Tuberculosis Outbreak Investigation in Seolwane Village, Botswana
Goabaone Rankgoane-Pono1,*, Lisani Ntoni1,2, Keatlaretse Siamisang1,2, Sidney Kololo2, Gilbert Paphidzo2, Dianah Modibedi2 and Tantamika Kabamba Mudiayi2
1Department of Family Medicine and Public Health, University of Botswana, Gaborone, Botswana 2Department of Health Services Management, Ministry of Health, Gaborone, Botswana
Received Date: 14/02/2023; Published Date: 07/04/2023
*Corresponding author: Goabaone Rankgoane-Pono, Department of Family Medicine and Public Health, University of Botswana, Gaborone, Botswana
Abstract
Introduction: Tuberculosis (TB) remains one of the world’s deadliest communicable diseases. There is an increased risk of transmission of Tuberculosis (TB) in institutional settings and overcrowded areas. Early detection, rapid diagnosis and early initiation of treatment are the cornerstone for containing the spread of infection., This is particularly important during outbreaks as it interrupts the transmission chain. Screening of contacts allows detection of
active disease and latent TB infection (LTBI) in order to initiate the right treatment.
Methods: This was an outbreak investigation of TB cases in Seolwane village, in the Maunatlala health catchment area in Palapye DHMT central district, Botswana., with a population of 1513 people an expert team was set-up in order to investigate the outbreak. The primary goal of the outbreak investigation was to control the disease within the affected population and to prevent the disease from spreading to other populations. The team responded to the outbreak using a systematic approach following the outbreak investigation steps.
Results: We report a cluster of 16 TB cases at Seolwane village. The median age was 36 years (IQR 17-50). Of the 16 patients, all were new notifications. 62.5% were males and 43.5% were HIV positive on treatment.The epidemiologic curve depicted a propagated source outbreak
Conclusion: The outbreak investigation afforded detection of cases who were probably living with the disease and transmitting it and also early identification of more patients who benefited from early management of TB, preventing further morbidity and transmission. Outbreak investigations are an important intervention in any communicable disease.
Keywords: Tuberculosis; Outbreak investigation; Botswana
Introduction
Tuberculosis (TB) remains one of the world’s deadliest communicable diseases. There is an increased risk of transmission of TB in institutional settings and overcrowded areas. TB outbreaks have been described in nursing homes, correctional facilities and boarding schools. What is common about these settings is that they encourage prolonged exposure due to congregate lodging [1-4] However, there are outbreaks occurring in the community, reinforcing the need for constant surveillance in order to detect, understand and control the outbreak earlier. It is essential to identify high-risk, hot spot settings with increased risk of TB transmission in order to reduce transmission and control the epidemic. Delayed identification of high-risk areas and delayed TB case detection, resulting in prolonged exposure can lead to TB outbreaks [5,6]. Investigating and managing TB outbreaks can be a challenging intervention for national TB programs. The characteristics of the index case has implications on how the investigation will be carried out. If the index is a child, it means there is an adult who is the primary source of the infection and the priority is finding that adult and where the index is an adult, the priority is finding other infected contacts [6].
Early detection, rapid diagnosis and early initiation of treatment are the cornerstone for containing the spread of TB. This is particularly important during outbreaks as it interrupts the transmission chain. Screening of contacts allows detection of active disease and Latent TB Infection (LTBI) in order to initiate the right treatment [6,7].
Case investigations are very similar to outbreak investigations in that in both the investigators have to look for contacts to an index case. So, the principles of contact investigations are very vital to outbreak investigations. The difference is in that the management of contacts and cases is more complex in an outbreak investigation. The overall response can be complex for national TB programs making it difficult to respond quickly and effectively to TB outbreaks.
The primary goal of any outbreak investigation is to control the disease within the affected population and to prevent the disease from spreading to other populations [1-3].
