The Autonomic Profile in Postural Orthostatic Tachycardia Syndrome, about 12 Patients
Nabil Laktib*, Halima Benjelloun, Rokaya Fellat
Department of Cardiology, Ibn Sina Hospital, Morocco
Received Date: 31/10/2021; Published Date: 24/11/2021
*Corresponding author: Nabil Laktib, Resident of Cardiology, Assigned to Cardiology Center of Mohammed V Military Teaching hospital, Rabat, Morocco.
Abstract
The postural orthostatic tachycardia syndrome is one of the most common autonomic dysfunctions. Although its clinical presentation may be misleading for the practitioner, it can be easily identified using autonomic tests. Our study included 12 patients with postural orthostatic tachycardia syndrome. Autonomic tests were performed to all those patients. The tests included orthostatic test, echo stress, deep breathing, and hand grip. All subjects had increased central and peripheral beta-adrenergic activity. Alpha adrenergic activity was within normal rage.
Keywords: Postural; Orthostatic; Tachycardia; Syndrome; Autonomic; Profile
Introduction
The postural orthostatic tachycardia syndrome (POTS) is a common autonomic disease, initially described in 1983 [1]. It can be defined as an orthostatic intolerance associated with an excessive tachycardia without orthostatic hypotension which may reduce patient’s functional capacity and impact their quality of life. POTS should be distinguished from isolated orthostatic intolerance, which is a common term including several manifestations due to standing position not fulfilling POTS criteria [2]. This syndrome is a new entity not well known by cardiologists often mistook for other causes of palpitations. It can be easily diagnosed using autonomic tests. The aim of our study is to describe the autonomic profile in POTS.
Material and Methods
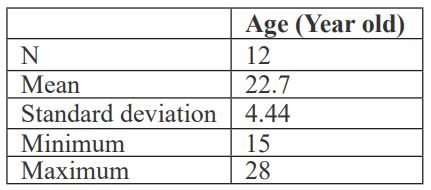
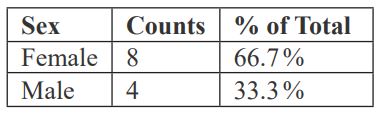
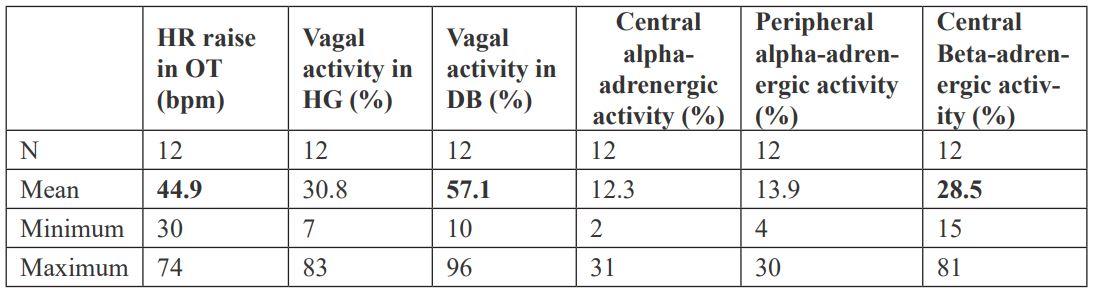
This is a retrospective study including 12 patients with POTS conducted at the Cardiology A departement of Ibn Sina hospital. The autonomic testing included Orthostatic Test (OT) for peripheral beta-adrenergic activity, Echo Stress (ES) for central alpha- and beta-adrenergic activity, Deep Breathing (DB) for vagal activity and Hand Grip (HG) for both vagal activity and peripheral alpha adregneric activity assessement. The alpha-adrenergic activity is assessed through blood pressure variability whereas beta adrenergic activity is assessed through heart rate variability.
Results
Discussion
POTS is one of the most common autonomic diseases. It can be defined as a clinical syndrome lasting at least 6 months that is characterized by an increase in heart rate (HR) ≥30 beats per minute (bpm) within 5 to 10 minutes of orthostatism (or ≥40 bpm in patients 12 to 19 years of age), the absence of orthostatic hypotension (>20 mm Hg decrease in systolic blood pressure) and frequent symptoms that occur with standing such as palpitations, lightheadedness, tremulousness, generalized weakness, blurred vision, exercise intolerance, and fatigue [3]. Several subtypes of POTS were discribed: neuropathic, primary hyperadrenergic, hypovolemic, joint-hypermobility-related, and immune-related [4].
POTS predominates in women with a sex ratio of 4-5: 1 [5]. It usually afflicts young people between 13- to 50-year-old [6]. The POTS typical autonomic profile includes increased beta-adrenergic activity and normal alpha-adrenergic activity. An alpha-adrenergic hyperactivity may be encountered in case of adrenergic receptors dysfunction [7]. Vagal hyperactivity and POTS overlap is possible [8]. In that case, the identification of the autonomic disorder responsible for the symptoms can be difficult [8].
In our study, 66.7% of the subjects were young females. All patients have increased central (normal range ≈ 10%) and peripheral beta-adrenergic activity whereas alpha adrenergic activity was within normal rage (≈ 10%). 10 of 12 had also a vagal hyperactivity on DB (normal range 30 to 50%).
Conclusion
POTS is a common autonomic disorder. Its typical presentation is a young woman with lightheadedness and palpitations occurring in upright position, an increase in HR≥ 30 bpm within 5 to 10 minutes of orthostatism and a normal alpha-adrenergic activity. An overlap with vagal hyperactivity can be observed.
Funding: No funding was received for conducting this study.
Author’s contribution: All authors contributed to the final manuscript.
Competing interests: None of the authors have conflicts of interest.
Compliance with ethical standards.
References
- Rosen S, Cryer P. Postural tachycardia syndrome. The American Journal of Medicine. 1982; 72(5): 847-850.
- Parsaik A, Allison T, Singer W, Sletten D, Joyner M, Benarroch E, et al. Deconditioning in patients with orthostatic intolerance. Neurology. 2012; 79(14): 1435-1439.
- Bryarly M, Phillips L, Fu Q, Vernino S, Levine B. Postural Orthostatic Tachycardia Syndrome. Journal of the American College of Cardiology. 2019; 73(10): 1207-1228.
- Zadourian A, Doherty T, Swiatkiewicz I, Taub P. Postural Orthostatic Tachycardia Syndrome: Prevalence, Pathophysiology, and Management. Drugs. 2018; 78(10): 983-994.
- ROBERTSON D. The Epidemic of Orthostatic Tachycardia and Orthostatic Intolerance. The American Journal of the Medical Sciences. 1999; 317(2): 75-77.
- Garland E, Raj S, Black B, Harris P, Robertson D. The hemodynamic and neurohumoral phenotype of postural tachycardia syndrome. Neurology. 2007; 69(8): 790-798.
- Stewart J. Orthostatic intolerance in pediatrics. The Journal of Pediatrics. 2002; 140(4): 404-411.
- Carew S, Cooke J, O'Connor M, Donnelly T, Costelloe A, Sheehy C et al. What is the optimal duration of tilt testing for the assessment of patients with suspected postural tachycardia syndrome? Europace. 2009; 11(5): 635-637.

