A Rare Tumor in a Rare Location: Ganglioneuroma
Faisal El mouhafid*
Department of Visceral Surgery, Mohammed V Military Teaching Hospital, Morocco
Received Date: 14/02/2022; Published Date: 24/02/2022
*Corresponding author: Faisal El mouhafid, Department of Visceral Surgery, Mohammed V Military Teaching Hospital, Ryad, Rabat, Morocco
Abstract
The ganglioneuroma is a rare benign tumor Neuronagliomas of the adrenal gland are a rare pathology. Therefore, this case will be of interest to urologists, surgeons, oncologists and pathologists. located in the adrenal gland (20%), along the sympathetic chain and particularly in the posterior mediastinum (40%) and the retroperitoneum (30%). The ganglioneuroma poses a positive diagnostic and therapeutic problem.
We report the case of a patient aged 48 admitted for pain in the right hypochondrium. He had no significant past medical or surgical history. a physical examination there were no noticeable findings except for mild tenderness and a mass on palpation. he underwent abdominal CT, which showing a relatively homogenous right adrenal tumor measuring. Endocrine work-up including urine catecholamine and cortisol levels was normal. Due to the tumor size and with consideration of the differential diagnosis of a malignant lesion we elected to operate on the patient. A right adrenalectomy was performed, with no related complication. The final histopathologic report revealed adrenal ganglioneuroma. Although benign; the ganglioneuroma can present malignant aspects, in particular CT scans and biological that can mislead the clinician, so histology remains the examination of choice for making the diagnosis.
Keywords: Tumor; Adrenal glands; Gangioneuroma
Introduction
Ganglioneuromas are benign and well-differentiated tumors of the sympathetic nervous system. They arise from the great sympathetic chains extending from the base of the skull to the neck, mediastinum, retroperitoneum and adrenal glands [1,2]. Ganglioneuromas of the adrenal gland are extremely rare. These tumors affect preferentially young people with the majority reported to occur before the age of 20. These tumors are usually asymptomatic and, in the majority of cases, detected incidentally. When symptomatic, they present with non-specific symptoms related to their size or location with compression of neighbouring structures [3]. GN’s are usually hormonally inactive, some of them secrete catecholamines. Symptoms like virilisation, hypertension and diarrhea may develop as a result of mixed hormone secretion. The imaging characteristics of adrenal GN are variable and some are very similar to other adrenal tumors such as Adrenocortical Carcinoma (ACC) and pheochromocytoma, a fact that is crucial in the clinic [4,5]. Therefore, it is generally challenging to obtain a precise differential diagnosis of adrenal GN prior to surgery. Histopathological examination is currently the only tool to definitely diagnose this pathology.
Case Report
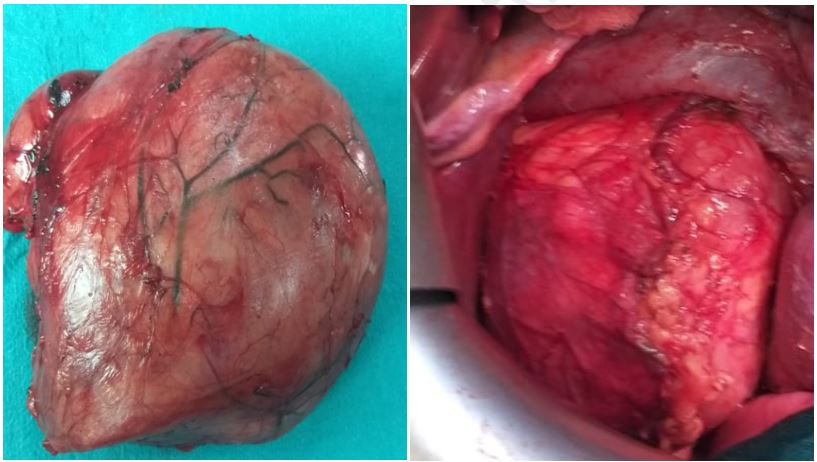
A 48-year-old male admitted to our hospital for pain in the right hypochondrium. He had no significant past medical or surgical history. a physical examination there were no noticeable findings except for mild tenderness and a mass on palpation. The results of laboratory tests were all found to be within the normal ranges. Because of his symptoms, he underwent abdominal CT, which showing a relatively homogenous right adrenal tumor measuring 20*18*11 cm. Endocrine work-up including urine catecholamine and cortisol levels was normal. Due to the tumor size and with consideration of the differential diagnosis of a malignant lesion we elected to operate on the patient. exploratory laparotomy was performed to allow a definite diagnosis. A right adrenalectomy was performed, with no related complication. The surgical specimen was an elastic tumor, measuring 20×18×11cm (Figure 1 ). On microscopy, the section showed irregular proliferation of spindle-shaped cells and scattered mature ganglionic cells with dystrophic changes and focal lymphocytic infiltration. No evidence was found for the malignancy.
