Opiate Narcotics in Pain Management: Limitations and Prescribing Constraints
Aboubacar Sekou Kaba1,*, Mohamed Réda Sefrioui2, Khaoula Lemacha1, Abdessamad Karroum1, Belhachmi Adil3, Ali chefchaouni1, Soufiane Derraji1
1Laboratory of Pharmacology-Toxicology, Faculty of Medicine and Pharmacy of Rabat, Mohamed V University of Rabat
2Laboratory of Medicine Sciences, Biomedical and Biotechnological Research, Faculty of Medicine and Pharmacy of Casablanca, Hassan II University of Casablanca
3Neurosurgery Department, Military Training Hospital Mohamed V, Rabat
Received Date: 21/05/2022; Published Date: 07/06/2022
*Corresponding author: Aboubacar Sekou Kaba, Resident in clinical pharmacy, Mohamed V Military Training Hospital of Rabat, Faculty of Medicine and Pharmacy, Mohamed Vde Rabat University, Morocco
Summary
Objective: the main objective of this study, which aims to highlight the difficulties encountered by any prescriber in the management of pain in the third level, and to determine the constraints of prescribing analgesics belonging to table B.
Methods: This is a retrospective study of prescribers of narcotic analgesics in the management of third-level pain. A questionnaire was submitted to volunteer physicians prescribing major analgesics during the period from October to November 2020.
Results: Over a period of 2 months, 100 questionnaires were collected from physicians prescribing morphine analgesics. For the storage of this type of so-called narcotic drugs, 74% of the participants judged that their storage was secure, against 20% who found it not secure. On the other hand, stock management seemed easy for 25 participants and always fluid for 16, while 46 doctors complained about the cumbersome abundance of documents.
Conclusion: Our results showed that narcotics are important in pain management, especially in palliative care. Several alternatives to drug treatment can be considered, but unfortunately, analgesics are the main tool that comes first for any pain, which requires health care workers to deepen their understanding of pain and its treatment. For 32 participants, the problem was mainly repeated stock-outs.
Keywords: Physician; Narcotics; Care; Pain; Analgesics
Introduction
Pain management has made considerable progress over the past decades. The range of drugs available has evolved rapidly and almost exponentially, particularly for strong opioids. The long-term continuation of these treatments is sometimes necessary, which then frequently leads to pharmacological tolerance phenomena and a risk of withdrawal symptoms, still called pharmacological dependence to prescription opioids [1,2].
The use of morphine for chronic pain has increased significantly in North America and variably in Europe. This increase has particularly affected patients with chronic non-cancer pain. The number of overdose deaths related to this prescription has increased in parallel [3].
The dispensing of narcotic drugs at the pharmacy is based first on a regulatory analysis of the prescription to verify whether the prescriber has the right to prescribe this type of drug, whether the prescription is valid with regard to the date of prescription, and whether it is secure and correctly written. Following this analysis, a succession of administrative tasks must be performed [4].
The physician has a great deal of freedom to prescribe. He can choose the most appropriate therapy for his patient or his professional use. However, the prescription of some narcotic drugs is reserved to certain doctors.
The dental surgeon can prescribe all the acts, products and services necessary for the practice of dentistry, including narcotic drugs for his patients or his professional use. The prescription of opiates as analgesics is complicated, from a legislative point of view. It involves problems, constraints and limitations that make their prescription difficult [4].
The midwife is subject to a double limitation: she can only prescribe certain drugs and products and only to the patients to whom she provides care (a woman or her child). Among the narcotic drugs, she can only prescribe morphine hydrochloride in the form of 10 mg injectable ampoules, within the limit of two ampoules per patient or for her professional use [4].
The veterinarian has the right to prescribe veterinary medicine, a right that is very extensive since he can, in certain cases, prescribe human drugs, including narcotics. [4]. It is forbidden to prescribe a narcotic drug for a treatment longer than 28 days, which can be reduced to 7 or 14 days [4].
The treatment of chronic non-cancer pain (CNCP) is not a validated indication for all strong opioids and may expose patients to an unfavorable benefit/risk ratio. In 2004, the French National Agency for the Safety of Medicines and Health Products (ANSM) published an update on the proper use of strong analgesics in this type of pain: at that time, of the strong analgesics available, only morphine could be used in CNCP. Since 2008, transdermal fentanyl is also indicated in DCNC [5].