For the Botswana National TB Program (BNTP), TB Surveillance is a hierarchical reporting system, with local health facilities manually reporting to the district TB coordinator/ focal person at District Health Management Team (DHMT) using the TB registers. The TB coordinator/focal person will transfer the data into a manual district TB register and an electronic web-based data management system called Open Medical Record System (OpenMRS), which will be accessed by the national monitoring and evaluation office. When a DHMT (sub-national level management) determine that the district has exceeded the expected number of cases following previous trends for that period, warranting an outbreak investigation, they will invite the national level for technical assistance. The BNTP will arrange a team from national TB officers to visit the affected district to go establish if there is an outbreak and manage it by describing the epidemiology of the outbreak, find any missing cases, identify transmission sites, conduct contacts screening, and implement control measures.
In December 2019 the Tuberculosis (TB) focal person at the Palapye DHMT based at Maunatlala clinic noticed an unusual rise in number of TB cases in Seolwane village which he supports therefore notified the Botswana National TB program (BNTP). This prompted the Palapye DHMT to bring interventions to respond to the outbreak in December 2019 and January 2020. The BNTP supported the response and carried out the TB outbreak investigation so as to guide necessary actions required to respond.
We report a cluster of 16 TB cases that occurred in Seolwane village (with a population of 1513 people) in the Maunatlala health catchment area in Palapye DHMT. The TB cases lived in dispersed communities.
Methodology and Findings
An expert team made up of an M&E Officer, Medical officer, Active Case finding coordinator was set-up in order to investigate the outbreak. The experts were selected by the Program Manager based on their expertise in the different areas of outbreak investigations, TB control and clinical medicine. The team responded to the outbreak using a systematic approach following these steps:
- Prepare for field work
- Establish the existence of an outbreak
- Verify the diagnosis
- Construct a working case definition
- Find cases systematically and record information
- Perform descriptive epidemiology
- Develop hypotheses
- Evaluate hypotheses
- As necessary, reconsider, refine, and re-evaluate hypotheses
- Implement control and prevention measures
- Communicate findings
Preparing for field work
Preparing for fieldwork involved convening the outbreak response team and defining the
roles and expectations of each team member.
The team also had an action plan and the objectives of the TB outbreak investigation were:
To confirm existence of outbreak
To assess contact investigation process
To Ensure laboratory investigations are conducted according to
National TB Management guidelines
To assess community engagement
To Ensure there is appropriate recording and reporting
To assess the needs of the DHMT and where possible address them, to facilitate an effective response to the TB outbreak
To assess the implementation of certain TB interventions (Active Case Finding, Intensified Case Finding, Community TB Care, Case management)
Establish the existence of an outbreak
We assessed the 5-year trend of TB cases at Seolwane village from 2015 to 2019. Before 2019, we noted the maximum number of cases had been 5. In 2019, Seolwane recorded 16 cases. Half (8 out of the 16 cases) were recorded in December 2019. Contact tracing was done in all 8 reported cases and 3 secondary cases diagnosed.
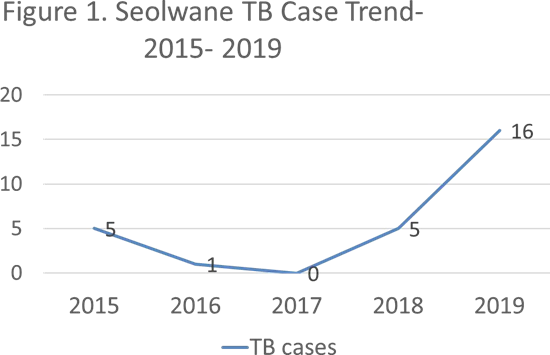
The trend confirmed the existence of a TB outbreak at Seolwane village which prompted the outbreak investigations.
Verify the diagnosis
Verifying the diagnosis was important: (a) to ensure that the TB was properly identified, since control measures are often disease-specific; and (b) to rule out laboratory error as the basis for the increase in reported cases.
The investigators visited the district microbiology lab and observed the lab processes. Clinical findings and laboratory results were reviewed. All Cases were diagnosed by using smear microscopy by an experienced microbiologist (Head of Microbiology). Standard Operating Procedures (SOPs) were followed when conducting tests. We also observed that sputum samples with a positive smear microscopy were also sent for culture and results were still pending. However, GeneXpert MTB/RIF was not always performed as the GeneXpert machine was broken and not working most of the year. Only 2 out of 16 cases in 2019 were diagnosed with GeneXpert MTB/RIF. This could also have caused to miss drug resistance TB cases and also other cases as this test is more sensitive and specific when compared to AFB microscopy (8).
