Comparison of RFF and ALT Flap in Head and Neck Reconstruction; One Single Center Experience
Giovacchini F1, Pignataro LV2,*, Mitro V1, Gilli M2 and Tullio A1
1Department of Maxillo-Facial Surgery, Santa Maria della Misericordia Hospital, Italy
2Department of Maxillo-Facial Surgery, University of Siena Faculty of Medicine and Surgery, Italy
Received Date: 12/08/2022; Published Date: 14/09/2022
*Corresponding author: Laura Viola Pignataro, Department of Maxillo-Facial Surgery, University of Siena Faculty of Medicine and Surgery, Siena, Italy
Abstract
Nowadays microsurgical free flap is the method of choice for head and neck reconstruction in case of large surgical gap and Radial Forearm Free (RFF) and Anterolateral Thigh (ALT) are two of the most used flaps in case of soft tissues defects. The purpose of this study is to present a single institution experience comparing outcomes in terms of free-flap survival and complications after head and neck reconstruction with ALT or RFF flaps and to show how ALT flap has become the preferred one thanks to its versatility for soft tissue reconstruction. Between April 2017 and April 2021 eighteen patients affected by head and neck cancer underwent a microvascular free flap reconstruction after head and neck tumor resection; fourteen ALT and four RFF surgical procedures were performed. In our opinion, the anterolateral thigh flap can be harvested safely and easily to reconstruct the complicated defects of head and neck. Primary closure could often be performed at the donor site and a variable pedicle permits different way of reconstruction. On the other hand, radial forearm free flap is the best option in case of intraoral lining defect. Anyway, individual patient factors and experience of the surgeon remain the determinants of the selection of the best reconstructive option.
Keywords: Anterolateral thigh flap; Head and neck cancer; Reconstructive surgery; Chimeric flap
Introduction
Head and neck cancer is among the most common cancers worldwide; the resection of malignant tumor can result in large and complex defects and gap reconstruction could be challenging for surgeons, considering outcomes in terms of tissue integrity, function and aesthetic.
Nowadays microsurgical free flap is the method of choice for head and neck reconstruction [1] in case of large surgical gap and Radial Forearm Free Flap (RFFF) and Anterolateral Thigh (ALT) are two of the most used flaps in case of soft tissues defects [2]. The radial forearm free flap was first described in 1981 by Yang et al. [3]. This flap has a thin texture, which facilitates harvesting procedure and a long constant pedicle with large caliber. At the same time there are limits connected to this flap that should be considered when thinking about reconstruction. The dissection of RFF flap implies the sacrifice of a major blood vessel to the hand and the wound closure at the donor site often requires a skin graft to be harvested.
On the other hand, the ALT flap is a typical perforator flap that has gained popularity since its introduction in 1983 by Baek [4]. First it was used in different sites such as upper and lower extremities and trunk, subsequently Koshima et al. [5] started to use it for head and neck reconstruction. One of the advantages of this flap is that it allows the transfer of different kind of tissues with large amounts of cutaneous and subcutaneous fat tissue of adjustable thickness.
The vascular pedicle has more anatomical variability respect to RFFF, but the length and relatively large-diameter vessels often permit good harvesting despite of a longer dissection. Moreover, lower donor site morbidity makes the ALT flap an ideal reconstructive option.
The purpose of this study is to present a single institution experience comparing outcomes in terms of free-flap survival and complications after head and neck reconstruction with ALT or RFF flaps and to show how ALT flap has become the preferred one in our institution thanks to its versatility for soft tissue reconstruction.
Case Series
Between April 2017 and April 2021 eighteen patients affected by early (stage I-II) or advanced (stage III-IV) head and neck cancer were treated at the Department of Maxillo-Facial Surgery, Santa Maria della Misericordia Hospital, Perugia (Italy). Total number of surgical procedures decreased dramatically between March 2020 and December 2021 and this change took place due to Covid-19 pandemic viral infection. All patients in our department had oncological disease and underwent composite resection with excision of the primary tumor, including for most of all ipsilateral or bilateral neck dissection and microvascular flap reconstruction. Eighteen free-flap procedures (ALT or RFF) were performed to reconstruct surgical defects. Patients were divided into two groups according to microsurgical reconstruction: ALT group (n=14) and RFF group (n=4). Analysis of the following demographic and clinical variables was conducted for each group: patient sex and age, tumor localization, days of hospitalization, flap survival. Complications were classified in systemic and local complications, separated in donor site or receiving site morbidities. Written consent from was obtained from all patients.