In 2011, a World Health Organization (WHO) recommendation reiterated the importance of patient access to internationally controlled drugs, especially those indicated for cancer pain [6].
Hospitals that manage cancer patients are sooner or later confronted with the prescription and management of Patient-Controlled Analgesia (PCA). The prescription of these PCAs requires indispensable attention on the part of the prescribing physicians to avoid errors in equivalence, dosage, rate and concentration. Patient-Controlled Analgesia (PCA) is a major therapeutic tool in algology, especially in the field of oncology. They allow the necessary doses of analgesics to be adapted as accurately as possible and give the patient considerable autonomy in the management of his treatment and his pain [7].
A study published in 2016 and conducted in 214 countries showed an increase in the global consumption of opioid analgesic drugs between 2001/2003 and 2011/2013. However, this consumption is very unevenly distributed among different regions of the world [8].
In an article recently published in the September 2015 issue of the Flyer, Drs. Philippe Poulain and Xavier Aknine reminded us that the goal of relieving patients' pain should not be overshadowed. Whether the patients are already dependent on opioids or at risk of becoming so, inadequate pain management leads to anxiety, avoidable suffering, and the risk of a break in follow-up. In addition, it may result in self-medication or 'medical shopping', which is even more dangerous for the health of patients [9].
The prescription of opiates as analgesics is a major public health problem given the constraints associated with writing a secure prescription. In France, the fight against chronic pain has been the subject of 3 successive plans in 1998, 2002, and 2006. Chronic pain is also a public health problem. Its prevalence of 31.7% (according to the STOPNEP study) makes it one of the primary reasons for medical consultation [10].
Hence the major objective of this study, which aims to highlight the difficulties encountered by any prescriber in the management of third-level pain, and to determine the constraints of prescribing analgesics belonging to table B.
Materials and Method
This is a retrospective study of prescribers of narcotic analgesics in the management of third-level pain. A questionnaire was submitted to volunteer physicians prescribing major analgesics during the period from October to November 2020. It aims to exploit the constraints and limitations that hinder the prescription of table B drugs and the proper management of pain. Excluded from the study were physicians prescribing level I and level II analgesics to questionnaires at the Military Hospital of Instruction Mohammed V - Rabat, University Hospital Rabat-Salé, Hospital of Specialties - Rabat, some clinics and offices in the Rabat-Salé region. The data collected were recorded on the attached data sheet and were computerized and statistically analyzed using Excel.
Results
Over a 2-month period, 100 questionnaires were collected from physicians prescribing morphine analgesics. Of these, 56% were specialists, 24% were general practitioners, and 20% were university doctors (Figure 1). 52% of these physicians have less than 5 years of practice, 16% have less than 10 years, while 32% have been practicing for more than 10 years up to 20 years (Figure 2).
QUALITY OF THE PRESCRIBER

Figure 1: Quality of the prescriber.
Years of Service

Figure 2: Years of practice.
Distribution of Specialties

Figure 3: Distribution of specialties.
Narcotic analgesics in pain management
In the analgesic management of third-tier pain, more than 60 physicians prescribe strong opioids, weak opioids, or both together, 48 physicians prescribe non-opioid analgesics. For major analgesics, generally morphine and fentanyl and their derivatives are the most prescribed.
Analgesic Management of Pain Level Three
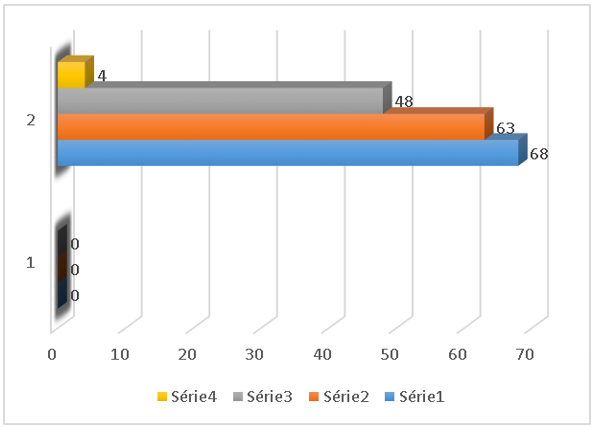
Figure 4: Graphical representations of analgesics prescribed by study participants in the management of level three pain.