Case definition
A case definition is a standard set of criteria for deciding whether an individual should be classified as having the health condition of interest. For our setting, the case definition was: “People living in Seolwane village who are microbiologically confirmed as having Tuberculosis by either smear microscopy and/ or GeneXpert between January 2019 and December 2019”.
Finding cases systematically and recording the information
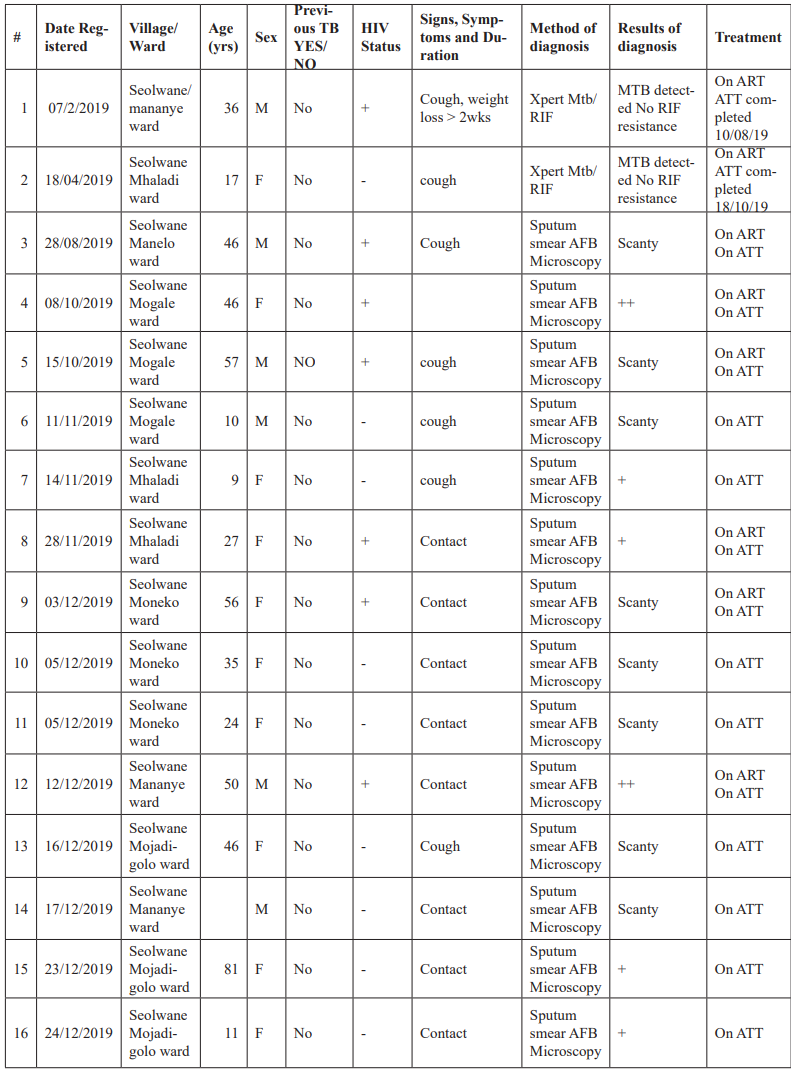
Following the case definition and other steps above, the cases were identified and recorded systematically using line list that the team developed.
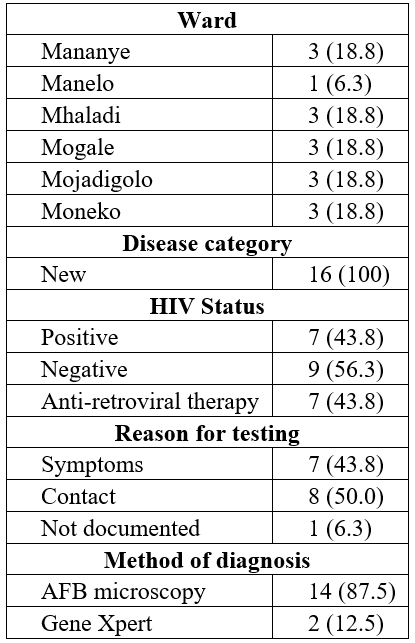
Table 1: TB Line list.
