Localized Guillain Barre Syndrome Associated with Cervical Syringomyelia
Meryem Bouyadmar*, Nabila Chekhlabi, and Nouzha Dini
Sheikh Khalifa International University Hospital, Faculty of Medicine, Mohammed VI University of Health, Casablanca, Moroco
Faculty of Medicine and Pharmacy, Mohammed V University, Rabat, Morocco
Received Date: 05/02/2022; Published Date: 18/02/2022
*Corresponding author: Meryem Bouyadmar, Sheikh Khalifa International University Hospital, Faculty of Medicine, Mohammed VI University of Health, Casablanca, Moroco
Abstract
Guillain-Barré Syndrome (GBS) is an acute inflammatory polyradiculoneuritis responsible, in its typical form, for ascending paralysis that can be life-threatening. It most often occurs following a viral infection rarely following a bacterial infection such as mycoplasma. Syringomyelia is a chronic disease characterized by a cavity that extends longitudinally inside the spinal cord. In this case report, we report one case exhibiting the exceptional association of this syndrome with syringomyelia.
Clinical Case
An 11-year-old child, second of two siblings, from and living in Casablanca, was admitted for paralysis of the right upper limb. The patient's history indicates a known epileptic since the age of 9 and a half without treatment. He underwent a first crisis without tonic fever lasting 10 min, frontal epilepsy on the EEG, and a second tonic-clonic crisis a year before his admission in the hospital with post-critical deficit. The history of the disease goes back to a week before his admission with progressive muscle weakness then total impotence of the right upper limb, headaches, without other signs (no respiratory or digestive signs), all evolving in a context of fever not encrypted. Due to the intensification of headaches and motor deficit despite taking anti-inflammatories by self-medication, the parents consulted a pediatric neurologist with hospitalization in the pediatric department. A general exam was performed and showed that the patient was conscious, hemodynamically and respiratory stable, with a fever of 38.2°, a Glasgow score of 15/15. The Neurological examination showed no stiff neck, normal gait, deep tendon reflex well perceived in the lower limbs, deep tendon reflex abolished to upper limbs, muscular strength rated at 5/5 in both lower limbs and left upper limb, muscle strength at 2/5 in the right upper limb, sensitivity preserved in the right upper limb to pain and heat, no impairment of the cranial nerves or facial paralysis, while the rest of the somatic examination is without anomaly. Additional examinations were performed and showed the absence of encephalic abnormality in his brain MRI, and the collapse of motor response amplitudes in the right upper limb with decrease in these in the left upper limb in his electromyogram to 4 limbs. It showed also the appearance evoking motor axonal polyradiculoneuritis affecting the upper limbs and predominant on the right upper limb (AMAN syndrome), spinal MRI with no Chiari anomaly, cervical syringomyelic cavity extended from C2 to D1, lumbar Puncture Fluid having a slightly cloudy appearance Leukocytes of 39/mm3 , 8% PNN and 92% lymphocytes, and normal chemistry of NFS with Hg 12.1 g/dl, GB of 7580/mm3, platelets of 220000/mm3, negative CRP and procalcitonin, negative hepatitis A, B, C, CMV and EBV serologies, and positive mycoplasma pneumonia serology. The patient was put on an immunoglobulin infusion at a dose of 500 mg/kg for 5 days, macrolide-based antibiotic therapy and regular motor rehabilitation with good clinical progress.