Available Central Analgesics

Figure 5: Most prescribed major analgesics.
The most commonly considered route of administration in the analgesic management of third level pain is the parenteral route, followed by the enteral route, and finally the epidural route or other routes.
Most Likely Routes of Administration
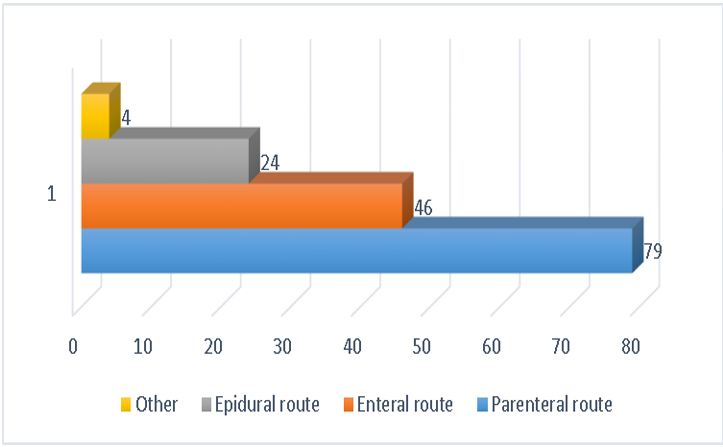
Figure 6: Graphical representation of the routes of administration of the analgesics most commonly considered in pain management by study participant.
For the storage of this type of so-called narcotic drugs, 74% of the participants consider that their storage is secure, against 20% who find it not secure (Figure 7). On the other hand, stock management seemed easy for 25 participants and always fluid for 16, while 46 doctors complained about the cumbersome abundance of documents. For 32 participants, the problem was mainly repeated stock-outs (Figure 8).
Storage of Narcotics
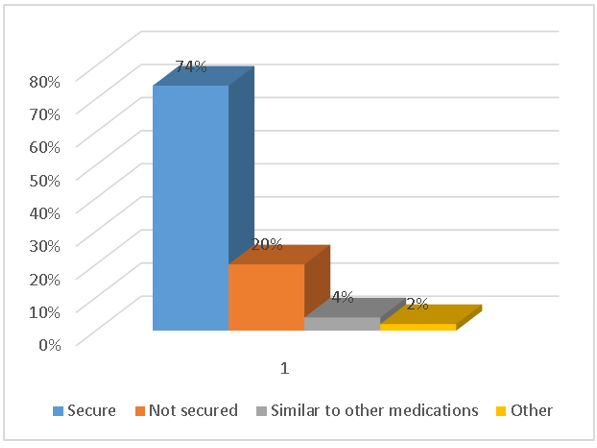
Figure 7: Drug storage.
Stock Management of Narcotics

Figure 8: Narcotics inventory management from the perspective of study participants.
Prescription materials
Concerning the prescription supports for narcotic products, the majority of the prescribers qualify them as necessary, exactly 68 doctors. 12 others think that they are unavoidable (Figure 9). Eight doctors think that these supports are not really necessary. Among these opinions, there are those who find beside that these documents limit the prescription of narcotics. When asked about the availability of the counterfoil books, for 16% of the prescribers these documents are always available, while this is not the case for the rest. They are not always available for 66% of prescribers, and not available for the remaining 18% (Figure 10).
Nececity of the Prescription Media for Narcotics
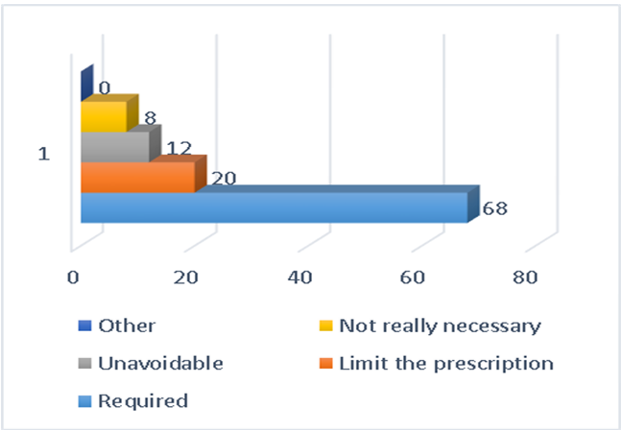
Figure 9: Graphic representations of the necessity supports prescription of narcotics.