Perform descriptive epidemiology
With the information gathered, the outbreak was described in terms of time, place and person which provided clues about the source of the outbreak.
Time
The epidemic curve below shows a Propagated Source outbreak. A Propagated outbreak is due to transmission from one person to another, usually by direct person-to-person contact. The number of cases usually decrease after some time. This may be due to unavailability of susceptible persons or effective prevention and control measures [9]. TB management strategies including active case finding and case management were intensified in December 2019 which may explain the graph below.
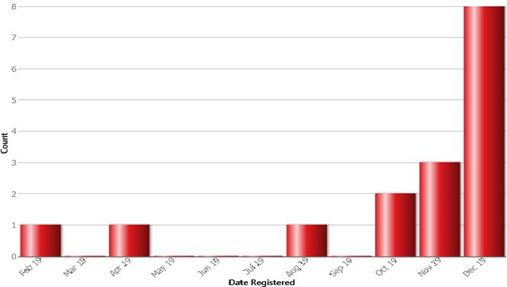
Figure 2: The Epi curve.
Place
Assessment of an outbreak by place does not only provide information on the geographic location of the problem, but may also demonstrate clusters or patterns that provide important etiologic clues. Spot maps and diagrams can be extremely helpful in identifying locations where cases may have been exposed to TB or where cases may have exposed others. The cases are marked with red spots on the map below and are equally distributed through all the wards in the village. There are no clusters of cases.

Figure 3: Seolwane spot map.
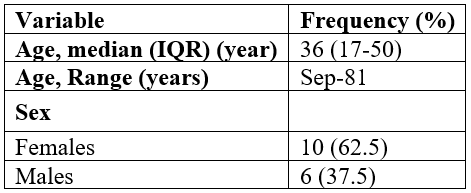
Person
Table below shows the characteristics of the TB patients In Seolwane village. The median age was 36 years (IQR 17-50). The age range was 9- 81 years. Of the 16 patients, 10 (62.5%) were males. All of the 16 patients were new notifications. The HIV status was positive in 7 (43.5%) of the TB patients. All of these were on ART therapy.
Table 1: Characteristics of TB patients in Seolwane village, 2019.
Develop hypotheses
The hypothesis developed was that there is a Propagated source of TB transmission at Seolwane village.
Evaluate hypotheses
The hypothesis was evaluated using a combination of clinical evidence, environmental evidence, laboratory science, and epidemiology. Furthermore, one to one interview was conducted with the local health personnel (a health education assistant and a nurse) were interviewed in order to get more information because they know the people in the community and their practices, and often may have important insights into the cause of the outbreak based on their knowledge and experience. The information gathered revealed that there was a possible chain of transmission from a propagated source which was linked to some workplaces such as the kgotla, primary school, a certain bar and homes as shown in the Figure 4.

Figure 4: Possible chains of transmission.
Epidemiologic data would help identify persons with TB disease involved in the same chain of recent transmission. TB genotyping offers a powerful tool to help direct the application of appropriate efforts. Genotyping could not be done as resources were not available.
Implementation of control and prevention measures
Community Mobilization was done through:
- Sensitization of village leaders such as Village Development Committee, Kgosi (the village Chief), Councillors and the Member of Parliament for the area.
- TB awareness campaigns were done at the Kgotla and the primary school through community health education, and also conducting TB Screening.
- Case surveillance and management
- Active Case Finding was done through contact tracing and symptom screening campaigns at the Kgotla, the primary school and house to house. In addition, active case finding was done at two classes at the primary school and also at the Bar. These places were not covered by the district officers in December 2019 when they were doing contact tracing. Where symptom screening was positive samples were collected for AFB smear microscopy.
- All patients were enrolled into Community TB Care (CTBC) after a thorough assessment.
- All cases were given anti-TB treatment. TB Preventive Therapy (TPT) was also given to eligible contacts who were not initially enrolled by the district officers. These were five under-fives who were living with people with TB.
- Monitoring and evaluation: We recorded the data, analysed it and produced a report to inform other actions required.