Results
Eighteen patients underwent a microvascular free flap reconstruction after head and neck tumor resection; fourteen ALT and four RFF surgical procedures were performed. Twelve of the patients were males, six females. The age of most of the patient at the time of surgical procedure was over sixty years; just in one case a demolitive surgery procedure for tongue cancer ablation was performed in a 21-years old male. Among these tumors, six were located in left or right maxilla and partial maxillectomy was necessary. In two patients parotidectomy was performed since the origin of the disease was parotid gland. Two patients underwent exenteratio due to a fronto-orbital skin tumor involving eyelid tissues. In other two patient’s ablation of a tumor of the floor of the mouth was performed. In one case removal of frontoparietal tumor required demolition of cutaneous, subcutaneous, muscular and cortical bone tissues since the cancer was radiologically involving the skull. One patient underwent a removal of genian region tumor. Three patients required a hemiglossectomy for tongue cancer removal and in last one patient a massive oral cavity demolition was performed since the tumor was extended from oropharynx to mandible.
The microsurgical success rate, expressed as flap survival was 100%, in case of both ALT and RFF groups. No second-free flap surgery was necessary.
All this data is summarized in Table 1, 2.
Table 1
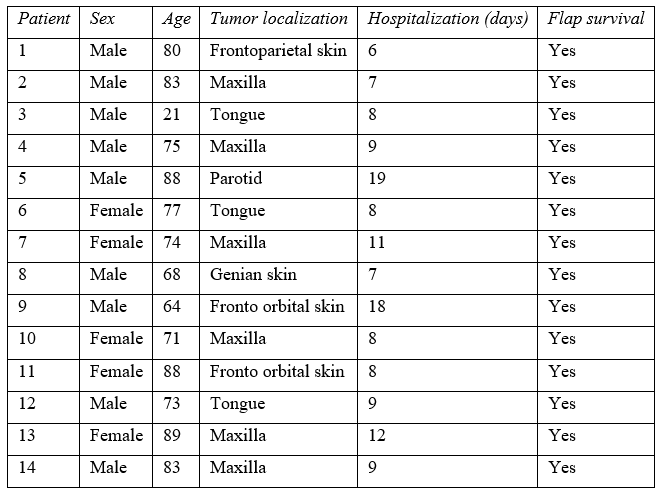
Table 2

Complications were classified in systemic and local complications, separated in donor site or receiving site morbidities. Systemic complications were experienced by two patients from ALT group consisting in nosocomial pneumonia; one of these two got complicated with respiratory failure and several days of hospitalization to restore before discharge were required.
In one of this two patients a minor receiving site morbidity also occurred; delayed healing was observed in a millimetric extremities of the flap where connection with accepting tissues were required. No other receiving site morbidities were observed in other patients.
Minor donor site complications were observed in five cases of ALT group. In one patient infection of the donor-site occurred 52 days after surgery; debridement and surgical curettage in local anesthesia were performed and antibiotic intravenous therapy was administered.
In other four patients second intention healing of the wound at the donor site occurred due to inability to suture skin flaps to restore a large surgical defect; subsequently second intention healing was obtained. In one of these cases a skin graft was harvested to repair the surgical gap, but skin graft loss was observed and subsequently second intention healing was obtained.
In contrast, second intention healing was observed in every patient submitted to RFF flap harvesting and donor site infection manifested in one of these.
Skin graft harvesting was always necessary in these patients. Moreover, a linear scar was also observed because of the need of more proximal dissection to obtain a longer pedicle and it always resulting in a hypertrophic scarring.
Patients of both groups developed hyperpigmentation of the skin-grafted area.
Donor site major complications weren’t observed; severe hematoma, compartment syndrome or functional impairment were not experienced in patients submitted to surgical procedures in our department.
All this data is summarized in Table 3, 4.
Table 3
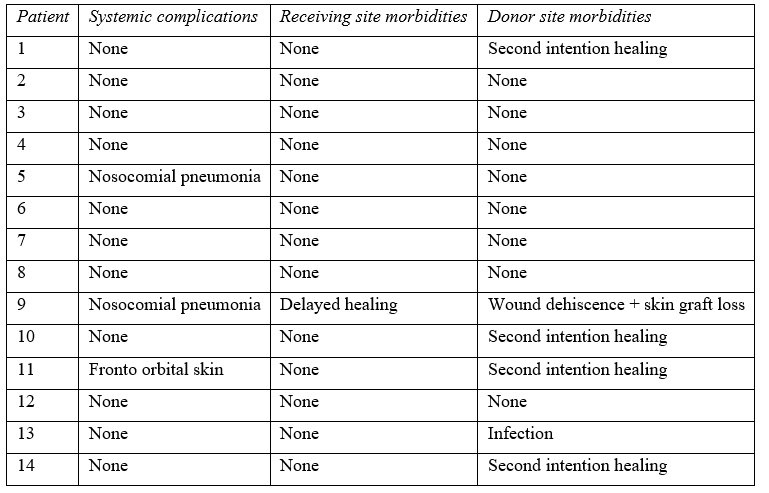
Table 4

Discussion
Reconstruction surgery after head and neck cancer resection is always challenging.