An immunohistochemical examination showed positive staining of the ganglion and Schwann cells for S-100, vimentin and synaptophysin. The final histopathologic report revealed adrenal ganglioneuroma (Figure 2). Postoperative recovery was uneventful. No recurrence was detected during the one-year follow-up visits.

Discussion
GN is a rare, differentiated and benign tumor arising from primordial neural crest cells that form the sympathetic nervous system [6]. On histology, it is composed of mature Schwann cells and ganglion cells with fibrous stroma [7,8]. GN is a member of a group of neurogenic
tumors group that includes ganglioblastoma and neuroblastoma. It differs from other neurogenic tumors in its benign potential [6].
Although GN is generally considered to occur more frequently in young people, some recent studies have shown that it may also be seen between the ages 40 and 50 [4,9]. GN is most commonly found in the posterior mediastinum and retroperitoneum, and the involvement
of the adrenal gland is relatively rare (21%) [10]. Adrenal GN is usually regarded as having silent hormonal functions and therefore can be asymptomatic. Occasionally, composite tumors with pheochromocytoma are seen and they, rarely, can secrete cortisol and androgen [11,12].
Additionally, Geoerger et al. reported that up to 30% of patients with GN had elevated plasma and urinary catecholamine levels but that patients were rarely found to have symptoms of catecholamine excess [7]. By contrast, Koch et al. reported the case of a patient with a GN that was positive for vasoactive intestinal peptide, which is the product of ganglion cells [13]. Patients with vasoactive intestinal peptide-positive tumors such as GN and neuroblastomas may not have any symptoms or signs of vasoactive intestinal peptide secretion [14]. GN can also produce and secrete other hormones, such as testosterone, indicating the pluripotency of its precursor cell.
The differential diagnosis of an adrenal mass comprises a long list including adenoma, myelolipoma, cyst, lipoma, pheochromocytoma, adrenal cancer, metastatic cancer, hyperplasia and tuberculosis [7-8].
The macroscopic characteristics of adrenal GN are an encapsulated mass with a firm consistency and a solid, homogeneous, grayish-white cut surface. Histopathological examination shows mature ganglion cells and Schwann cells among a fibrous stroma. Using microscopy, they can be classified in two main groups: mature and maturing.
The mature type is composed of mature Schwann cells, ganglion cells and perineurial cells, whereas the maturing type consists of cells with different maturation levels, ranging from mature cells to neuroblasts with a similar stroma. According to immunohistochemical analysis, GN are characterized by reactivity for S-100, vimentin, synaptophysin and neuronal markers [12].
The imaging characteristic of adrenal GN on CT and MRI have been well described, the precise diagnosis of adrenal GN using radiological evaluation prior to surgery is difficult. Qing et al. reported that the misdiagnosis rate of adrenal GN on CT and MRI before
surgery is 64.7% [4]. intratumoral calcification has been determined in 0% to 29% of the cases [4,5].
PET scans can help complete the picture obtained by CT and MRI when making a differential diagnosis between adrenal GN and ACC or metastasis. One study reported that all cases of ACC had a SUV of 3.0 or higher, and that the sensitivity and specificity to distinguish
ACC from adenoma were 100% and 98%, respectively [15,16]. In another review of four patients with adrenal GN, the SUVs were between 1.5 and 2.9 [9].
Even though a lesion size greater than 4.5cm seems to be a strong predictor of malignancy, this is not correctly confirmed by histologic evaluations. In our patient, although his tumor was larger than 18 cm, pathology confirmed a benign tumor. Recent studies recommended that nonsecretary adrenal incidentalomas larger than 6cm or with suspicious features of malignancy on imagining procedures should be treated by adrenalectomy [6-17].
