Severe Covid Manifestations in Pregnant Women in the South of Colombia: A Series of 4 Case
Jairo Antonio Rodriguez Rodriguez*
Department of Pediatrics, University Hospital of Neiva, Surcolombiana University, Colombia
Received Date: 01/08/2022; Published Date: 10/08/2022
*Corresponding author: Jairo Antonio Rodriguez Rodriguez, Faculty of Health, Department of Pediatrics, University Hospital of Neiva, Surcolombiana University, Calle 9 # 14-02, Neiva, Colombia
Summary
Objective: To describe the clinical presentation and outcome of 4 pregnant women with severe respiratory infection secondary to severe acute respiratory syndrome due to coronavirus 2 in women from southern Colombia.
Materials and Methods: Pregnant women attended at the Hospital Universitario de Neiva, who met the definition of severe COVID-19, between September and November 2020.
Results: 4 pregnant women under 35 years of age, presented with severe pneumonia and severe preeclampsia, required ICU, mechanical ventilation, two extracorporeal membrane oxygenation (2); CRP and LDH increased, there was lymphopenia and reduction of neutrophil/lymphocyte ratio. One neonate was positive for SARS-CoV-2. Three mothers and one neonate died.
Discussion: The risk of severe Covid in pregnant women is higher, this is related to pregnancy factors and preeclampsia, with previous references to this association in mothers with COVID 19. The high mortality found and vertical transmission in one of the cases is noteworthy.
Conclusions: The development of severe preeclampsia in all 4 cases impacted triggered death in 3 of them, lymphopenia and reduced neutrophil/lymphocyte ratio is suggested as a prognostic factor. Future studies will elucidate the consequences of COVID-19 on gestation.
Keywords: COVID-19 In pregnancy; Acute respiratory infection; Pregnant women; Pre-eclampsia
Introduction
In pregnant women, coronavirus infection including Middle East respiratory syndrome (MERS CoV2), severe acute respiratory syndrome (SARS CoV1 and SARS CoV2), has the potential to cause major complications as it increases preterm delivery 14.3% (10.2-30.2), preeclampsia 5.9% (3.6-11. 7), admission to Intensive Care Units (ICU) 31.3% (27.2-55.5), intrauterine growth restriction (IUGR) 2.8% (1.8-8.9), fetal distress 26.5% (17.5-39. 5), admission to neonatal intensive care unit (NICU) 11.33% (5.6-20.3) and perinatal death 2.2 (1.2-12.8) [1], but overall it has a mild to moderate clinical behavior [2,3]. Initial reports in 2020 showed admission to the ICU of 2 (2.98%) pregnant women among 67 cases of COVID 19 in pregnant women [4].
Some risk factors for developing severe COVID-19 include maternal age older than 35 years OR 1.78 (1.25-2.55), body mass index greater than 30 kg/m2 OR 2.38 (1.67-3.39), history of hypertension OR 2.0 (1.14-3.48) and diabetes OR 2.51 (1.31-4.80) [5].
There have been attempts to find widely used and inexpensive biological markers to discern which pregnant women with SARS CoV2 infection will have a higher risk of complications, among which the Neutrophil/Lymphocyte Ratio (NLR) is a tool that could be useful, Anggraini and Sulistyowati [6] whose reported value of less than 5.8 is synonymous with a lower risk of complications.
This review aims to describe the clinical presentation of a case series of pregnant women in Neiva, a city located in south-central Colombia, who developed severe SARS-CoV-2 infection. There are no reports to date in Colombian pregnant women that allow us to know if they have had a behavior similar to that reported in other countries.
Case 1
A 27-year-old woman, in her 34th week of third gestation with cough, asthenia, adynamia and fever of 10 days, oligohydramnios, positive PCR for SARS-CoV-2. On admission, she presented cough with no other findings, management for pneumonia was started with ampicillin/sulbactam and clarithromycin and RECOVERY protocol for patient with COVID-19 was established. Two days later, procalcitonin-negative antibiotics were discontinued and oxygen support by nasal cannula at 3 L/min was started. Blood pressure was elevated: 138/85 mmHg and fetal lung maturation scheme with betamethasone was indicated. On day 4 she presented progressive increase in respiratory effort and deterioration of oxygenation, reaching PaFi of 123.2 mmHg; interstitial pneumonia with ground-glass pattern, cesarean section was performed. Subsequently, she continued with hypertension, headache, hyperreflexia, proteinuria and was started on magnesium sulfate for severe preeclampsia. On day 9 she presented cardiorespiratory arrest that responded to cardiopulmonary resuscitation maneuvers requiring vasopressor support and mechanical ventilation. Due to fever, amikacin and cefepime were administered. On day 11 he presented deep vein thrombosis; enoxaparin was administered. On day 12 due to rising hypoxemia and hypercapnia, she was transferred to receive ECMO therapy but died. The neonate had positive PCR for SARS-CoV-2 asymptomatic and was discharged without complications.
