The Adoption of Narrow-Band Imaging for Colorectal Polyps in Malaysia, Are We Ready for Prime-Time?
Narayanan Prakash*, Cha Chee Tan, Shih Mun Yong, Keng Hoong Chiam and Muthukaruppan Raman
Department of Medicine, Queen Elizabeth Hospital, Kota Kinabalu Sabah, Malaysia
Received Date: 27/02/2023; Published Date: 08/05/2023
*Corresponding author: Narayanan Prakash, Department of Medicine, Queen Elizabeth Hospital, Kota Kinabalu Sabah, Malaysia
Background
Objective: To evaluate the sensitivity and Negative Predictive Value (NPV) of real-time optical diagnosis with colorectal Narrow-Band Imaging (NBI) in addition to exploring its’ feasibility for prime-time application in Malaysia.
Design: Retrospective analysis of prospectively collected data.
Setting: Single centre, tertiary referral hospital.
Patients: Individuals requiring colonoscopies for various indications were analysed.
Intervention: Colorectal polyps measuring less than 10 mm were detected on White Light Imaging (WLI) followed by characterization with NBI, resulting in a real-time optical histological diagnosis prior to resection. The NBI interpretation was then compared against formal histopathology reporting for a conclusive diagnosis.
Main outcome measurement: All resected specimens were examined by our resident pathologists and identified as either adenoma or non-adenoma.
Results: A total of 600 colorectal lesions sized ‹10mm from 264 patients were reported in this study. The mean age was 59.0±9.98 years. The mean size of the lesions was 4.61±2.28mm; 404 (67.3%) lesions were diminutive (≤5mm) and 196 (32.7%) were small (>5 mm and ‹10mm). The relationship between NICE classifications and histologic findings are demonstrated in table 2. The sensitivity, specificity, PPV, NPV and accuracy based on the NICE classification was 97.54%, 93.99%, 96.97% and 96.36% respectively.
Conclusion: In an established centre with modern endoscopy setup, the adoption of colorectal NBI for the resect-and-discard and diagnose-and-leave strategy is a conceivable approach. Histological evaluation can be limited to lesions with low-confidence optical diagnosis which in turn reduces the burden on overall hospital expenditure and human resources.
Introduction
Colorectal Cancer (CRC) is the third most diagnosed malignancy worldwide. It ranks second for global cancer-related mortality [1]. Colonoscopy and polypectomy are the only method proven to halt the progression of the adenoma-carcinoma sequence. This sequence is recognized as the natural evolution of an adenomatous lesion into cancer [2]. More than 90% of colorectal polyps encountered are small, measuring less than 10 mm in size [3,4]. These are easily removed and sent for histological evaluation to guide subsequent surveillance colonoscopy. Despite this, not all polyps are adenomatous and thus need not be removed. A proportion of them are hyperplastic lesions located in the sigmoid colon and rectum that do not progress with time [5]. Resection can be time-consuming when they are flat and occur in multiplicity.
The role of colorectal polyp characterization with Narrow-Band Imaging (NBI) has significantly altered the landscape for endoscopic polypectomy. This paradigm shift grants the endoscopist the ability to interpret the polyp real-time and guides decision making on whether to adopt the ‘resect-and-discard’ or ‘diagnose-and-leave’ strategy during colonoscopy [6,7]. When applied in colorectal cancer screening, this would translate to a huge cost-saving effort in addition to reducing the workload for the pathologist.
Colorectal cancer screening in Malaysia is primarily opportunistic and is driven by healthcare providers’ awareness on the availability of stool-based test and referral to a centre with colonoscopy. The implementation would likely be a huge challenge owing to cost and if we could drive down a huge financial portion in diagnostic expenses, the likelihood of embracing screening policies could be a reality.
Methodology
Study Type and Design
This is a retrospective analysis of prospectively collected data of small colorectal polyps (less than 10 mm) found in patients during colonoscopy for various indications in a tertiary centre in Sabah. The duration of the study was from February 2020 to February 2022.
Study Population
Individuals requiring colonoscopies for common indications were analysed. Colorectal polyps measuring less than 10 mm were systematically characterised with NBI. These polyps were then resected and histological evaluation obtained. Colonoscopies without polyps or those with polyps that are 10 mm or larger were excluded from our study.
Inclusion Criteria
- All patients presenting for colonoscopies with colorectal polyp measuring less than 10 mm.
Exclusion Criteria
- Patients with colorectal polyps measuring 10 mm or larger.