Availability of Counterfoil Books
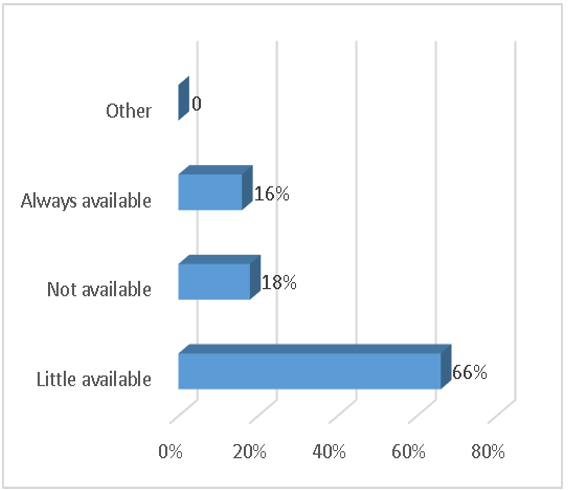
Figure 10: Availability of narcotic prescribing materials for prescribers participating in the study.
For the traceability of the prescription of narcotics, only 29 cases that find it always reliable and 24 that find it always fast. 21 others think that it is not always fast. While 48 doctors find that this traceability is not always reliable (Figure 11).
Traceability of Drug Prescription

Figure 11: Graphical representation of physicians' judgment on prescription traceability.
Legislation regarding the prescription of narcotics
The legislation concerning the prescription of narcotics is apparently complex and limiting for the majority of the participants in the study, in fact for 57%, only 33% find it flexible, and the other 10% preferred not to comment (Figure 12).
Legislation on the Prescription Of Narcotics

Figure 12: Participants' views on drug prescription legislation.
These prescribing procedures, dictated by the legislative standards of medical law, limited the prescribing of narcotics for 65 participants, appeared to be very time-consuming for 36 participants, and even caused 16 participants to abandon narcotic pain management (Figure 13).
Modalities of Prescription
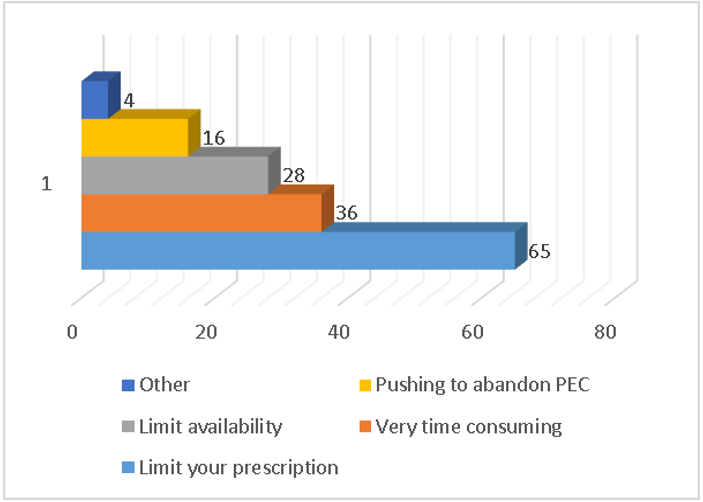
Figure 13: Participants' Views on Prescribing Arrangements for Narcotics.
Discussion
As detailed in the results, narcotic analgesics occupy a large space in the drug arsenal of pain management. However, despite their remarkable importance, the prescription of narcotics encounters several limitations and constraints, ranging from the supports necessary for the prescription of this particular type of medication, to the legislation relating to this prescription. Compared to their necessity, the counterfoil books are hardly available, and this is on the one hand. On the other hand, all the legal norms defining the regulation of prescription of narcotics complicate the latter to the point of limiting it, or even pushing the prescribers to abandon this therapeutic family of drugs.
