Awake Craniotomy: Asleep-Awake-Asleep Craniotomy: Clinical Case Study
Viera Dorame RF1, Gallo Frias LG2, Pimentel D2, Alejandro Y3, León Velázquez Teresita de J3 and Gabriel MN4*
1Department of Neurosurgery, University of Guadalajara, Mexico
2Social Service, University of Guadalajara Lamar, Mexico
3University of Guadalajara Lamar, Mexico
4Department of Neurology, Hospital Center of the Presidential General Staff, Master’s in Public Health, Doctor in Administration and Public policies, Mexico
Received Date: 04/08/2020; Published Date: 18/08/2020
*Corresponding author: Gabriel Miranda Nava, Department of Neurology, Hospital Center of the Presidential General Staff, Master’s in Public Health, Doctor in Administration and Public policies, Mexico. E-mail: drgabrielmiranda@hotmail.com
Abstract
Observe and evaluate neurological preservation of patient in posterior position for surgical intervention asleep-awake-asleep craniotomy.
Material and Methods: observational, retrospective, longitudinal and descriptive study, considered, as variables are database articles from PubMed and UPTODATE.
Clinical Case Study: The patient is a 57 year old Hispanic male, whom arrives for a neurosurgery consultation at the Regional Military Hospital of Specialties in Guadalajara after presenting an epileptical crisis that initiated in 2013, he was followed up with laboratorial studies and MRI reporting a cerebral tumor located in the frontal right side of the brain. Surgical contentment and space in the operating room (OR) and established to perform surgical resection with biopsy.
Findings: Under anesthesia in asleep-awake-asleep procedure an Oligodendroglioma is found in right frontal side of the brain.
Conclusion: Surgery was not possible due to under capacitated medical equipment and previous preparation to perform asleep-awake-asleep craniotomy.
Keywords: Epileptic Crisis; Biopsy, Resection; Oligodendroglioma; Asleep-Awake-Asleep
Introduction
The oldest finding is with Hippocrates whom performed this procedure in 377-460 A.C [4]. Craniotomy were first implemented to control convulsive crisis by Otfrid Foester and Wilver Penfield whom performed the first surgical intervention at the General Hospital of Massachusetts with the idea of having a cerebral outline, serving for neurological evaluation in precise areas of the brain like motor and sensitive language areas during the procedure to avoid neurological deficiencies posterior to the procedure. Mexico in 2012 performed their first attempt at the hospital Centro Medico Adolfo Lopez Mateos and in 2018 having first realized the asleep-awake-asleep craniotomy [9]. It is of utmost importance to previously evaluate the patient before performing the surgical procedure, must meet certain requirements and characteristics, “the patient must cooperate with the procedure, the patient is required to not present anxiety, somnolence disorientation or aphasia previous to procedure, airway must not be difficult to handle, present chronic pulmonary obstructive disease or obesity” [5]. Tumors are highly vascularized and must be handled with general anesthesia, which makes patient inadequate for this particular surgical procedure. Patient must be at least 10 years of age to be considered a candidate. Patients whom may be intervened are for meningioma, aneurisms, vascular and arteriorvenous malformations or with an affected area considered eloquent.
Methods
The procedure lasts 3-5 hours and must have previous magnetic resonance imagery (MRI) to locate the eloquent cortical areas and the sub cortical white substance tracts. Preoperative psychology counseling is required, anxiolytics with alleviated anxiety which Zolpidem is recommended the previous night of the surgical procedure, if necessary at the time of the procedure the patient should be positioned in supine o lateral. To apply a central venous catheter, Foley or urinary catheter, endotracheal intubation or laryngeal mask the patient must be under general anesthesia and during the craniotomy a neuronavigation system must be utilized for incision.
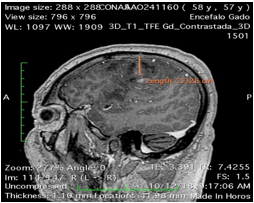
Figure 1: Sagittal cut: Hyperintensive lesion in the frontal right lobule, located in the motor region.
Under general anesthesia and a regional scalp block are utilized to block the auricular-temporal nerve, zygomatic-temporal, supraorbital, supra-trochlear and mayor and minor occipital nerve with 0.5% bupivacaine to perform craniotomy [3]. During the surgical procedure stimulation must be applied with a bipolar and uni cautery in two different points. The pulse stimulation will be 6-10nm and a square wave of 100 ms with repetition in frequencies of 50 Hz having the possibility of a mapping sequence of the superficial cortical area all while consistently checking language and demonstrating images to the patient as well as a sub cortical map previously done [8]. To initiate anesthesia, begin with an intravenous 15mg/kg of Midozolam while in the OR on the operating table in the supine or lateral position, then an infusion must commence with Propofol 75-100mg/kg/min, as well as an infusion Remifentanilo 0.03-0.05 mg/kg/min if available may be switched with Dexametomina [2,6]. General anesthesia must be suspended for 20 minutes before screening the cortical map and electrocorticography, maintaining a level of sedation of three in a modified evaluation of observation in alert/sedation, having the patient respond when spoken to during the cerebral resection of the tumor [1]. The procedure is performed under microscopic view with functional cerebral tests done in real time searching for evident damage to the cortical and sub cortical areas [2]. To finalize the procedure the laryngeal mask is removed, patient follows awake to the Intensive Care Unit (ICU) having constant evaluation posterior to surgical procedure. Having there been multiple risks and complications due to infection or thromboembolism, extra measures of anti-edema must be done during the postoperative and the rest of the intra-hospital stay.