There is no medical treatment for such tumors. GN, although benign, can grow aggressively. Patients treated surgically for a benign neurogenic tumor have an excellent prognosis. Papavramidis et al. reported that adrenal GN should be respected by adrenalectomy, whereas retroperitoneal GN can be resected without adrenalectomy [18]. The laparoscopic adrenalectomy becoming the procedure of choice for the surgical removal of a vast majority of small sized (<6cm) adrenal lesions [6,7,17]. The prognosis for an adrenal GN following surgical resection is good.
Conclusion
References
- Linos D, Tsirlis T, Kapralou A, et al. Adrenal ganglioneuromas: incidentalomas with misleading clinical and imaging features. Surgery, 2011; 149: 99–105.
- Sucandy I, Akmal YM, Sheldon DG. Ganglioneuroma of the adrenal gland and retroperitoneum: a case report. N Am J Med Sci, 2011; 3: 336–338.
- Hayes FA, Green AA, Rao BN. Clinical manifestation of ganglioneuroma. Cancer, 1989; 63: 1211–1214.
- Qing Y, Bin X, Jian W, Li G, Linhui W, Bing L, et al. Adrenal ganglioneuromas: a 10-year experience in a Chinese population. Surgery, 2010; 147: 854–860.
- Maweja S, Materne R, Detrembleur N, de Leval L, Defechereux T, Meurisse M, et al. Adrenal ganglioneuroma. A neoplasia to exclude in patients with adrenal incidentaloma. Acta Chir Belg, 2007; 107: 670–674.
- Joshi VV. Peripheral neuroblastic tumors: pathologic classification based on recommendations of international neuroblastoma pathology committee (modification of shimada classification). Pediatr Dev Pathol, 2000; 3: 184–199.
- Geoerger B, Hero B, Harms D, Grebe J, Scheidhauer K, Berthold F. Metabolic activity and clinical features of primary ganglioneuromas. Cancer, 2001; 91: 1905–1913.
- Enzinger FM, Weiss SW. Ganglioneuroma. In Soft Tissue Tumors 3rd edition. St Louis: Mosby-Year Book, 1995: 929–964.
- Rhondeau G, Nolet S, Latour M, Braschi S, Gaboury L, Lacroix A, et al. Clinical and biochemical features of seven adult adrenal ganglioneuromas. J Clin Endocrinol Metab, 2010; 95: 3118–3125.
- Jain M, Shubha BS, Sethi S, Banga V, Bagga D. Retroperitoneal ganglioneuroma: report of a case diagnosed by fine-needle aspiration cytology, with review of the literature. Diagn Cytopathol, 1999; 21: 194–196.
- Charfi S, Ayadi L, Ellouze S, Ghorbel R, Khabir A, Gouiaa N, et al. Composite pheochromocytoma associated with multiple endocrine neoplasia type 2B. Ann Pathol, 2007; 28: 225–228.
- Sasaki S1, Yasuda T, Kaneto H, Otsuki M, Tabuchi Y, Fujita Y, et al. Large adrenal ganglioneuroma. Intern Med, 2012; 51: 2365–2370.
- Koch CA, Brouwers FM, Rosenblatt K, Burman KD, Davis MM, Vortmeyer AO, et al. Adrenal ganglioneuroma in a patient presenting with severe hypertension and diarrhea. Endocr Relat Cancer, 2003; 10: 99–107.
- Kogner P. Neuropeptides in neuroblastomas and ganglioneuromas. Prog Brain Res, 1995; 104: 325–338.
- Mackie GC, Shulkin BL, Riberio RC, Worden FP, Gauger PG, Mody RJ, et al. Use of [18]F-fluoro-deoxyglucose positron emission tomography in evaluating locally recurrent and metastatic adrenocortical carcinoma. J Clin Endocrinol Metab, 2006; 91: 2665–2671.
- Kulkarni AV, Bilbao JM, Cusimano MD, Muller PJ. Malignant transformation of ganglioneuroma into spinal neuroblastoma in an adult. Case report. J Neurosurg, 1998; 88: 324–327.
- Yamaguchi K, Hara I, Takeda M: Two cases of ganglioneuroma. Urology, 2006; 67: 622. e1-e4.
- Papavramidis TS, Michalopoulos N, Georgia K, Kesisoglou I, Valentini T, Georgia R, et al. Retroperitoneal ganglioneuroma in an adult patient: a case report and literature review of the last decade. South Med J, 2009; 102(10): 1065–1067.