Sample Size
Until the completion of the study duration
Endoscopic procedure
Under conscious sedation, WLI and NBI colonoscopic observations were performed for detected colorectal polyps by an expert endoscopist trained in advance endoscopic imaging. WLI was first used to detect polyps followed by characterisation with the NBI mode. High magnification is available and can be used on demand. All colonoscopies were performed with the attachment of an Olympus distal transparent cap to achieve an optimal crisp and clear image. The WLI and NBI polyp images were photo-documented and stored followed by polypectomy.
Endoscopic system:
The Olympus colonoscopes in which both WLI and NBI function were used in this study was the EVIS EXERA III CF H190L, CF HQ190L and PCF H190L. The colonoscopes were connected to a CV-190 video processor system and fitted with the CLV-190 Xenon Light Source.
WLI diagnostic criteria:
All colonic polyps were first detected using the WLI setting with their location, size and gross morphology identified and computed by an assistant.
NBI diagnostic criteria:
Polyps detected on WLI were then characterised further using the capillary pattern classification developed by NICE. Based on the NICE classification, non-adenomatous lesions were identified as NICE 1. Adenomatous lesions were identified as NICE 2.
Histopathology
All resected polyp specimens were examined by our general pathologists. In the study, a colorectal polyp was identified either as an adenoma or non-adenoma.
Data collection
The variables collected in the study include: Patient’s age at colonoscopy, gender, indication for colonoscopy, depth of colonoscopy insertion, bowel preparation based on Boston Bowel Preparation Score (BBPS), lesion size, location, Paris classification of morphology, NBI capillary pattern based on JNET classification, NBI diagnosis, histological diagnosis, method of resection and completeness in resection.
Statistical analysis
The variables were analysed with IBM’s Statistical Package for Social Sciences (SPSS 25.0 Package Facility, SPSS Inc., Chicago, Illinois, USA). Colonic polyps were evaluated when a diagnosis for neoplasm and non-neoplasm were made. When a diagnosis was classified as non-interpretable, they were excluded from the diagnostic test evaluation. The diagnostic test evaluation consisted of sensitivity, specificity, positive, negative predictive values and accuracy.
Risk and benefit to study participants: Not applicable
Risk Benefit Assessment: Not applicable
Ethics of Study: The study will be conducted in compliance with ethical principles outlined in the Declaration of Helsinki and Malaysian Good Clinical Practice Guideline. The investigators also seek study approval from local ethical committee (Malaysia Research Ethics Committee) prior to starting this study.
Informed Consent: As per local hospital guideline. Informed consent will be taken with the usual consent form furnished by the endoscopy unit in addition to a separate research consent form. Patients will be given adequate time to read, ask questions and decide on their participation in the study.
Privacy and Confidentiality
Subject’s names will be kept on a password-protected database and will be linked only with a study identification number for this research. The identification number instead of patient identifiers will be used on subject data sheets. All data will be entered into a computer that is password protected. On completion of study, data in the computer will be copied to CDs and the data in the computer erased. CDs and any hardcopy data will be stored in a locked office of the investigators and maintained for a minimum of three years after the completion of the study. The CDs and data will be destroyed after that period of storage. Subjects will not be allowed to view their personal study data, as the data will be consolidated into a database. Subjects can write to the investigators to request access to study findings.
Results
Table 1: Clinicopathological characteristic of colorectal lesions less than 10 mm.
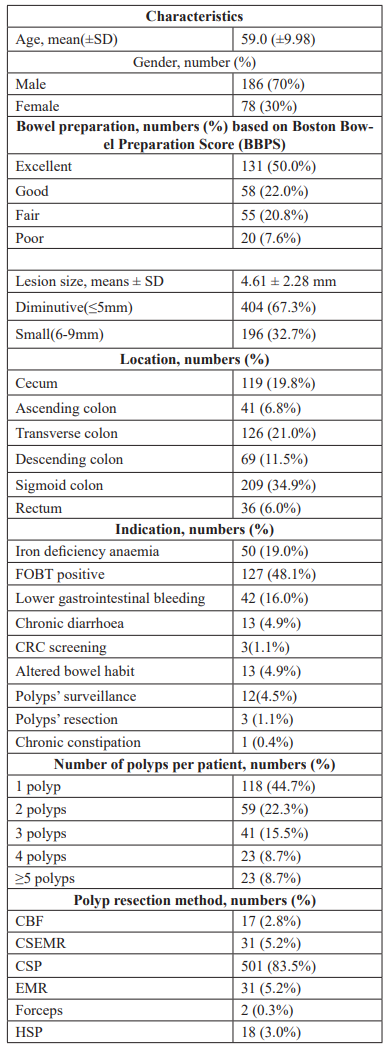
CBF: Cold biopsy forceps; CSEMR: Cold snare endoscopic mucosal resection; CSP: Cold snare polypectomy; EMR: Endoscopic mucosal resection; HSP: Hot snare polypectomy
Table 2: Characterisation of polyps retrieved for histological determination.