Discussion
Guillain-Barré syndrome and syringomyelia are diseases of different entities. GBS is an acute post-infectious autoimmune disease transmitted by autoantibodies directed against the myelin of peripheral nerves. It is observed at all ages, with equal frequency in both sexes, in all races, without seasonal predominance. Its incidence is approximately 1 case per 100,000 inhabitants. In 2/3 of the patients, one finds, 1 to 3 weeks before the first symptoms, an infectious episode of the upper airways or the digestive tract. The agents most often involved are cytomegalovirus, Epstein-Barr virus, mycoplasma pneumonia and Campylobacter Jejuni. More rarely, GBS can follow a vaccination or a surgical procedure. In its typical form, GBS begins with paraesthesias of the extremities, then rapidly develops paralysis affecting all four limbs. The intensity of the paralysis is variable, ranging from a simple weakness of the lower limbs hampering walking and climbing stairs, to complete quadriplegia with paralysis of the respiratory muscles, requiring emergency respiratory assistance. Osteotendinous areflexia is a hallmark of the syndrome. It begins in the lower limbs, where weakness predominates, then it becomes diffuse (cf. Figure 1). Motor impairment localized to a single limb, such as our case, is very rare. Therefore, we intend to educate treating pediatricians and neurologists about these rare variants of GBS so that these cases are properly diagnosed and treated [2]. The ENMG electro-neuro-myogram shows a drop or even a collapse (cf. Figure 2).
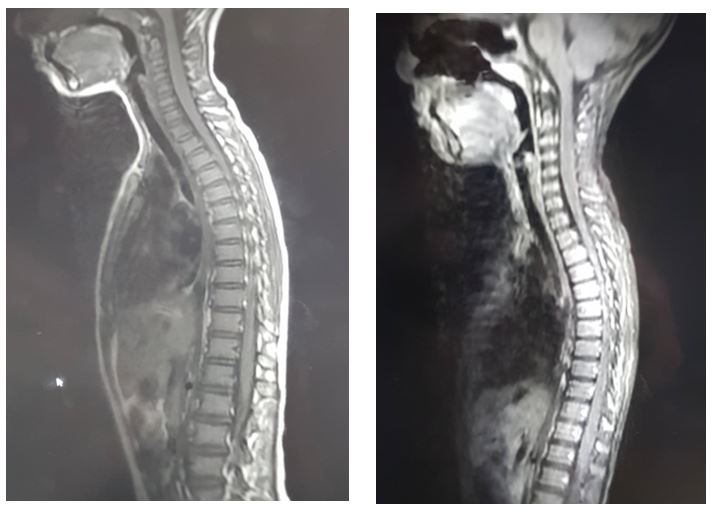
Figure 1,2: Sagittal T1 MRI slices showing the syringomyelic cavity.
Syringomyelia is defined by the presence of an intramedullary fluid formation distributed over at least 2 myelomeres and composed of a fluid identical to cerebrospinal fluid. It is a rare, chronic disease and most often progresses to a severe neurological deficit and dysfunctions through chronic neuropathic pain. Nowadays, given the availability of MRI, we see more and more patients in whom an image of a more or less extensive intramedullary cavity is discovered either incidentally or during various clinical signs, signs and electrophysiological evoking neuropathy including GBS. The association of Guillain Barré syndrome and syringomyelia is exceptional [1]. In the literature, the coexistence of Guillain barré syndrome secondary to a mycoplasma infection and pre-existing syringomyelia has been described in a similar observation in a 6-year-old girl [3]. It is based on the administration of human immunoglobulins with often very good results. Syringomyelic clefts generally do not require surgical treatment unless they are extensive. Despite standard treatment with IVIG or plasma exchange, approximately 20% of severely affected patients remained unable to walk after six months. The prognosis of GBS is difficult to predict due to the wide variations in therapeutic response.
Conclusion
References
- Kim HS, Yun DH, Chon J, Lee JE, Park MH, Han YJ. Syringomyelia coexisting with guillain-barre syndrome. Annals of Rehabilitation Medicine, 2013; 37(5): 745.
- Verma R, Chaudhari TS. Two unusual variants of Guillain-Barre syndrome. Case Reports, 2012, bcr2012007088.
- Vampertzi O, Dalpa E, Vavilis T, Tramma D. Comorbid presentation of syringomyelia and Guillain-Barre syndrome, attributed to mycoplasma, in a 6-year-old female patient. Case Reports, 2018.

