Essential hypertension pathogenesis: Merely a sympathetic hyperactivity? A series of 10 patients
NABIL LAKTIB ; HOUDA.MOKHLISS ; ILYASSE ASFALOU ; NAJAT MOUINE ; AATIF.BENAYASS
CDepartment of Cardiology Intensive Care Unit, Cardiology Center of the Military Teaching Hospital Mohammed V, Rabat, Morocco.
Department of non-invasive cardiac explorations, Cardiology Center of the Military Teaching Hospital Mohammed V, Rabat, Morocco.
Head of non-invasive cardiac explorations department, Cardiology Center of the Military Teaching Hospital Mohammed V, Rabat, Morocco.
Head of clinical cardiology department, Cardiology Center of the Military Teaching Hospital Mohammed V, Rabat, Morocco.
Head of Cardiology Center of the Military Teaching Hospital Mohammed V, Rabat, Morocco
Received Date: 28/03/2022; Published Date: 13/04/2022
*Corresponding author: Nabil Laktib, Department of Cardiology Intensive Care Unit, Cardiology Center of the Military Teaching Hospital Mohammed V, Rabat, Morocco
Abstract
Essential, idiopathic or primary hypertension is a hypertension form with no known etiology. Several studies have demonstrated that the autonomic system is involved in the pathogenesis of many cardio-vascular diseases such as hypertension. The aim of our work is to describe the autonomic profile of patients with hypertension and discuss an eventual relationship between hypertension and sympathetic hyperactivity. This is a prospective study that included 10 patients admitted for essential hypertension in the autonomic nervous system unit of cardiology center Mohammed V Military Hospital Rabat, Morocco. All of them had cardiovascular autonomic testing including Deep Breathing, Hand-Grip, Mental Stress and orthostatic tests. The average age of patients was 62.1 years. The sex ratio was 1. At rest, systolic blood pressure was146.8 mmhg and diastolic blood pressure was 82 mmhg. The autonomic nervous testing showed a high alpha peripheral sympathetic response at 21.1 %, a normal alpha central sympathetic response at 10.1%, a low beta central sympathetic response at 8.5% and a vagal deficiency at 26.1%. This study showed a peripheral alpha-adrenergic hyperactivity in most patients which may suggest a possible association between essential hypertension and alpha adrenergic overdrive.
Keywords: Primary hypertension · Adrenergic overdrive · Pathogenesis
Introduction
Hypertension (HT) is defined as the blood pressure level at which the benefits of treatment unequivocally outweigh treatment risks as documented by clinical trials [1]. However, cut-offs have been established for clinical practice. HT can be defined as office systolic blood pressure values ≥140 mmHg and/or diastolic blood pressure values ≥90 mmHg [2]. Essential or idiopathic or primary hypertension is a hypertension form that is the result of no medical condition or no known etiology. Several studies looked for an eventual cause of essential hypertension. The most popular theory is the role of sympathetic hyperactivity in essential HT pathogenesis. The aim of our work is to describe the autonomic profile of patients with HT and discuss an eventual relationship between HT and sympathetic hyperactivity.
Patients and Methods
This is a prospective study including 10 patients with essential HT conducted at the autonomic nervous system unit of cardiology center Mohammed V Military Hospital of Rabat. The autonomic testing included deep breathing (DB) for vagal activity and Hand Grip (HG) for peripheral alpha adrenergic activity assessment, Echo Stress (ES) for central alpha- and beta-adrenergic activity, the alpha-adrenergic activity is assessed through blood pressure variability.
Results
Table 1: Patients age.
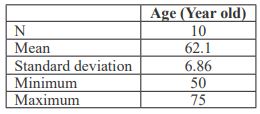
Table 2: Patients sex.
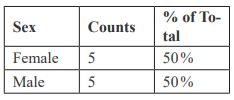
Table 3 : Autonomic tests results.