Communicate findings
The final task was to summarize the outbreak investigation, its findings, and its outcomes in a report and to disseminate the findings in an effective manner. This communication was in two forms:
- An oral briefing to the local authorities (Kgosi, VDC, councillors). The oral briefing was conducted by the Palapye DHMT staff who were responsible for implementing TB control and prevention measures in the district. The team described what they found, what they did, and what should be done in the village going forward.
- A written report with evidence of things done, discussed and recommendations was submitted to the DHMT, BNTP management and Ministry management.
Discussion
The primary goal of the outbreak investigation was to control the disease within the affected population and to prevent the disease from spreading to other populations through evidence-based interventions. Traditional contact tracing was not adequate to identify the outbreak in Selolwane village. Active case finding and laboratory testing played a prominent role in identification and confirmation of the outbreak. The active case finding did not only improve case detection but also unearthed the possibility of a chain of transmission between two or more cases which proved the evidence of the outbreak.
The outbreak investigation afforded detection of cases who were probably living with the disease and transmitting it and also early identification of more patients who benefited from early management of TB, preventing further morbidity and transmission. January and February 2020 the village had 2 cases per month highlighting the role of an outbreak
investigation in the control of TB. Contrary to the findings of other studies aluding to the fact that TB outbreaks are common in congregate lodging, this outbreak was in dispersed communities showing propagated source caused by spread of pathogen from one susceptible person to another without a common source [1-4].
After appropriately isolating a micro-organism, it is difficult to differentiate whether it is cross contamination or it is really from that sample. It is also difficult to establish the source of the outbreak. Microbiologically explaining the outbreak without a thorough outbreak investigation is also not easy [5]. This is due to the fact that an increase in TB cases can happen due to an influx of persons from areas where TB is common (e.g., refugees), persons are misdiagnosed with TB, as a result of mislabelling or contamination during specimen collection or in the laboratory (sometimes called false-positive laboratory results). In our investigation, the diagnosis was verified by an experienced microbiology technician proving that this was an actual outbreak. A standard definition of the exposed population is necessary to enable thorough case finding to be carried out to ascertain the presence and/ or absence of pseudo-outbreaks.
Seolwane is a low-incidence rural area. The village had 0–5 cases per year in the past four years before the outbreak (2015–2018). This outbreak led to an increase in the need for intensified TB investigations and case management. The health seeking behaviour and resource challenges in this outbreak are not unique to the village and have been encountered in other resource-limited settings. Treatment delays can be from the demand side where patients delay in seeking care or from the supply side where providers miss cases. Whatever the reason, treatment delays allow time for pulmonary TB disease progression leading to development of smear-positive disease and cavitation [11].
Limitations
The investigation encountered some limitations. Due to limited resources, some investigations such as geneXpert testing and genotyping were not done. Several studies have shown how vital GeneXpert testing is in the diagnosis of pulmonary tuberculosis [9,12–15]. In this investigation, due to an unavailability of resources, the GeneXpert machine in the area was out of service and therefore genexpert testing was not done on the samples. Due to an increased sensitivity of molecular testing over sputum microscopy, there is a possibility that some of the cases were missed and therefore under reporting the number of cases during the outbreak. This does not take away from the fact that an outbreak was verified and also control measures were put in place.
Genotyping is quite important in confirming the social links between patients in an outbreak. This is vital and demonstrates the significance of molecular epidemiology in TB control and surveillance. Genotyping isolates for M. tuberculosis have been used in several studies in low resource settings to identify clusters and guided further investigations (16-18). For our investigation, more evidence would have been gathered if TB genotyping was done to ascertain the strains of Mycobacterium in Seolwane village.
Conclusion
Outbreak investigations are an important intervention in any communicable disease. This outbreak would have been prevented had delays not occurred both from the demand side and supply side of managing TB. Due to limited resources, we could not do genexpert testing and genotyping of the samples from the outbreak investigation. Despite this, further cases were identified and initiated early on treatment preventing transmission of the disease and those eligible were initiated on TPT, contributing to the prevention and control of TB.
Acknowledgements: The authors wish to thank Palapye DHMT staff for participating in the investigation and communicating the findings.
References
- Mangura BT, Napolitano EC, Passannante MR, McDonald RJ, Reichman LB. Mycobacterium tuberculosis mini epidemic in a church gospel choir; CHEST, 1998; 113: 234-237.