Clinical Case
Patient gave informed signed consent. Masculine, 57 years old, began in 2013 with epileptic crisis’ while at work, which he is then taken to the Regional Military Hospital of Specialties in Guadalajara, having been attended by Neurosurgery an MRI is done immediately demonstrating a cerebral tumor. The patient is given options one being a surgical resection of the tumor and the gold standard treatment. The patient denies the surgical treatment and opts for his conventional treatment of Carbamazepine to control the convulsive crisis. Posterior to the consultation in 2017 he experiences left superior hemiparesis with thermal sensibility accompanied by pain, left dissymmetric alteration of coordination with ataxia in thorax and march altered with lateralization to the left deciding to follow up in October 2018 to be reevaluated by neurosurgery accepting the surgical procedure. Proceeding to blood analyses blood biometry concentrations: anemia with hemoglobin 10.60 g/dL, Hematocrit 33%, Total Leucocytes 17.3x103/uL (94.2% neutrophils). Blood chemistry: Glucose 142 mg/dl, BUN 8.0 mg/dL, and Creatine 0.82 mg/dL. The magnetic resonance imagery (MRI) identifies a heterogeneous mass of 2.9 x 1.8 cm observed in the right cerebral hemisfere characterized by a central region. In T1 imagery the distortion is found to be isointense as for in T2 hypointense. Perilesion edema in the frontal, parietal and temporal lobules.
The surgical procedure is continued applying the sleep-awake-asleep craniotomy technique having resected the tumor in 3.5 hours having the patient posteriorly experience a laryngeal spasm in the process of transoperation which complicated the hemodynamic stability, tachycardia and hypertension, with oxygen saturation decrease bringing together cerebral edema. It’s decided to continue procedure under general anesthesia due to complications previously mentioned then transferring patient to ICU where he presents an increase in convulsive crisis and decrease in the left hemiparesis prolonging his intrahospital stay for 3 days in ICU then transferring to the general hall where he spent another 4 days. It is essential and required to perform this surgical procedure in order to optimize the results and avoid probable complications that may be presented in the future.
Discussion
At the moment of undergoing the surgical procedure for this condition it is recommended to evaluate the size of the tumor and the possibility of performing the resection with a beneficial outcome for the patient, the most common cause of postoperative deficiency is performing an aggressive resection of the tumor and peritumor manipulation, having mutism as a complication. In the case of thee intervened patient did not present neurologic deficiencies posterior to procedure.
There a recent study published by Ari George where he performed 32 craniotomies utilizing the asleep-awake-asleep technique in patients with gliomas which were intervened in eloquent areas having posterior to surgery neurological deficiencies in 3 patients demonstrating beneficial results [1].
According to Harvey-Jumper published in 2015 having followed up on 27 years of experience on resection of gliomas with patients under the asleep-awake-asleep technique which he records 248 surgeries from 1986 -1997 adding 611 surgeries from 1997-2014 with results of 55% high grade and 42% low risk gliomas, 2% with metastasis and 1% with other lesions found with overall few complications and differences between patients with high risk and low risk gliomas [5]. In 2019 an article published by Gerritsen Jkw, in which he performed 37 asleep-awake-asleep craniotomies and 111 craniotomies under general anesthesia demonstrating fewer complications in patients intervened with the asleep-awake-asleep versus general anesthesia craniotomies. The results also proved beneficial for mayor resection of the tumors in patients intervened in asleep-awake-asleep with life expectancy a 5 years postoperational [6,7].
Conclusion
The postoperative conditions of the patient must be evaluated to observe if the patient is an adequate candidate to perform the surgical procedure. Have a multidisciplinary team that can fully operate the equipment and have the equipment necessary available to continue performing with this technique obtaining positive results and search for decreasing mortality and neurologic deficiency.
Acknowledgments
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
References
- Ari G, Santhosh T, Srinivasa B, Roy D, Geeta C, Krishna P, et al. Awake craniotomy and electrophysiological mapping for eloquent area tumours. Clinical Neurology and Neurosurgery. 2013;115:329-334.
- Chui, Jason. Et al. Anestesia para craneotomía en el paciente despierto: una actualización. May 2014. https://www.redalyc.org/pdf/1951/195138949005.pdf.
- Gonzalez, Luis Fernando, Ariza Cadena, Fredy. Senz Ernest. Juan Uribe, Alfonso, Velazquez Fernando. Craneotomia con paciente despierto para resección de tumores cerebrales. April 2009. http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S0120-33472009000100007.
- Lacerda Gallardo, Angel J. Cranietomia Descompresiva en el tratamiento de traumatismo craneoencefálico grave. Marzo de 2012. https://www.medigraphic.com/pdfs/revcubneuro/cnn-2013/cnn131q.pdf.
- Orozco Ramirez, Sergio Manuel, Hernandez Sanchez, Betsu Mayoly, Gonzalez, Alejandro Miranda de Alba Salmeron, Ana Lucia. Tecnica anestésica paciente dormido-despierto para cranectotomia de tumores en áreas funcionales reporte de dos casos. December 2017. https://www.medigraphic.com/pdfs/rma/cma-2017/cma174j.pdf.
- Ramírez E. Anestesia para craneotomía con el paciente despierto: Técnica dormido-despierto-dormido. Medigraphic. 2014;37(1):48-52.
- Shawn H, Jing Li, Darryl L, Molinaro A, David P, Lingzhong M. et al. Awake craniotomy to maximize glioma resection: methods and technical nuances over a 27-year period. J Neurosurg. 2015.
- Tyler B, Ashish S, Amade B, Nirav H. Shah, Thambuswamy M, et al. Awake Craniotomy for Brain Tumor Resection: The Rule Rather Than the Exception? J Neurosurg Anesthesiol. 2013.
- Wan M. The History of Awake Craniotomy in Hospital Universiti Sains MalaysiaMalays J Med Sci. 2013;20(5):67-69.