Pain management
Analgesic medication prescribed for intense and intolerable pain is clearly dominated by strong or weak opioids, according to more than 60% of the physicians participating in the study. However, this was not the case in a survey conducted by Dr. David Harel and his team in 18 hospitals of the regional pain network in Basse-Normandie, on "the management of acute pain". In this study, second and third level analgesics (weak opioids and strong opioids) represent 21% of the types of analgesics used in emergencies, knowing that 34% of patients arriving in emergencies suffer from intense or even intolerable pain. Thus, in another study carried out by doctor Doina Roscoulet among general practitioners in Val-de-Marne in Paris, the use of morphine in the therapeutic arsenal remains "rare" for 57% of prescribers and "exceptional" for 11%. While it is "usual" for only 30%, and only 2% declare to prescribe morphine "very frequently". The same study shows that the major indication for morphine analgesics is in 97% of cancer pain. The use of morphine products is limited because most patients benefit from a non-drug analgesic treatment, or they have the pain automatically relieved after etiological treatment. In the same interests, several therapeutic alternatives to the medical prescription of morphinics were detailed in the research of Déborah Charbonnier carried out in 2013 in the Faculty of Medicine of Nice in France, concerning an "evaluation of the difficulties encountered and the information delivered to patients when prescribing second stage analgesics in general medicine".
Availability of central analgesics
Morphine (96%) and fentanyl (80%) and their derivatives are the drugs most frequently encountered when asked about the availability of central analgesics. The same results were found by Michel Galinski's team in the telephone survey they conducted to "evaluate the practices of physicians in mobile emergency and resuscitation services (SMUR) in France concerning the management of severe acute pain in adults in out-of-hospital medicine". Morphine was available in these mobile hospital units for 93% of the doctors questioned, fentanyl for 79%, nalbuphine for 64%, and sufentanil for 26%.
Routes of administration considered
The routes of administration most considered by the prescribing physicians participating in the study were parenteral for 79 physicians, followed by enteral for 46 physicians, and finally the epidural route for 24 physicians. Contrary to the results found by Doina Roscoulet, in her study in Val-de-Marne, which show that the injectable parenteral route is considered by only 3% of general practitioners, while the routes dominating the prescriptions by a rate of 97% are those enteral extended release (37%) or immediate (29%) next to the transdermal route (31%). Several explanations can make this discrepancy clearer, first of all the quality of the prescriber; our study reserved only 20% of places for general practitioners, whereas the comparative study only concerned general practitioners. Thus, the availability and accessibility of the different galenic forms of narcotics can be largely modified between France and Morocco. Finally, hospital care differs from outpatient care, which may be the most concerned by the study of D. Roscoulet.
Availability and necessity of prescription supports
In his article "Utilité et acceptabilité du carnet à souches" (Usefulness and acceptability of the counterfoil book) published in 1998 in "La Revue du Praticien" (The Practitioner's Review), Pierre Poloméni pointed out that the prescription of narcotics is low, having as a data that the orders on the counterfoil books are not very important in relation to the number of practising doctors. But without being able to demonstrate the obvious link between the existence of the counterfoil book and the low level of prescription. This suggested that the simple removal of this tool will not cause significant changes in physician practices, but it may cause other difficulties. The same results were shared with the above study in terms of the availability of counterfoil books; judged "not very available" by 66% of the physicians, 18% consider them "unavailable", and only 16% who find them "always available". But in terms of the necessity of these books, they are "necessary" for 68 doctors among those questioned, and "unavoidable" for 12 others, only 8 doctors who do not find them really necessary.
Traceability of narcotics prescriptions
Mathieu Guerriaud in his article "Délivrance des médicaments stupéfiants" published in 2019 in the journal "Actualités Pharmaceutiques" discussed the importance of ensuring good traceability of narcotics prescriptions, while mentioning the difficulty of maintaining good practices of their delivery at the pharmacy. The latter has a framework that may appear restrictive, but is very important to protect both society from the dangers of these drugs, and health professionals from any attempt at fraud. In this interest, a succession of administrative tasks must be carried out to ensure maximum traceability. Among the physicians participating in our study, 48% doubt the reliability of the traceability of the prescription of narcotic drugs, there was among them a lack of accurate information on this subject. This suggests the need for better training of staff on all aspects of pain management using narcotics. In her research on morphine prescribing, Doina Roscoulet asked about the availability of health workers to participate in more specific training for pain management, and 57% of the physicians responded that they were interested in participating.