Discussion
Primary HT is the most prevalent cardiovascular disease worldwide. It is termed as a silent killer as it leads to lethal complications even in asymptomatic patients. Blood pressure regulation mechanisms are nowadays very well known. The autonomic nervous system plays a critical role in vascular homeostasis regulation [3]. Neurological regulation of blood pressure and flow depends on the cardiovascular centers located in the medulla oblongata. It involves baroreceptors reflexes located within blood vessels and heart chambers responding to the degree of stretch caused by the blood flow.
When blood pressure increases, baroreceptors trigger parasympathetic stimulation. Therefore, cardiac output decreases. Sympathetic stimulation of the peripheral arterioles will also decrease, resulting in vasodilation causing blood pressure decrease [4]. In the other hand, when blood pressure drops too low, the rate of baroreceptors firing decreases. This triggers an increase in sympathetic heart stimulation, leading to cardiac output increasing [4]. It also triggers sympathetic stimulation of the peripheral vessels, resulting in vasoconstriction hence rising blood pressure.
Sympathetic hyperactivity may be involved in primary hypertension. The purpose of this study was mainly to evaluate sympathetic activity when performing autonomic tests in patients with primary HT. We investigated whether sympathetic activity is further increased in individuals with hypertension and found that hypertensive patients had a significantly higher sympathetic response to peripheral stimulation and a significantly lower parasympathetic response. However, central sympathetic response was within normal range. In Benjeloun et al. Study [5], both central and peripheral response were higher in patients with HT compared to normal patients whereas parasympathetic response was low. Therefore, HT pathogenesis may be a combination of a sympathetic overdrive and a low parasympathetic response.
The discovery of an autonomic disorder in hypertensive patients not only helps to identify the mechanisms of HT, but also to understand the pathophysiology of the cardiovascular system implication to help guide therapeutic decision as it is desirable to develop antihypertensive treatment by acting as well on the sympathetic overdrive, as already mentioned by some authors [6-8].
Conclusion
Our study showed a peripheral alpha-adrenergic hyperactivity and a low parasympathetic activity in most hypertensive patients. That suggests the role of autonomic system imbalance in HT pathogenesis due mostly to adrenergic overdrive.
Funding: No funding was received for conducting this study.
Author’s contribution: All authors contributed to the final manuscript.
Competing interests: None of the authors have conflicts of interest.
Compliance with ethical standards.
References
- Williams B, Mancia G, Spiering W, et al. ESC/ESH Guidelines for the management of arterial hypertension. European Heart Journal, 2018 ; 39(33) : pp.3021-3104.
- Journal of Hypertension. European Society of Hypertension European Society of Cardiology guidelines for the management of arterial hypertension*, 2003; 21(6): pp.1011-1053.
- Franklin S, Khan S, Wong N, Larson M, Levy D. Is Pulse Pressure Useful in Predicting Risk for Coronary Heart Disease? Circulation, 1999; 100(4): pp.354-360.
- Raven P, Chapleau M. Blood pressure regulation XI: overview and future research directions. European Journal of Applied Physiology, 2014; 114(3): pp.579-586.
- Benjelloun H, Aboudrar S, Jroundi I, Benjelloun-Bennani H, Coghlan L, Benomar M. Les réponses sympathiques dans l’hypertension artérielle essentielle. Annales de Cardiologie et d'Angéiologie, 2009; 58(3) : pp.139-143.
- de Champlain J, Karas M, Nguyen P, Cartier P, Wistaff R, Toal C, et al. Different effects of nifedipine and amlodipine on circulating catecholamine levels in essential hypertensive patients. Journal of Hypertension, 1998; 16(9): pp.1357-1369.
- Fotherby M, Iqbal P. Antihypertensive therapy and orthostatic responses in elderly hospital in-patients. Journal of Human Hypertension, 1997; 11(5): pp.291-294.
- Rabbia F, Martini G, Genova G, Milan A, Chiandussi L, Veglio F. ANTIHYPERTENSIVE DRUGS AND SYMPATHETIC NERVOUS SYSTEM. Clinical and Experimental Hypertension, 2001; 23(1-2): pp.101-111.