The RFF and ALT are two types of free flaps frequently used for complex reconstruction; the decision about the appropriate flap should consider the restoration of integrity, form and function of the demolition site and it is crucial to obtain optimal long-term outcomes. Flap reliability and surgical technique also are two variable that should influence the reconstructive decision. One of the preferred flaps in the defects of small volume and great surface is the radial forearm flap; according to Valentini et al. [6], its thinness permits to achieve great outcomes when used as a thin intraoral lining flap for reconstruction of the floor of the mouth defects. However, since its introduction the ALT flap has become the preferred donor site for soft tissue reconstruction for several authors [7,8] thanks to its versatility and especially when more soft tissue bulk is needed. The purpose of this study is to present a single institution experience in comparing outcomes in terms of free-flap survival, complications and morbidity of the donor site after head and neck reconstruction with ALT or RFF flaps and to show how ALT flap has become the preferred one thanks to its versatility for soft tissue reconstruction. Nevertheless, the main limits of this study are the limited number of patients included and the unequal distribution of patients between the two groups.
First, directions to use one or the other flap to restore surgical gap could be different. As ALT can provide soft tissue with sufficient volume and versatile shapes, it should be used for relatively large defects; it has good pliability and can be designed as either a single skin paddle for one-layer defect reconstruction or double-skin paddles for full-thickness defects supported by one or multiple perforators. Radial forearm free flap has the advantages of thinness, pliability, reliability of survival and a long constant pedicle, but skin paddle is usually smaller.
Surgical harvesting technique is important to be considered. While RFF harvesting is relatively easy to perform, ALT dissection is more difficult, due primarily to the anatomy of the perforator originating from the descending branch of the lateral circumflex femoral artery. Studies have described the anatomical variability of this perforator vessel, but few reports have shown the absence of this perforator [9-11]. Nevertheless, the arterial vessel which is always accompanied by two veins has diameters that usually facilitates an easier microvascular anastomosis.
Allen test is a valid instrument to understand practicability of RFF since disposal of a major artery to the hand is another drawback of this flap. When abnormal clinical Allen test is obtained, a modified surgical Allen's test could be performed to assess collateral flow to the hand.
A sterile pulse oximeter is placed on one finger of the hand where flow must be evaluated and saturation is registered. Radial artery is surgically exposed and a vascular clamp is applied. After deflation of the tourniquet, hand and digit perfusion is assessed with return of color, turgor and saturation value. With normal collateral perfusion a radial forearm flap could be harvested.
On the other hand, doppler ultrasound could be used to localize the perforator vessel; it could help to perform a faster and safer muscular dissection and preparation of the ALT flap that in our hands could be harvested in about 90 minutes. Although this advantage, in our experience many times wasn’t possible to find correspondence between the vessels evidenced with ultrasound test and the ones found during surgical procedures. Doppler ultrasound certainly offers a valid support during surgical preparation, but it couldn’t be considered necessary.
Moreover, the anatomical variability of anterolateral thigh perforators doesn’t influence microsurgical outcomes in our experience. Shieh et al. [12] have classified the vascular variation of the ALT pedicle into four types based on the derived perforator and the direction in which it crossed the vastus lateralis muscle; In type 1 (vertical musculocutaneous perforator), the perforator is vertically derived from the descending branch of the lateral circumflex femoral artery. In type 2 (horizontal musculocutaneous perforator), the perforator is derived from the transverse branch of the lateral circumflex femoral artery and runs parallel with the vastus lateralis muscle. In type 3 (vertical septocutaneous perforator), the origin of the perforator is the descending branch of the lateral circumflex femoral artery. In type 4 (horizontal septocutaneous perforator), the perforator is derived from the transverse branch of the lateral circumflex femoral artery and runs parallel with the vastus lateralis muscle.
Furthermore, variability of ALT perforators vessels sometimes could be a benefit.
When large demolition surgery is performed, the resulting shape of the defect could not be favorable for the insetting of the flap and reconstruction with RFF couldn’t be possible. The possibility to harvest ALT flap with two or more perforators vessels permits to obtain a chimeric flap such as the one performed in our department to repair a large surgical defect in maxillary carcinoma in which mucosal and skin gap had to be replaced.