Legislation and Prescribing Practices for Narcotics
When asked about the legislation regarding the prescription of narcotics, more than half of the participants in the study shared the same opinion. 57% of the physicians found this legislation complex and limiting for the prescription of morphine products, 10% refused to comment, and only 33% found it flexible. The complexity of the regulations further complicates the prescribing modalities, which were judged to be limiting by 65 physicians, very time-consuming by 36 physicians, and 16 physicians think that these modalities even lead to abandoning the management of pain by narcotic products.
In the study carried out by Doina Roscoulet in Val-de-Marne, one of the main obstacles to prescribing morphine was the cumbersome nature of this operation, which was considered difficult by 36% of the respondents, despite the abolition of counterfoil books and the introduction of secure prescriptions since 1999. This last detail confirms Pierre Poloméni's view that the abolition of counterfoil books will not change much in the complexity of prescribing narcotics.
Conclusion
Our results showed that narcotics play an important role in pain management, especially in palliative care. Several alternatives to drug treatment can be considered, but unfortunately, analgesics are the main tool for pain management, which requires health workers to deepen their understanding of pain and its treatment through targeted and specialized training. The burdensome nature of opioid prescribing is well recognized by practitioners around the world, but it is necessary and should never be exceeded, as it is the inevitable result of strict and detailed regulatory oversight to control these specific products. However, there is no excuse for avoiding their prescription just because it is burdensome.
Declaration of interests: The authors declare that they have no interests.
References
- Rolland B, Bouhassir D, Authier N, et al. Mésusage et dépendance aux opioïdes de prescription : prévention, repérage et prise en charge ; La Revue de médecine interne,
- Alain S. Le fossé mondial de la douleur : déséquilibre entre Nord et SUD ; Douleurs,
- Adam F. Mauvais usage des morphiniques en analgésie. Le Praticien en anesthésie réanimation, 2017
- Guerriaud M. Délivrance des médicaments stupéfiants ; Elsevier Masson SAS,
- Delinger F, Patrick G, Céline E, Laure P, Hélène P. Opioïdes forts dans le traitement des douleurs chroniques non cancéreuses : analyse rétrospective de patients pris en charge pour un sevrage ; Thérapie,
- Marie B, Joëlle PP, Ghada MS, Amélie D. Évolution de l’offre de médicaments stupéfiants en médecine ambulatoire en France : aspects réglementaires et stratégies de mise sur le marché (2003—2017) ; therapie, 2018.
- Laurent L, Valérie DC, Mickael D, Nathalie L, Marie NF, Fabrice L. Prescription et gestions des PCA de stupéfiants : un outil pour ne plus se tromper et gagner du temps ; douleurs, 2012.
- Nadia F, Mati N, Henda R, Yacine H, Alain S. Accès aux analgésiques opioïdes pour les douleurs cancéreuses : des inégalités majeures — la situation en Afrique; douleurs, 2017.
- Patrick S. Opioïdes et risques addictifs, comment les prévenir ? Questions posées aux Dr S. Robinet, Dr C. Lucas, Dr J. Bernard et Pr N. Franchitto ; Douleurs,
- Leila BVDK, Marc S. Impact de la prise en charge podo-posturale dans le cadre de 2 types de douleurs chroniques débutantes au niveau de la plante des pieds : la douleur en rapport avec la neuropathie des petites fibres et la douleur en rapport avec la maladie rhumatismale.
- Ollivier C, Bernard L, Gentili M, Règles de prescription des morphiniques de palier 3 en ambulatoire, Le Courrier de l’algologie, 2007.
- Beloeil H. Anesthésie sans opiacés. Société française d'anesthésie et de réanimation (Sfar) Anesth Reanim. Elsevier Masson SAS, 2018.