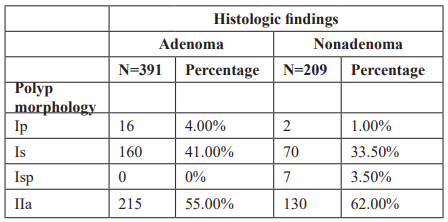
Table 3: Relationship between NBI International Colorectal Endoscopic (NICE) classification and histologic findings.
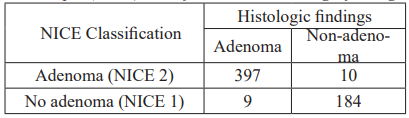
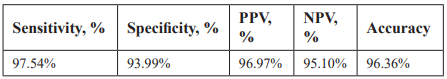
Table 4: Performance characteristics of NBI International Colorectal Endoscopic (NICE) classification.
A total of 600 colorectal lesions sized ‹10mm from 264 patients were reported in this study. The mean age was 59.0±9.98 years. The mean size of the lesions was 4.61±2.28mm; 404(67.3%) lesions were diminutive (≤5mm) and 196(32.7%) were small (‹10mm). The location of polyps; 119(19.8%) in cecum, 41(6.8%) in ascending colon, 126(21.0%) in transverse colon, 69(11.5%) in descending colon, 209(34.9%) in sigmoid colon and 36(6.0%) in rectum. These were resected using various polypectomy methods include 501 polyps via cold snare polypectomy, 31 polyps via endoscopic mucosal resection, 31 polyps via cold snare endoscopic mucosal resection, 17 polyps via cold biopsy forceps, 18 polyps via hot snare polypectomy and 2 polyps via cold biopsy forceps avulsion. The resection method was decided based on the size, location and morphology of the polyp. Attempts made to ensure completeness of resection includes endoscopic evaluation of resected base and further clarified by histological assessment.
The relationship between NICE classifications and histologic findings shows in Table 2. The sensitivity, specificity, PPV, NPV and accuracy based on NICE classification were 97.54%, 93.99%, 96.97% and 96.36% respectively.
Discussion
In this study, we obtained data regarding clinical utility of NICE classification system for the diagnosis of diminutive and small colorectal polyps by classifying 600 colorectal polyps through a review of magnifying NBI images and a comparison with pathological findings. The NBI diagnosed of NICE 1 and NICE 2 correlated strongly with non-adenoma and adenoma respectively, suggesting that lesion could be diagnosed using NICE classification alone. Our results were in accordance to the key requirements set by the ASGE PIVI on Real-Time Endoscopic Assessment of the Histology of Diminutive Colorectal Polyps thresholds [8] with a sensitivity of 97.54% and negative predictive value of 96.97%, our experience was similar with other centres [9,10].
NBI technology is easily available that has been implemented into current generation of endoscopes (Olympus Inc, Tokyo, Japan). NBI technology is an exciting frontier in advance diagnostic endoscopy for which its use has been widely adopted in various lesions found within the gastrointestinal tract. The applicability for characterization is simple to operate with a single push of a button on the endoscope following lesion detection on white light imaging.
Furthermore, there are validated and established tools such as the NBI International Colorectal Endoscopic (NICE) and Japan NBI Expert Team (JNET) classifications with sample images for convenient referencing [11]. The adoption of NBI is convenient and provides high-confidence prediction with both sensitivity and negative predictive value (NPV) exceeding 90% [12].
The most standardized agreement for lesion characterization is within the colon and rectum. Of the multiple classifications published, the NICE classification is widely regarded as the easiest to use. The three key components that NICE looks into includes the polyp colour, vessels and surface pattern. In addition, figure illustration is also provided for the convenience of comparison. This can be easily attached in endoscopy rooms for reference purposes or serve as a quick guide when clarification is required. Unlike other NBI classifications, the NICE classification can be used without the need for magnifying endoscopes. The latter is not readily available in many centres outside Japan where the majority of these classifications are developed.
There are certainly some challenges in getting this technology through to the general pool of endoscopists who are more familiar with white light imaging compared to NBI. The belief that all lesions should either be biopsied or resected is not cost-effective. Furthermore, biopsied lesions may be inconclusive and this would in turn lead to patient anxiety and fear. If NBI could assist in lesion characterization with high confidence, endoscopists may then be more comfortable with removing ‘genuine’ precancerous lesion while leaving the benign ones alone. The role of NBI could also guide targeted biopsy on a suspicious focus in bigger polyps that would allow for a better yield. This would reduce the need for multiple repeat procedures meant for diagnostic clarification and allow a clearer pathway towards definitive treatment.