Case 2
35-year-old primiparous woman in week 31, obese, polyhydramnios and gestational diabetes. She has 8 days of fever, asthenia, cough and progressive dyspnea with hypertension. PCR confirmed COVID-19. She was admitted to the ICU for dyspnea with PaFi of 163 mmHg, oxygen was started by non-rebreathing mask, thromboprophylaxis with enoxaparin and fetal lung maturation with betamethasone. Preeclampsia with proteinuria and hypertension was managed with magnesium sulfate. Cesarean section was performed after presenting hypoxemia and PaFi of 93 mmHg. On day 5 of hospitalization, she was fully anticoagulated and mechanically ventilated due to imminent ventilatory failure, and reported infiltrates with severe bilateral pneumonic compromise. Broad-spectrum antibiotic coverage was started with piperacillin-tazobactam. On day 6, due to hypotension, noradrenaline was added and maintained for 2 days, reporting elevated D-dimer, ferritin, LDH and CRP. Stationary evolution for 3 days, compromised oxygenation and respiratory acidemia. On day 9, methicillin-resistant Staphylococcus epidermidis was documented, requiring adjustment to ampicillin-sulbactam, vancomycin and clarithromycin. On day 12, he showed radiological and clinical improvement. On day 13 he has visual contact, ventilatory requirements are gradually withdrawn. On day 16 oxygen was suspended and on day 20 she was discharged with a negative SARS-CoV 2 neonate.
Case 3
32-year-old primiparous woman in week 32 with hypothyroidism treated with levothyroxine. She was admitted with clinical symptoms of 4 days of evolution consisting of persistent fever, anosmia, dyspnea on medium effort and SARS-CoV-2 infection confirmed by PCR. He presented increased respiratory effort with evidence of severe oxygenation disorder after reaching PaFi 54 mmHg, requiring invasive mechanical ventilation. She was admitted to the ICU in ventilatory failure with anhydramnios and category III fetal monitoring, so a cesarean section was performed. The neonate required CPR maneuvers and advanced life support, with subsequent transfer to the neonatal ICU. The patient remained on ventilatory support (FiO2 90-100%) including prone-supine ventilation, prophylactic enoxaparin and pseudoanalgesia with midazolam and fentanyl, with no changes in her evolution until day 4 when she presented sudden deterioration of oxygenation, signs suggestive of PTE, and was transferred to full anticoagulation, On the 6th day, fever and elevation of acute phase reactants began, with continued stationary evolution until the 12th day when arterial hypertension in crisis range and positive proteinuria were documented, magnesium sulfate was added, refractory hypoxemia on the 14th day and ECMO therapy was recommended, but she died on the 31st day of hospitalization.
Case 4
Primiparous 19-year-old pregnant woman of 31 weeks with clinical symptoms of 8 days of evolution consisting of fever, headache, asthenia, anosmia and edema of the lower limbs, hypertension with elevated aminotransferases and thrombocytopenia, diagnosis of HELLP syndrome. Admitted to ICU, with severe hypertension without dyspnea, positive PCR for SARS-CoV-2; magnesium sulfate and fetal lung maturation scheme were started. On day 2 she had positive proteinuria. On day 3 she underwent cesarean section and due to persistent hypertension a second drug was added. She developed dyspnea that was temporarily corrected with a non-rebreathing mask. Images showed 95% pulmonary compromise, there was a decrease in saturation levels, she could not tolerate prone decubitus; she evolved to ventilatory failure and invasive mechanical ventilation was started. On day 5 in poor general condition, severe oxygenation disorder and mixed acidosis, azotemia and prolonged coagulation times. On day 7 fever, leukocytosis and positive acute phase reactants are considered septic shock, antibiotics and renal replacement therapy are indicated. On day 9 he had multiorgan failure, on day 16 blood culture positive for Pseudomona aeruginosa, so antibiotic therapy was adjusted. On day 18 ventilatory failure, multiorgan failure, asystole without response to maneuvers and died. The neonate, although negative for SARS-Cov-2, died in the NICU.
Results
Among the findings were a mean maternal age of 28.2 years (19-35 years), gestational age 32 weeks (31-34 weeks), days of illness at admission 7.2 (4-10 days), hospital stay 16 days (12-20 days), all had lymphopenia and increased neutrophil/lymphocyte ratio. Mortality occurred in 3 of the mothers and in one of the newborns. Other data are shown in Table 1.
The symptoms found were fever in 100%, cough and dyspnea in 3 of 4 pregnant women (75%). Two patients had thromboembolism, one of them with deep vein thrombosis and another with pulmonary thromboembolism despite receiving thromboprophylaxis.