Results indicate versatility of the ALT flap also related to receiving site; in our experience different kind of reconstruction could be performed with this flap, from intraoral defects to large cranial defects also with dural exposition. Moreover, depending on the surgical gap that must be replaced, preoperatory programme could be changed during surgical procedure when ALT flap harvesting is performed. In fact, versatility of this flap permits the surgeon to decide dimensions and geometry of the flap expressed in length, width and thickness of the tissues in the operatory room. In our experience, surgical demolition programme could not always be respected due to differences between preoperatory radiological finding and intraoperative finding in oncological patient.
This versatility is an important advantage of ALT flap that could not be obtained with RFF harvesting that is especially indicated as a thin lining flap.
Results show that there’s no significant differences in terms of flap survival rates between RFF and ALT; approximately in line with the results achieved by Liu et al. [13], our study demonstrates that there was no flap failure.
Hospitalization expressed in terms of days, could be influenced by different variable, including operating time which is one of the most variable data. Depending on surgeon experience but mostly on demolition surgery, removal of a tumor could require more or less time determined by dimensions, localization and important structures proximity. However, from 6 to 19 days could be necessary; when approaching small tumors, localized in areas that do not require extra procedures, such as ventilatory support tracheotomy, few days of hospitalization are sufficient. Similar results could be reached when the patient is young and healthy.
Surgical treatment of a larger tumor, older patient or comorbidity are factors affecting days of hospital stay. In our experience longer hospitalization was necessary in two patients when systemic complications occurred, consisting in nosocomial pneumonia. One of these two patients got complicated with respiratory failure, but both patients had underlying systemic conditions which could facilitated development of complications. Otherwise, all patients of our study that submitted an oral cancer ablation immediately underwent a logopedic first evaluation and following controls to restore deglutition reflex and speech as soon as possible without consequences. A strict programme of prophylactic exercises and the teaching of swallowing maneuvers can reduce specific impairments, maintain functions and enable a faster recovery ensuring post-treatment rehabilitation. A restorative protocol should be targeted at specific physiological deficits and volitional control to compensate for changes of the anatomy and physiology of the body. This can reduce the risk of aspiration, malnutrition and improve quality of life of those patients. Logopedic figures, restorative dental surgeon and/or prosthetic technician should work closely together to get the best outcomes for patients.
One last determinant that our study consider is donor site morbidity. Although primary closure is usually achieved with the harvesting of anterolateral thigh flap, wound dehiscence was the most frequent complication that occurred in others despite of ten of eighteen patients that didn’t manifest morbidities. In these patients, a very large defect had to be corrected after demolition surgery.
In one case in which skin graft was harvested, its loss was registered; underlying systemic disorder and patient collaboration are two factors that should be considered when thinking about this solution. In other patients second intention healing was obtained without additional patient discomfort. Just in one case, a female patient manifested an infection of the donor-site 52 days after surgery. Debridement and surgical curettage in local anesthesia were performed and antibiotic intravenous therapy was administered.
In contrast, as observed by Yang et al. [14], primary repair of the donor site is not usually possible with radial forearm free flap harvesting and the scar cannot be easily hidden. Even though the use of an acellular dermal matrix (such as Hyalomatrixâ in our experience) in a forearm defect after radial forearm free flap harvesting can improve skin elasticity and moisture, it still leaves a conspicuous scar resulting in a painful wound and numbness that is visible on the forearm. Furthermore, split-thickness skin grafts from the forearm can result in restriction of range of motion of the interested arm and disability because dense scars form on the skin and graft tendon adhesions may develop.
Risk of exposing important structures, such as arm’s tendons and nerves has to be considered.
Moreover, the strategy implemented in our department provides for early mobilization of the patient in order to have a rapid recovery and a return to a good quality of life as soon as possible.
It also provides short hospitalization reducing risk of nosocomial infections.
Nevertheless, early mobilization of the patient could be counterproductive in term of wound healing of the donor site in case of ALT flap harvesting when a skin graft is required. While a radial forearm skin graft could be secured with a plaster cast and patient mobilization could start safer, inevitably an ALT skin graft suffers from movement and delayed healing occurs more easily.
Finally, something to keep in mind is donor site paresthesia. Due to its anatomical location, the medial branch of the lateral cutaneous nerve of the thigh can be injured or sacrificed during ALT flap elevation, or may be included to make the flap sensate, leading to lateral thigh paresthesia. When injured, different techniques could be suitable to restore the integrity of the nerve [15].