The main limitation in our study is a retrospective study from single centre. A good start would be to incorporate a comparison for pre- and post-formal training on NBI colorectal polyp classification followed by assessment on their individual and collective sensitivity and NPV performance. Although this research focus has been addressed at various recognized endoscopic centres worldwide, our challenge is that a large burden of colonoscopies is performed by junior endoscopists in the public health system [13,14]. By addressing their needs with brief training exercises and refresher courses, we believe that this would enhance the capability of both polyp detection and characterization. Thus, only true ‘adenomas’ should be respected and suspicious lesions biopsied for histological confirmation.
Conclusion
In an established centre with modern endoscopy setup, the adoption of colorectal NBI for the resect-and-discard and diagnose-and-leave strategy is a conceivable approach for diminutive and small polyps. Histological evaluation can be limited to lesions with low-confidence optical diagnosis which in turn reduces the burden on overall hospital expenditure and human resources.
Conflict of Interest: The investigators declare they have no conflict of interest.
Publication Policy: No personal information will be disclosed and subjects will not be identified when the findings of the survey are published.
References
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin, 2018; 68: 394–424
- Zauber AG, van BM, Schapiro M, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med, 2012; 10.
- Lieberman D, Moravec M, Holub J, Michaels L, Eisen G. Polyp size and advanced histology in patients undergoing colonoscopy screening: implications for CT colonography. Gastroenterology, 2008; 135(4): 1100–1105.
- Rex DK, Overhiser AJ, Chen SC, Cummings OW, Ulbright TM. Estimation of impact of American College of Radiology recommendations on CT colonography reporting for resection of high-risk adenoma findings. Am J Gastroenterol, 2009; 104(1): 149–153.
- Weston AP, Campbell DR. Diminutive colonic polyps: Histopathology, spatial distribution, concomitant significant lesions, and treatment complications. Am J Gastroenterol, 1995; 90: 24–28.
- Rastogi A, Rao DS, Gupta N, Grisolano SW, Buckles DC, Sidorenko E, et al. Impact of a computer-based teaching module on characterization of diminutive colon polyps by using narrow-band imaging by nonexperts in academic and community practice: a video-based study. Gastrointest Endosc, 2014; 79: 390-398. DOI: 10.1016/j.gie.2013.07.032.
- Ladabaum U, Fioritto A, Mitani A, Desai M, Kim JP, Rex DK, et al. Real-time optical biopsy of colon polyps with narrow band imaging in community practice does not yet meet key thresholds for clinical decisions. Gastroenterology 2013; 144: 81-91. DOI: 10.1053/j.gastro.2012.09.054
- Abu Dayyeh BK, Thosani N, Konda V, et al. ASGE Technology Committee systematic review and meta-analysis assessing the ASGE PIVI thresholds for adopting real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointestinal endoscopy, 2015; 81(3): 502.e1–502.e16.
- Hassan C, Pickhardt PJ, Rex DK. A resect and discard strategy would improve cost-effectiveness of colorectal cancer screening. Clin Gastroenterol Hepatol, 2010; 8: 865-869.
- Wanders LK, East JE, Uitentuis SE, Leeflang MM, Dekker E. Diagnostic performance of narrowed spectrum endoscopy, autofluorescence imaging, and confocal laser endomicroscopy for optical diagnosis of colonic polyps: a meta-analysis. The lancet oncology, 2013; 14: 1337-1347.
- Hewett DG, Kaltenbach T, Sano Y, Tanaka S, Saunders BP, Ponchon T, et al. Validation of a simple classification system for endoscopic diagnosis of small colorectal polyps using narrow-band imaging. Gastroenterology, 2012; 143(3): 599–607.e1.
- McGill SK, Evangelou E, Ioannidis JP, Soetikno RM, Kaltenbach T. Narrow band imaging to differentiate neoplastic and non-neoplastic colorectal polyps in real time: a meta-analysis of diagnostic operating characteristics. Gut, 2013; 62: 1704-1713. DOI: 10.1136/gutjnl-2012-303965
- Rastogi A, Pondugula K, Bansal A, et al. Recognition of surface mucosal and vascular patterns of colon polyps by using narrow-band imaging: interobserver and intraobserver agreement and prediction of polyp histology. Gastrointest Endosc, 2009; 69: 716-722.
- Raghavendra M, Hewett DG, Rex DK. Differentiating adenomas from hyperplastic colorectal polyps: narrow-band imaging can be learned in 20 minutes. Gastrointest Endosc, 2010; 72: 572-576.