Table 1: Clinical and lab findings in pregnancy with severe COVID-19 grave.
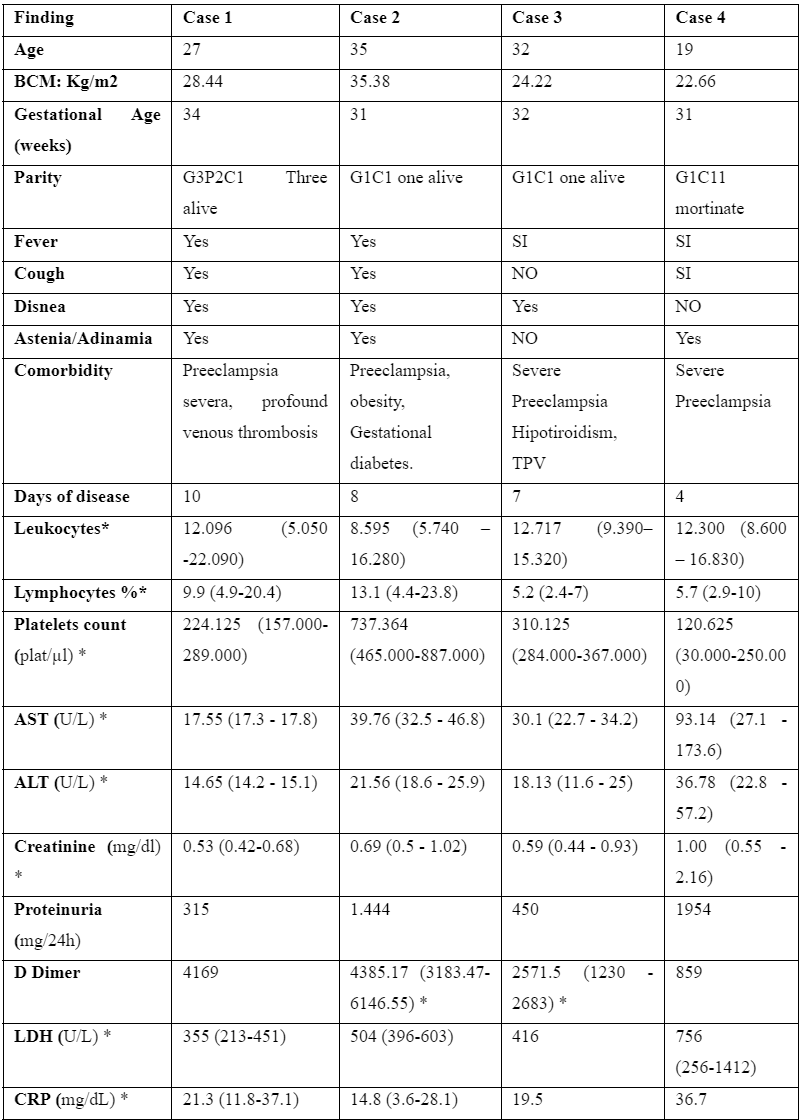
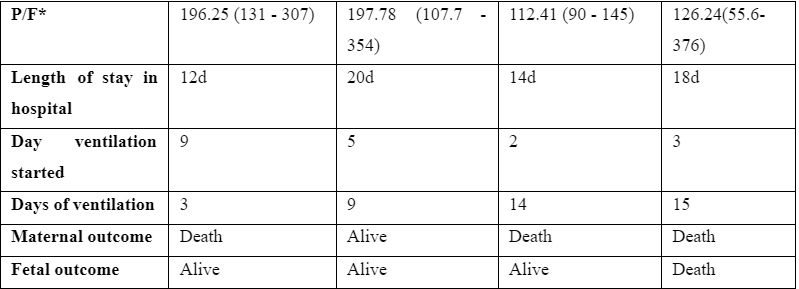
* mean and range
BMI: Body Mass iIdex ; AST: Aspartate aminotransferase; ALT: Alanine aminotransferase; LDH: Lactate Dehydrogenase; CRP: C-reactive protein;; P/F: relation between arterial oxygen tension and fraction of inspired oxygen (PaO2/ FIO); TPV: PT : pulmonary thromboembolism;
Discussion
The age of 28 years in these pregnant women is lower than that reported by Sentilhes Le et al, who state that age becomes a risk factor for severe COVID 19 in those over 35 years of age [7].
This could be related to the findings described in the study of Shaness et al. [8], in which the placentas of patients with SARS-CoV-2 infection show a greater presence of decidual arteriopathy and other characteristics of poor maternal vascular perfusion, reflecting an inflammatory state and hypercoagulability, similar to pathologies related to placental insufficiency [9]. It has been described that LDH, CRP, ferritin and D-dimer levels are considerably higher in severe cases, which was observed in the patients described, suggesting a higher level of systemic inflammation in them [10]. It is noteworthy that case number 2, who was the only survivor, presented higher total lymphocyte values and lower NLR compared to the other cases, on day 13, a parameter that persisted in subsequent days. At the beginning of the pandemic, it was reported that lymphocyte counts lower than 5% were associated with higher admission to the ICU; values higher than 20% were considered a good prognosis [11]. This value reinforces this finding found in the 4 patients described.
