atrial fibrillation, atrial flutter, supraventricular tachycardia, and ventricular fibrillation [7]. ST segment changes, either elevation or depression can also be seen in ACS-like myocarditis [4].
Measurement of cardiac enzymes and biomarkers (Troponins and NT-proBNP) can also be used as indirect evidence of myocyte damage. Echocardiography is a valuable non-invasive imaging test and it can detect left ventricular systolic dysfunction, wall motion abnormalities, and chamber dilatation. Other advanced investigations include cardiac MRI (CMR), cardiac CT, and endomyocardial biopsy (EMB). Late gadolinium enhancement at CMR is a diagnosis of acute myocarditis and is associated with poor prognosis [8].
Management mainly depends on presenting symptoms. Acute myocarditis has a good prognosis with spontaneous recovery seen in about 50%. ACEI or angiotensin-receptor blockers (ARBs), β-blockers, diuretics, and aldosterone antagonists are first-line medications for heart failure treatment. Circulatory support (either inotropic agents or mechanical) may be required in fulminant myocarditis. Bradyarrhythmia needs close cardiac monitoring because it can progress to high-grade atrioventricular block, sinus arrest, and asystole. Temporary pacing may be a consideration. Pharmacological or mechanical cardioversion should be considered in patients with atrial or ventricular fibrillation with hemodynamic compromise. Anticoagulation may be needed and beneficial if there is a risk of arterial and venous thromboembolism associated with atrial fibrillation or concomitant myocardial ischemia cannot be excluded [9]. Long-term antiarrhythmic medications, implantable cardioverter defibrillators (ICD), or permanent pacemaker insertion may be warranted if tachy or brady arrhythmia persists after acute illness subsides. The role of anti-viral is unclear. Immunosuppressive therapy, immunomodulatory therapies like high-dose intravenous immunoglobulin, and immunoadsorption (IA) may be used in special cases. All patients with acute myocarditis should limit physical activity for at least 6months [10]. Regular ECG and echocardiographic monitoring are essential for the early detection of complications due to chronic myocarditis.
Conclusion
Timely diagnosis and prompt treatment is crucial in acute myocarditis to prevent life-threatening complications and chronic myocarditis. Myocarditis should be an important differential diagnosis if a person without significant cardiac risk factors presents with acute de novo heart failure and new-onset tachy-brady arrhythmia. Prior history of acute viral illness supports the diagnosis. Thus, clinicians should be aware of these potentially life-threatening cardiac complications when treating patients with acute viral gastroenteritis.
Limitation
There are some limitations in this case series. Diagnosis of myocarditis was done mainly based on clinical symptoms, cardiac biomarkers (Troponins and NT pro-BNP), echocardiogram, and history of viral gastroenteritis. Due to limited resources, endomyocardial biopsy (EMB) and CMR have not been done. In case 6, genetic testing for congenital long QT syndrome has not been done. However, due to negative family history, exclusion of secondary causes (medications and electrolyte imbalance), and resolution of prolonged QT interval, we supposed that long QT interval may be related to myocardial conduction disturbances associated with transient viral myocarditis.
Acknowledgment: None
Funding information: No funding was obtained for this study.
Conflict of interest: The author declares that there is no conflict of interest.
Data availability statement: All data supporting the conclusions are presented in the manuscript.
Ethical approval: Not applicable.
Consent: Written informed consent was obtained from the patients and patient’s guardian to publish this case series and any accompanying images.
References
- Graves NS. Acute gastroenteritis. Prim Care, 2013; 40(3): 727-741. doi: 10.1016/j.pop.2013.05.006. Epub 2013 Jul 19. PMID: 23958366; PMCID: PMC7119329.
- Maisch B, Ristić AD, Hufnagel G, Pankuweit S. Pathophysiology of viral myocarditis: the role of humoral immune response. Cardiovasc Pathol, 2002; 11(2): 112-122. doi: 10.1016/s1054-8807(01)00113-2. PMID: 11934603.
- Sozzi FB, Gherbesi E, Faggiano A, Gnan E, Maruccio A, Schiavone M, et al. Viral Myocarditis: Classification, Diagnosis, and Clinical Implications. Front Cardiovasc Med, 2022; 9: 908663. doi: 10.3389/fcvm.2022.908663. PMID: 35795363; PMCID: PMC9250986.
- Buttà C, Zappia L, Laterra G, Roberto M. Diagnostic and prognostic role of electrocardiogram in acute myocarditis: A comprehensive review. Ann Noninvasive Electrocardiol, 2020; 25(3): e12726. doi: 10.1111/anec.12726. Epub 2019 Nov 28. PMID: 31778001; PMCID: PMC7958927.
- Shauer A, Gotsman I, Keren A, Zwas DR, Hellman Y, Durst R, et al. Acute viral myocarditis: current concepts in diagnosis and treatment. Isr Med Assoc J, 2013; 15(3): 180-155. PMID: 23662385.
- Inoue S, Shinohara F, Sakai T, Niitani H, Saito T, Hiromoto J, et al. Myocarditis and arrhythmia: a clinico-pathological study of conduction system based on serial section in 65 cases. Jpn Circ J, 1989; 53(1): 49-57. doi: 10.1253/jcj.53.49. PMID: 2716170.
- Gkouziouta A, Karavolias G, Kourkoveli P, Fekos J, Katsianis A, PH Cokkinos S. et al. Incidence and characteristics of tachyarrhythmias in patients with acute myocarditis, European Heart Journal, 2013; 34(suppl_1): 1. P3871, https://doi.org/10.1093/eurheartj/eht309.P3871
- Baccouche H, Mahrholdt H, Meinhardt G, Merher R, Voehringer M, Hill S, et al. Diagnostic synergy of non-invasive cardiovascular magnetic resonance and invasive endomyocardial biopsy in troponin-positive patients without coronary artery disease. Eur Heart J, 2009; 30(23): 2869-2879. doi: 10.1093/eurheartj/ehp328. Epub 2009 Aug 20. PMID: 19696191.
- Schultz JC, Hilliard AA, Cooper LT Jr, Rihal CS. Diagnosis and treatment of viral myocarditis. Mayo Clin Proc, 2009; 84(11): 1001-1009. doi: 10.1016/S0025-6196(11)60670-8. PMID: 19880690; PMCID: PMC2770911.
- Pollack A, Kontorovich A, Fuster V, et al.Viral myocarditis—diagnosis, treatment options, and current controversies. Nat Rev Cardiol,2015; 12: 670–680. https://doi.org/10.1038/nrcardio.2015.108.