- Mandell: Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 7th ed.Chapter 14. Copyright © 2009 Churchill Livingstone, An Imprint of Elsevier).
- Dholakia Y, Mistry N. Tuberculosis in congregate settings: Policies and practices in various facilities in Mumbai, India. Indian J Tuberc, 2017; 64(1): 10-13. doi: 10.1016/j.ijtb.2016.11.006. Epub 2016 Dec 16. PMID: 28166910.
- Bao H, Liu K, Wu Z, Wang X, Chai C, He T, et al. Tuberculosis outbreaks among students in mainland China: a systematic review and meta-analysis. BMC Infectious Diseases, 2019; 19: 972.
- Palmer SR. Epidemiology in search of infectious diseases: methods in outbreak investigation. J Epidemiol Comm Health, 1989; 43: 311–314.
- European Center for Disease Prevention and Control: Investigation and Control of Tuberculosis Incidents affecting children in congregate settings. Stockholm: ECDC, 2013.
- Stein-Zamir C, Volovik I, Rishpon S, Atamna A, Lavy1 A, Weiler-Ravelle D. Tuberculosis outbreak among students in a boarding school. Eur Respir J, 2006; 28: 986–991. DOI: 10.1183/09031936.06.00002506.
- Centers for Disease Control and Prevention. Module 9-Tuberculosis Outbreak Detection and Response.
- Agrawal Monika, Bajaj Ashish, Bhatia Vinay, Dutt Sarjana. Comparative Study of GeneXpert with ZN Stain and Culture in Samples of Suspected Pulmonary Tuberculosis. DOI: 10.7860/JCDR/2016/18837.7755
- Asch S, Leake B, Anderson R, Gelberg L. Centers for Disease Control and Prevention. Principles of Epidemiology. Lesson 1
- Why do symptomatic patients delay obtaining care for tuberculosis? Am J Respir Crit Care Med, 1998; 157: 1244–1248.
- Bowles EC, Freyée B, van Ingen J, Mulder B, Boeree MJ, van Soolingen D. Xpert MTB/RIF®, a novel automated polymerase chain reaction–based tool for the diagnosis of tuberculosis. Int J Tuberc Lung Dis, 2011; 15: 988–989.
- Miller MB, Popowitch EB, Backlund MG, Ager EP. Performance of Xpert MTB/RIF RUO assay and IS6110 real-time PCR for Mycobacterium tuberculosis detection in clinical samples. J Clin Microbiol, 2011; 49: 3458–362.
- Malbruny B, Le Marrec G, Courageux K, Leclercq R, Cattoir V. Rapid and efficient detection of Mycobacterium tuberculosis in respiratory and non-respiratory samples. Int J Tuberc Lung Dis, 2011; 15: 553–555.
- Marlowe EM, Novak-Weekley SM, Cumpio J, Sharp SE, Momeny MA, Babst A, et al. Evaluation of the Cepheid Xpert MTB/RIF assay for direct detection of Mycobacterium tuberculosis complex in respiratory specimens. J Clin Microbiol, 2011; 49: 1621–1623.
- Lowther SA, Miramontes R, Navara B, Sabuwala N, Brueshaber M, Solarz S, et al. Outbreak of Tuberculosis Among Guatemalan Immigrants in Rural Minnesota, 2008. Public Health Reports, 2011; 126.
- Smit PW, Vasankari T, Aaltonen H, et al. Enhanced tuberculosis outbreak investigation using whole genomesequencing and IGRA. Eur Respir J, 2015; 45: 276–279.
- Dobbs KG, Lok KH, Bruce F, Mulcahy D, Benjamin WH, Dunlap NE. Value of Mycobacterium tuberculosis fingerprinting as a tool in a rural state surveillance program. Chest, 2001;120: 1877-1882.
- Gardy JL, Johnston JC, Ho Sui SJ, Cook VJ, Shah L, Brodkin E, et al. Whole-genome sequencing and social-network analysis of a tuberculosis outbreak. N Engl J Med, 2011; 364(8): 730-739. doi: 10.1056/NEJMoa1003176. PMID: 21345102