Another aspect commented during infection by COVID-19 is the alteration in the expression of the ACE2 receptor, which is increased in placental tissue favoring hypertensive disorders of gestation [3,12]; this receptor is also expressed in lymphocytes and may be one of the causes of lymphopenia (11). Mendoza et al, postulates a similar syndrome to preeclampsia in patients with severe SARS-CoV-2 infection, who met the criteria for preeclampsia, but who recovered without the need to disinfect, obtaining improvement once the infectious condition is resolved [13]. In one of the 4 newborns in this series, a positive PCR test for SARS-CoV-2 was demonstrated, reinforcing the risk of vertical transmission reported in approximately 3.2% of pregnancies during the third trimester [14].
Conclusion
- The development of severe preeclampsia in the 4 cases of pregnant women with COVID impacted them negatively.
- There was maternal-fetal transmission in 1 of the 4 cases.
- Lymphopenia and increased neutrophil/lymphocyte ratio are poor prognostic factors in pregnant women who acquire SARS CoV-2 infection.
References
- Diriba K, Awulachew E, Getu E. The effect of coronavirus infection (SARS-CoV-2, MERS-CoV, and SARS-CoV) during pregnancy and the possibility of vertical maternal-fetal transmission: a systematic review and meta-analysis. Eur J Med Res, 2020; 25: 39.
- Di Toro F, Gjoka M, Di Lorenzo G, De Santo D, De Seta F, Maso G, et al. Impact of COVID-19 on maternal and neonatal outcomes: a systematic review and meta-analysis. Clin Microbiol Infect, 2021; 27(1): 36-46.
- Todros T, Masturzo B, De Francia S. COVID-19 infection: ACE2, pregnancy and preeclampsia. Eur J Obstet Gynecol Reprod Biol, 2020; 253: 330.
- Borre-Naranjo D, Santacruz J, Gonzalez-Hernandez J, Anichiarico W, Rubio-Romero J. Infección por SARS-CoV-2 en la paciente obstétrica: una perspectiva desde el cuidado crítico [SARS-CoV-2 infection in the obstetric patient: a perspective from critical care]. Acta Colom Cuidado Intens, 2020; 20: 98–107.
- Allotey J, Stallings E, Bonet M, Yap M, Chatterjee S, Kew T, et al. Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis. BMJ, 2020; 370: m3320.
- Anggraini NWP, Sulistyowati S. Low neutrophil to lymphocyte ratio decreases risk of coronavirus disease in pregnant women. Universa Medicina, 39(2): 88–96.
- Sentilhes L, De Marcillac F, Jouf- frieau C, et al. Coronavirus disease 2019 in pregnancy was associated with maternal morbidity and preterm birth. Am J Obstet Gynecol, 2020; 223: 914.e1-15.
- Carrasco I, Muñoz-Chapuli M, Vigil-Vázquez S, et al. Infección por SARS-COV-2 en gestantes y recién nacidos en una cohorte española (GESNEO-COVID) durante la primera ola. BMC Embarazo Parto, 2021;21: 326.
- Wastnedge EAN, Reynolds RM, van Boeckel SR, Stock SJ, Denison FC, Maybin JA, et al. Pregnancy and COVID-19. Physiol Rev, 2021; 101(1): 303-318.
- Chen G, Wu D, Guo W, Cao Y, Huang D, et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest, 2020; 130(5): 2620-2629.
- Tan L, Wang Q, Zhang D, dDing J, Huang Q, Tang YQ, et al. Lymphopenia predicts disease severity of COVID-19: a descriptive and predictive study. Signal Trans Targ Ther, 2020; 5: 33.
- Coronado-Arroyo JC, Concepción-Zavaleta MJ, Zavaleta-Gutiérrez FE, Concepción-Urteaga LA. Is COVID-19 a risk factor for severe preeclampsia? Hospital experience in a developing country. Eur J Obstet Gynecol Reprod Biol, 2021; 256: 502-503.
- Mendoza M, Garcia Ruiz I, Maíz N, Rodo C, Garcia-Manau P, Serrano B, et al. Pre-eclampsia syndrome induced by severe COVID-19: a prospective observational study. BJOG 2020.
- Kotlyar AM, Grechukhina O, Chen A, Popkhadze S, Grimshaw A, Tal O, et al. Vertical transmission of coronavirus disease 2019: a systematic review and meta-analysis. Am J Obstet Gynecol, 2021; 224(1): 35-53.e3.