Therefore, depending on the setting, paresthesia may not be considered a complication as much as an anticipated consequence of surgery and donor site morbidity is not significant following an anterolateral thigh free flap.
Conclusion
In conclusion, in our experience both RFF and ALT free flaps are two valid reconstructive options in head and neck after cancer ablation. Free-flap survival is the same in our hands, but donor-site morbidity appears to differ after surgical reconstruction with anterolateral thigh or radial forearm free flap. ALT flap gives optimal results either at the donor site and at the accepting site, being easy to harvest and providing an ideal reconstructive choice. When thinking about anterolateral thigh flap for intraoral defect, such as the one following a hemyglossectomy, laser-therapy could be a valid option to consider permitting to reduce patient discomfort after surgical procedure. In our opinion, nowadays the anterolateral thigh flap can be harvested safely and easily to reconstruct the complicated defects of head and neck. Primary closure could often be performed at the donor site and a variable pedicle permits different way of reconstruction. On the other hand, radial forearm free flap is a valid alternative especially in case of intraoral lining defect in women with elevated BMI where subcutaneous fat tissue could make the harvesting of ALT flap harder. Anyway, in our experience ALT flap could be considered the right reconstructive method for large and composite defects. Individual patient factors and experience of the surgeon remain the determinants of the selection of the best reconstructive option.
Conflicts of Interest: All authors declared no conflicts of interest
Grant Information: The authors received no specific funding for this work.
References
- Urken ML, Weinberg H, Buchbinder D, et al. Microvascular free flaps in head and neck reconstruction: report of 200 cases and review of complications. Arch Otolaryngol Head Neck Surg, 1994; 120: 633-640.
- Kim EK, Evangelista M, Evans GR. Use of free tissue transfers in head and neck reconstruction. J Craniofac Surg, 2008; 19: 1577–1582.
- Yang GF, Chen PJ, Gao YZ, Liu XY, Li J, Jiang SX, et al. Forearm free skin flap transplantation: a report of 56 cases. 1981. Br J Plast Surg, 1997; 50(3): 162-165.
- 4. Baek SM. Two new cutaneous free flaps: the medial and lateral thigh flaps. Plast Reconstr Surg, 1983; 71: 354-365.
- Koshima I, Fukuda H, Yamamoto H, et al. Free anterolateral thigh flaps for reconstruction of head and neck defects. Plast Reconstr Surg, 1993; 92: 421-430.
- Valentini V, Cassoni A, Marianetti TM, Battisti A, Terenzi V, Iannetti G. Anterolateral thigh flap for the reconstruction of head and neck defects: alternative or replacement of the radial forearm flap? J Craniofac Surg, 2008; 19(4): 1148-1153.
- Chen CM, Chen CH, Lai CS, et al. Anterolateral thigh flaps for reconstruction of head and neck defects. J Oral Maxillofac Surg, 2005; 63: 948Y952.
- Chana JS, Wei F-C. A review of the advantages of the anterolateral thigh flap in head and neck reconstruction. Br J Plast Surg, 2004; 57: 603Y609.
- Kimata Y, Uchiyama K, Ebihara S, Nakatsuka T, Harii K. Anatomic variations and technical problems of the anterolateral thigh flap: a report of 74 cases. Plast Reconstr Surg, 1998; 102: 1517–1523.
- Koshima I, Fukuda H, Utunomiya R, Soeda S. The anterolateral thigh flap: variations in its vascular pedicle. Br J Plast Surg, 1989; 42: 260–262.
- Wong CH, Wei FC. Anterolateral thigh flap. Head Neck, 2010; 32: 529–540.
- Shieh SJ, Chiu HY, Yu JC, et al. Free anterolateral thigh flap for reconstruction of head and neck defects following cancer ablation. Plast Reconstr Surg, 2000; 105: 2349Y2357.
- M: Reconstruction of soft-tissue defects of the head and neck: Radial forearm flap or anterolateral thigh flap? Eur Arch Otorhinolaryngol, 2011; 268: 1809-1812.
- Yang S, Hong JW, Yoon IS, Lew DH, Roh TS, Lee WJ. Anterolateral thigh free flaps and radial forearm free flaps in head and neck reconstruction: A 20-year analysis from a single institution. Arch Plast Surg, 2021; 48(1): 49-54.
- Gennaro P, Gabriele G, Mihara M, Kikuchi K, De Caris F. Side-to-end trigeminal to trigeminal fascicular neurorrhaphy to restore lingual sensibility: a new technique. J Reconstr Microsurg, 2014; 30(3): 211-214.

